Praes. Chassard DDI DC 30MAR09 2 01.Pdf(371
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fasted and Fed State Human Duodenal Fluids: Characterization, Drug Solubility, and Comparison to Simulated Fluids and with Human Bioavailability
European Journal of Pharmaceutics and Biopharmaceutics 163 (2021) 240–251 Contents lists available at ScienceDirect European Journal of Pharmaceutics and Biopharmaceutics journal homepage: www.elsevier.com/locate/ejpb Fasted and fed state human duodenal fluids: Characterization, drug solubility, and comparison to simulated fluids and with human bioavailability D. Dahlgren a, M. Venczel b,c, J.-P. Ridoux b,c, C. Skjold¨ a, A. Müllertz d, R. Holm e, P. Augustijns f, P.M. Hellstrom¨ g, H. Lennernas¨ a,* a Department of Pharmaceutical Biosciences, Biopharmaceutics, Uppsala University, Sweden b Global CMC Development Sanofi, Frankfurt, Germany c Global CMC Development Sanofi, Vitry, France d Physiological Pharmaceutics, University of Copenhagen, Copenhagen, Denmark e Drug Product Development, Janssen R&D, Johnson & Johnson, Beerse, Belgium f Drug Delivery and Disposition, KU Leuven, Leuven, Belgium g Department of Medical Sciences, Gastroenterology/Hepatology, Uppsala University, Sweden ARTICLE INFO ABSTRACT Keywords: Accurate in vivo predictions of intestinal absorption of low solubility drugs require knowing their solubility in Bioavailability physiologically relevant dissolution media. Aspirated human intestinal fluids (HIF) are the gold standard, fol Food effects lowed by simulated intestinal HIF in the fasted and fed state (FaSSIF/FeSSIF). However, current HIF charac Drug solubility terization data vary, and there is also some controversy regarding the accuracy of FaSSIF and FeSSIF for Human intestinal fluids predicting drug solubility in HIF. This study aimed at characterizing fasted and fed state duodenal HIF from 16 Drug absorption Drug dissolution human volunteers with respect to pH, buffer capacity, osmolarity, surface tension, as well as protein, phos Drug delivery pholipid, and bile salt content. -

Pharmacokinetic Interactions of Pioglitazone
Department of Clinical Pharmacology University of Helsinki Finland PHARMACOKINETIC INTERACTIONS OF PIOGLITAZONE Tiina Jaakkola ACADEMIC DISSERTATION To be presented, with the permission of the Medical Faculty of the University of Helsinki, for public examination in Auditorium 2 of Biomedicum, on August 24th, 2007, at 12 noon. Helsinki 2007 JJaakkola_Tiina_vaitos.inddaakkola_Tiina_vaitos.indd 1 117.7.20077.7.2007 221:11:231:11:23 Supervisors: Professor Pertti Neuvonen, MD Department of Clinical Pharmacology University of Helsinki Helsinki, Finland Docent Janne Backman, MD Department of Clinical Pharmacology University of Helsinki Helsinki, Finland Reviewers: Docent Kimmo Malminiemi, MD, MSc Department of Pharmacology, Clinical Pharmacology and Toxicology University of Tampere Tampere, Finland Professor emeritus Pertti Pentikäinen, MD Department of Medicine University of Helsinki Helsinki, Finland Opponent: Professor Kari Kivistö, MD Department of Pharmacology, Clinical Pharmacology and Toxicology University of Tampere Tampere, Finland ISBN 978-952-92-2224-7 (paperback) ISBN 978-952-10-4020-7 (PDF, http://ethesis.helsinki.fi ) Helsinki 2007 Yliopistopaino JJaakkola_Tiina_vaitos.inddaakkola_Tiina_vaitos.indd 2 117.7.20077.7.2007 221:11:551:11:55 JJaakkola_Tiina_vaitos.inddaakkola_Tiina_vaitos.indd 3 117.7.20077.7.2007 221:11:551:11:55 CONTENTS CONTENTS ABBREVIATIONS.......................................................................................................................................... 6 LIST OF ORIGINAL PUBLICATIONS....................................................................................................... -

Pharmacokinetic Interactions of Drugs with St John's Wort
http://www.paper.edu.cn Pharmacokinetic interactions of Journal of Psychopharmacology 18(2) (2004) 262–276 © 2004 British Association drugs with St John’s wort for Psychopharmacology ISSN 0269-8811 SAGE Publications Ltd, London, Thousand Oaks, CA and New Delhi 10.1177/0269881104042632 Shufeng Zhou Department of Pharmacy, Faculty of Science, National University of Singapore, Singapore. Eli Chan Department of Pharmacy, Faculty of Science, National University of Singapore, Singapore. Shen-Quan Pan Department of Biological Sciences, Faculty of Science, National University of Singapore, Singapore. Min Huang Institute of Clinical Pharmacology, School of Pharmaceutical Sciences, Sun Yat-Sen University, Guangzhou 510089, PR China. Edmund Jon Deoon Lee Department of Pharmacology, Faculty of Medicine, National University of Singapore, Singapore. Abstract There is a worldwide increasing use of herbs which are often cancer patients receiving irinotecan treatment. St John’s wort did not administered in combination with therapeutic drugs, raising the alter the pharmacokinetics of tolbutamide, but increased the incidence potential for herb–drug interactions. St John’s wort (Hypericum of hypoglycaemia. Several cases have been reported that St John’s wort perforatum) is one of the most commonly used herbal antidepressants. A decreased cyclosporine blood concentration leading to organ rejection. literature search was performed using Medline (via Pubmed), Biological St John’s wort caused breakthrough bleeding and unplanned pregnancies Abstracts, Cochrane Library, AMED, PsycINFO and Embase (all from their when used concomitantly with oral contraceptives. It also caused inception to September 2003) to identify known drug interaction with serotonin syndrome when coadministered with selective serotonin- St John’s wort. The available data indicate that St John’s wort is a reuptake inhibitors (e.g. -

Kriya Sharir of Kesh
Aayushi International Interdisciplinary Research Journal (AIIRJ) PEER REVIEW IMPACT FACTOR ISSN VOL- VI ISSUE-XI NOVEMBER 2019 e-JOURNAL 5.707 2349-638x A Review study -Kriya sharir of Kesh Dr. Pooja Pandurang Patil MD (Kriya Sharir) Assistant Professor B.G. Garaiya Ayurveda College Rajkot (Gujarat) Abstract: Health comprises of both, body and mind. Ayurveda aims at maintaining the health of a healthy person and to treat the diseased. Scalp hair is responsible for beauty, appearance of personality and protection. “The hair is the richest ornament of a woman”- Martin Luther. It brings one’s self-image into focus. There are an increasing number of panicked people coming to the doctor with the complaint of hair loss. Due to modern lifestyle, food, environment etc, people are more likely to lose hair at early age. Therefore more awareness about hair health is observed in the society. This article mentions the possible ways of enhancement of strength and beauty of scalp hair through the principles of achieving good health (Swasthy Prapti) as explained in Ayurveda. The scope of this article deals with understanding of all aspects of Kesha mentioned in the Samhitas of Ayurveda. Key words: Kesh, Kesha Swasthya, Beauty Introduction found to be more promising and result oriented with absolute no drawbacks. Ayurveda is an ancient and developed science of In Ayurveda, scattered references are India. Kesha (hair) is a complex and delicate part of available on maintaining the health and longevity of our body, which gives a personality. Beautification is hair. It has explained few concepts for achieving the process of making visual improvements to a good health. -

Girl Scout Trailblazers Guidelines
GIRL SCOUT TRAILBLAZERS Twenty-First Century Guidelines CONTENTS 3 Preface 3 How to Use This Toolkit 3 A Note to the Reader 4 Introduction 4 Why Girl Scout Trailblazers, Why Now? 4 What Is the Girl Scout Trailblazer Program? 5 Who Can Become a Trailblazer? 6 Interview with a Trailblazer 7 Are You Ready for a Trailblazer Program at Your Council? 10 Girl Scout Trailblazer Program 10 The Foundational Girl Scout Experience, Trailblazer Style 10 The Girl Scout Leadership Experience 10 The Three Girl Scout Processes 11 Take Action 11 Awards 11 Trips and travel 12 Product program 12 Girl Scout traditions 12 The Trailblazer uniform 12 Volunteers 13 Progression Within Trailblazer Troops 14 Trailblazer Events 15 Her Trailblazer Experience 15 Girl Scout Trailblazer Pin 15 Trailblazer Concentrations 16 Hiking 16 Stewardship 16 Adventure Sport 17 Camping 17 Survivorship 18 Learning by Doing 18 Trailblazer skill areas 18 Badges 21 Journeys 21 Highest awards 21 Take Action projects 22 Career exploration 22 Product program 22 Girl Scout traditions 23 Appendixes 23 Appendix A—GSUSA Outdoor Progression Model 24 Appendix B—Trailblazer Skill Development Areas 31 Appendix C—Tips for Adults Supporting Girls in the Outdoors 34 Appendix D—Resources GIRL SCOUT TRAILBLAZERS Twenty-First Century Guidelines Preface How to Use This Toolkit The audience for these guidelines is councils and their volunteers. The introduction provides an overview and direction to council staff for assessing, planning, and activating troops. Parts 2 and 3 speak to council staff and volunteers as they compose their troops and work with them to define the Trailblazer experience. -

NINDS Custom Collection II
ACACETIN ACEBUTOLOL HYDROCHLORIDE ACECLIDINE HYDROCHLORIDE ACEMETACIN ACETAMINOPHEN ACETAMINOSALOL ACETANILIDE ACETARSOL ACETAZOLAMIDE ACETOHYDROXAMIC ACID ACETRIAZOIC ACID ACETYL TYROSINE ETHYL ESTER ACETYLCARNITINE ACETYLCHOLINE ACETYLCYSTEINE ACETYLGLUCOSAMINE ACETYLGLUTAMIC ACID ACETYL-L-LEUCINE ACETYLPHENYLALANINE ACETYLSEROTONIN ACETYLTRYPTOPHAN ACEXAMIC ACID ACIVICIN ACLACINOMYCIN A1 ACONITINE ACRIFLAVINIUM HYDROCHLORIDE ACRISORCIN ACTINONIN ACYCLOVIR ADENOSINE PHOSPHATE ADENOSINE ADRENALINE BITARTRATE AESCULIN AJMALINE AKLAVINE HYDROCHLORIDE ALANYL-dl-LEUCINE ALANYL-dl-PHENYLALANINE ALAPROCLATE ALBENDAZOLE ALBUTEROL ALEXIDINE HYDROCHLORIDE ALLANTOIN ALLOPURINOL ALMOTRIPTAN ALOIN ALPRENOLOL ALTRETAMINE ALVERINE CITRATE AMANTADINE HYDROCHLORIDE AMBROXOL HYDROCHLORIDE AMCINONIDE AMIKACIN SULFATE AMILORIDE HYDROCHLORIDE 3-AMINOBENZAMIDE gamma-AMINOBUTYRIC ACID AMINOCAPROIC ACID N- (2-AMINOETHYL)-4-CHLOROBENZAMIDE (RO-16-6491) AMINOGLUTETHIMIDE AMINOHIPPURIC ACID AMINOHYDROXYBUTYRIC ACID AMINOLEVULINIC ACID HYDROCHLORIDE AMINOPHENAZONE 3-AMINOPROPANESULPHONIC ACID AMINOPYRIDINE 9-AMINO-1,2,3,4-TETRAHYDROACRIDINE HYDROCHLORIDE AMINOTHIAZOLE AMIODARONE HYDROCHLORIDE AMIPRILOSE AMITRIPTYLINE HYDROCHLORIDE AMLODIPINE BESYLATE AMODIAQUINE DIHYDROCHLORIDE AMOXEPINE AMOXICILLIN AMPICILLIN SODIUM AMPROLIUM AMRINONE AMYGDALIN ANABASAMINE HYDROCHLORIDE ANABASINE HYDROCHLORIDE ANCITABINE HYDROCHLORIDE ANDROSTERONE SODIUM SULFATE ANIRACETAM ANISINDIONE ANISODAMINE ANISOMYCIN ANTAZOLINE PHOSPHATE ANTHRALIN ANTIMYCIN A (A1 shown) ANTIPYRINE APHYLLIC -
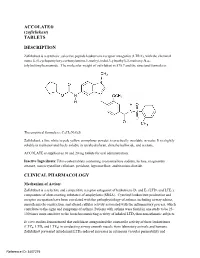
ACCOLATE® (Zafirlukast) TABLETS DESCRIPTION
ACCOLATE® (zafirlukast) TABLETS DESCRIPTION Zafirlukast is a synthetic, selective peptide leukotriene receptor antagonist (LTRA), with the chemical name 4-(5-cyclopentyloxy-carbonylamino-1-methyl-indol-3-ylmethyl)-3-methoxy-N-o tolylsulfonylbenzamide. The molecular weight of zafirlukast is 575.7 and the structural formula is: The empirical formula is: C31H33N3O6S Zafirlukast, a fine white to pale yellow amorphous powder, is practically insoluble in water. It is slightly soluble in methanol and freely soluble in tetrahydrofuran, dimethylsulfoxide, and acetone. ACCOLATE is supplied as 10 and 20 mg tablets for oral administration. Inactive Ingredients: Film-coated tablets containing croscarmellose sodium, lactose, magnesium stearate, microcrystalline cellulose, povidone, hypromellose, and titanium dioxide. CLINICAL PHARMACOLOGY Mechanism of Action: Zafirlukast is a selective and competitive receptor antagonist of leukotriene D4 and E4 (LTD4 and LTE4), components of slow-reacting substance of anaphylaxis (SRSA). Cysteinyl leukotriene production and receptor occupation have been correlated with the pathophysiology of asthma, including airway edema, smooth muscle constriction, and altered cellular activity associated with the inflammatory process, which contribute to the signs and symptoms of asthma. Patients with asthma were found in one study to be 25 100 times more sensitive to the bronchoconstricting activity of inhaled LTD4 than nonasthmatic subjects. In vitro studies demonstrated that zafirlukast antagonized the contractile activity of three leukotrienes (LTC4, LTD4 and LTE4) in conducting airway smooth muscle from laboratory animals and humans. Zafirlukast prevented intradermal LTD4-induced increases in cutaneous vascular permeability and Reference ID: 3407275 inhibited inhaled LTD4-induced influx of eosinophils into animal lungs. Inhalational challenge studies in sensitized sheep showed that zafirlukast suppressed the airway responses to antigen; this included both the early- and late-phase response and the nonspecific hyperresponsiveness. -

How the Brain Forms New Habits: Why Willpower Is Not Enough
How The Brain Forms New Habits: Why Willpower Is Not Enough Presented by George F. Koob, Ph.D. Disclosure Neither Dr. George F. Koob, the presenting speaker, nor the activity planners of this program are aware of any actual, potential or perceived conflict of interest Sponsored by Institute for Brain Potential PO Box 1127 KnrA`mnr, B@82524 COURSE OBJECTIVES Participants completing the program should be able to: 1) Name several characteristics of reward-centered habits. 2) Identify several evidence-based strategies for managing reward-centered habits. 3) Describe how threat-based mental habits are connected to maladaptive emotions and actions. 4) List one or more strategies for coping adaptively with threat-based mental habits. 5) Identify several evidence-based principles for initiating and maintaining health- promoting habits. Policies and Procedures 1. Questions are encouraged. However, please try to ask questions related to the topic being discussed. You may ask your question by clicking on “chat.” Your questions will be communicated to the presenter during the breaks. Dr. Koob will be providing registrants with information as to how to reach him by email for questions after the day of the live broadcast. 2. If you enjoyed this lecture and wish to recommend it to a friend or colleague, please feel free to invite your associates to call our registration division at 866-652-7414 or visit our website at www.IBPceu.com to register for a rebroadcast of the program or to purchase a copy of the DVD. 3. If you are unable to view the live web broadcast, you have two options: a) You may elect to download the webinar through February 28 th , 2014. -

The Elimination of High Doses of Phenytoin In
THE ELIMINATION OF HIGH DOSES OF PHENYTOIN IN MAN AND THE RABBIT by Peter Chinwah Department of Clinical Pharmacology St. Vincent's Hospital Darlinghurst, 2010, N.S.W. AUSTRALIA A Thesis submitted for the Degree of Master of Science in the University of New South Wales February, 1987 Ul·lilJ:2?.S1TY QF N.S.W. ~ 14 JUN 1988 f L!.:.": --":c_A:_'''"lARY I (i) ACKNOWLEDGEMENTS I wish to thank Professor Denis Wade for the opportunity to undertake this thesis in the Department of Clinical Pharmacology and for his overseeing and supervision of this project. I would like to express my gratitude to Dr Garry Graham, Senior Lecturer in the Department of Physiology and Pharmacology at the University of New South Wales, for his significant contribution in discussion and critical review of this thesis. I also wish to thank my colleagues of the Department of Clinical Pharmacology and Toxicology at St Vincent's Hospital for their assistance during the course of the project. Finally, I am grateful to Dr Ken Williams of the Department of Clinical Pharmacology and Toxicology at St Vincent's Hospital for many hours of discussion, and his admonishment, long suffering and perserverence which have made this thesis possible. (ii) ABSTRACT The pharmacokinetics of phenytoin were studied in twelve patients who presented to casualty with phenytoin toxicity. These patients were divided into 3 groups according to the type of plasma elimination profiles observed. Group 1. consisted of 3 patients who demonstrated first order elimination kinetics with long elimination half lives (70-106 hours). Group 2. consisted of 6 patients who showed saturable elimination kinetics (mean estimated terminal half life 28 hours). -

By Dagmar Schultz AUDRE LORDE – HER STRUGGLES and HER Visionsi in This Presentation I Will Try to Explain How Audre Lorde Came
By Dagmar Schultz AUDRE LORDE – HER STRUGGLES AND HER VISIONSi In this presentation I will try to explain how Audre Lorde came to Germany, what she meant to me personally and to Orlanda Women’s Publishers, and what effect her work had in Germany on Black and white women. In 1980, I met Audre Lorde for the first time at the UN World Women’s Conference in Copenhagen in a discussion following her reading. I knew nothing about her then, nor was I familiar with her books. I was spellbound and very much impressed with the openness with which Audre Lorde addressed us white women. She told us about the importance of her work as a poet, about racism and differences among women, about women in Europe, the USA and South Africa, and stressed the need for a vision of the future to guide our political praxis. On that evening it became clear to me: Audre Lorde must come to Germany for German women to hear her, her voice speaking to white women in an era when the movement had begun to show reactionary tendencies. She would help to pull it out of its provinciality, its over-reliance, in its politics, on the exclusive experience of white women. At that time I was teaching at the Free University of Berlin and thus had the opportunity to invite Audre Lorde to be a guest professor. In the spring of 1984 she agreed to come to Berlin for a semester to teach literature and creative writing. Earlier, in 1981, I had heard Audre Lorde and Jewish poet Adrienne Rich speaking about racism and antisemitism at the National Women’s Studies Association annual convention. -
Student-Centered Learning: Life Academy of Health and Bioscience
Stanford Center for Opportunity Policy in Education Student-Centered Learning: Life Academy of Health and Bioscience By Nikole Richardson and Joe Feldman sco e Stanford Center for Opportunity Policy in Education Student-Centered Learning: Life Academy of Health and Bioscience i Suggested citation: Richardson, N., & Feldman, J. (2014). Student-centered learning: Life Academy of Health and Bioscience. Stanford, CA: Stanford Center for Opportunity Policy in Education. Portions of this document may be reprinted with permission from the Stanford Center for Opportunity Policy in Education (SCOPE). To reprint, please use the following language: “Printed with permission, Stanford Center for Opportunity Policy in Education. http://edpolicy.stanford.edu.” For more information, contact us at [email protected]. This work is made possible through generous support from the Nellie Mae Education Foundation. Stanford Center for Opportunity Policy in Education Stanford, California • 650.725.8600 • [email protected] http://edpolicy.stanford.edu @scope_stanford sco e Stanford Center for Opportunity Policy in Education Table of Contents Overview ......................................................................................................................... i Introduction ................................................................................................................... 1 School Description and Outcomes ................................................................................. 3 Personalization .............................................................................................................. -

Physical Arrangement of the Classroom Students
Physical Arrangement of COMPONENT the Classroom 1 Objective: To explain how the physical arrange- ment of your classroom impacts the success of your COMPONENT 1 Physical Arrangement of the Classroom students. COMPONENT 2 THINKING TRAPS Organization of Materials “Why go to all the trouble of arranging my room just so?” “I like my students to work wherever COMPONENT 3 they feel comfortable.” Schedules “I don’t have enough furniture or space to make special areas in my classroom.” COMPONENT 4 Visual Strategies COMPONENT 5 Behavioral Strategies COMPONENT 6 Goals, Objectives, and Lesson Plans e often hear these comments as we begin to COMPONENT 7 W assist teachers in arranging their classrooms, Instructional Strategies and we acknowledge that these are valid concerns. We also know that physically arranging a classroom is very hard physical labor! Finding the right type of furniture COMPONENT 8 and enough furniture is challenging as well. No mat- Communication Systems and Strategies ter how difficult this task of physically arranging your classroom may appear, we recommend that you do it COMPONENT 9 before you attempt to address any of the other com- Communication With Parents ponents. It will make implementing the other compo- nents easier once the physical space is clearly defined. The classroom arrangement is the physical foundation COMPONENT 10 Related Services and Other School Staff for the 10 critical components. 6 • 10 Critical Components RATIONALE In a well-designed special education classroom, the classroom activities that are to take place and the needs of the students must be considered when planning the arrangement of the classroom furniture and where instructional areas will be located.