Specific Binding of Human Corticosteroid-Binding Globulin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

This Fact Sheet Provides Information to Patients with Eczema and Their Carers. About Topical Corticosteroids How to Apply Topic
This fact sheet provides information to patients with eczema and their carers. About topical corticosteroids You or your child’s doctor has prescribed a topical corticosteroid for the treatment of eczema. For treating eczema, corticosteroids are usually prepared in a cream or ointment and are applied topically (directly onto the skin). Topical corticosteroids work by reducing inflammation and helping to control an over-reactive response of the immune system at the site of eczema. They also tighten blood vessels, making less blood flow to the surface of the skin. Together, these effects help to manage the symptoms of eczema. There is a range of steroids that can be used to treat eczema, each with different strengths (potencies). On the next page, the potencies of some common steroids are shown, as well as the concentration that they are usually used in cream or ointment preparations. Using a moisturiser along with a steroid cream does not reduce the effect of the steroid. There are many misconceptions about the side effects of topical corticosteroids. However these treatments are very safe and patients are encouraged to follow the treatment regimen as advised by their doctor. How to apply topical corticosteroids How often should I apply? How much should I apply? Apply 1–2 times each day to the affected area Enough cream should be used so that the of skin according to your doctor’s instructions. entire affected area is covered. The cream can then be rubbed or massaged into the Once the steroid cream has been applied, inflamed skin. moisturisers can be used straight away if needed. -

Steroid Use in Prednisone Allergy Abby Shuck, Pharmd Candidate
Steroid Use in Prednisone Allergy Abby Shuck, PharmD candidate 2015 University of Findlay If a patient has an allergy to prednisone and methylprednisolone, what (if any) other corticosteroid can the patient use to avoid an allergic reaction? Corticosteroids very rarely cause allergic reactions in patients that receive them. Since corticosteroids are typically used to treat severe allergic reactions and anaphylaxis, it seems unlikely that these drugs could actually induce an allergic reaction of their own. However, between 0.5-5% of people have reported any sort of reaction to a corticosteroid that they have received.1 Corticosteroids can cause anything from minor skin irritations to full blown anaphylactic shock. Worsening of allergic symptoms during corticosteroid treatment may not always mean that the patient has failed treatment, although it may appear to be so.2,3 There are essentially four classes of corticosteroids: Class A, hydrocortisone-type, Class B, triamcinolone acetonide type, Class C, betamethasone type, and Class D, hydrocortisone-17-butyrate and clobetasone-17-butyrate type. Major* corticosteroids in Class A include cortisone, hydrocortisone, methylprednisolone, prednisolone, and prednisone. Major* corticosteroids in Class B include budesonide, fluocinolone, and triamcinolone. Major* corticosteroids in Class C include beclomethasone and dexamethasone. Finally, major* corticosteroids in Class D include betamethasone, fluticasone, and mometasone.4,5 Class D was later subdivided into Class D1 and D2 depending on the presence or 5,6 absence of a C16 methyl substitution and/or halogenation on C9 of the steroid B-ring. It is often hard to determine what exactly a patient is allergic to if they experience a reaction to a corticosteroid. -

The Effects of Dehydroepiandrosterone Sulfate on Counterregulatory Responses During Repeated Hypoglycemia in Conscious Normal Rats Darleen A
The Effects of Dehydroepiandrosterone Sulfate on Counterregulatory Responses During Repeated Hypoglycemia in Conscious Normal Rats Darleen A. Sandoval, Ling Ping, Ray Anthony Neill, Sachiko Morrey, and Stephen N. Davis ⅐ ؊1 ⅐ ؊1 We previously determined that both antecedent hy- mol/l kg min ; P < 0.05). In summary, day-1 poglycemia and elevated cortisol levels blunt neu- antecedent hypoglycemia blunted neuroendocrine and roendocrine and metabolic responses to subsequent metabolic responses to next-day hypoglycemia. How- hypoglycemia in conscious, unrestrained rats. The adre- ever, simultaneous DHEA-S infusion during antecedent nal steroid dehydroepiandrosterone sulfate (DHEA-S) hypoglycemia preserved neuroendocrine and metabolic has been shown in several studies to oppose corticoste- counterregulatory responses during subsequent hypo- roid action. The purpose of this study was to determine glycemia in conscious rats. Diabetes 53:679–686, 2004 if DHEA-S could preserve counterregulatory responses during repeated hypoglycemia. We studied 40 male Sprague-Dawley rats during a series of 2-day protocols. he Diabetes Control and Complications Trial Day 1 consisted of two 2-h episodes of 1) hyperinsuline- mic (30 pmol ⅐ kg؊1 ⅐ min؊1) euglycemia (6.2 ؎ 0.2 established that intensive glucose control in type ANTE EUG), 2) hyperinsulinemic eug- 1 diabetic patients can slow the progression or ;12 ؍ mmol/l; n -plus simultaneous Tsignificantly reduce the onset of diabetic micro (8 ؍ lycemia (6.0 ؎ 0.1 mmol/l; n intravenous infusion of DHEA-S (30 mg/kg; ANTE EUG vascular complications (e.g., retinopathy, nephropathy, ؉ DHEA-S), 3) hyperinsulinemic hypoglycemia (2.8 ؎ neuropathy) (1). Unfortunately, the study also established ANTE HYPO), or 4) hyperinsulinemic that intensive glucose treatment causes an approximate ;12 ؍ mmol/l; n 0.1 -with simulta- threefold increase in the frequency of severe hypoglyce (8 ؍ hypoglycemia (2.8 ؎ 0.1 mmol/l; n neous intravenous infusion of DHEA-S (30 mg/kg; ANTE mia (2). -

Inhaled and Oral Corticosteroids
Inhaled and Oral Corticosteroids Corticosteroids (steroids) are medicines that are used to treat many chronic diseases. Corticosteroids are very good at reducing inflammation (swelling) and mucus production in the airways of the lungs. They also help other quick-relief medicines work better. The steroids (corticosteroids) used to treat asthma and other chronic lung diseases are not the same as anabolic steroids, used illegally by some athletes for bodybuilding. Corticosteroids do not affect the liver or cause sterility. Does the Body Make Steroids? Corticosteroids are similar to cortisol, a hormone produced by the adrenal glands in the body. Cortisol is one of the body's own natural steroids. Cortisol is essential for life and well being. During stress, our bodies produce extra cortisol to keep us from becoming very sick. Normally the adrenal glands release cortisol into the blood stream every morning. The brain monitors this amount and regulates the adrenal function. It cannot tell the difference between its own natural cortisone and that of steroid medicines. Therefore, when a person takes high doses of steroids over a long time, the brain may decrease or stop cortisol production. This is called adrenal supression. Health care providers generally decrease a steroid dosage slowly to allow the adrenal gland to recover and produce cortisol at a normal level again. If you have been on steroids long- term do not stop taking them suddenly. Follow your doctor’s prescription. What are Some Steroid Medicines? Steroid medicines are available as nasal sprays, metered- dose-inhalers (inhaled steroids), oral forms (pills or syrups), injections into the muscle (shots) and intravenous (IV) solutions. -

Pharmacologic Characteristics of Corticosteroids 대한신경집중치료학회
REVIEW J Neurocrit Care 2017;10(2):53-59 https://doi.org/10.18700/jnc.170035 eISSN 2508-1349 Pharmacologic Characteristics of Corticosteroids 대한신경집중치료학회 Sophie Samuel, PharmD1, Thuy Nguyen, PharmD1, H. Alex Choi, MD2 1Department of Pharmacy, Memorial Hermann Texas Medical Center, Houston, TX; 2Department of Neurosurgery and Neurology, The University of Texas Medical School at Houston, Houston, TX, USA Corticosteroids (CSs) are used frequently in the neurocritical care unit mainly for their anti- Received December 7, 2017 inflammatory and immunosuppressive effects. Despite their broad use, limited evidence Revised December 7, 2017 exists for their efficacy in diseases confronted in the neurocritical care setting. There are Accepted December 17, 2017 considerable safety concerns associated with administering these drugs and should be limited Corresponding Author: to specific conditions in which their benefits outweigh the risks. The application of CSs in H. Alex Choi, MD neurologic diseases, range from traumatic head and spinal cord injuries to central nervous Department of Pharmacy, Memorial system infections. Based on animal studies, it is speculated that the benefit of CSs therapy Hermann Texas Medical Center, 6411 in brain and spinal cord, include neuroprotection from free radicals, specifically when given Fannin Street, Houston, TX 77030, at a higher supraphysiologic doses. Regardless of these advantages and promising results in USA animal studies, clinical trials have failed to show a significant benefit of CSs administration Tel: +1-713-500-6128 on neurologic outcomes or mortality in patients with head and acute spinal injuries. This Fax: +1-713-500-0665 article reviews various chemical structures between natural and synthetic steroids, discuss its E-mail: [email protected] pharmacokinetic and pharmacodynamic profiles, and describe their use in clinical practice. -
17-Hydroxyprogesterone
17-Hydroxyprogesterone 1 Name and description of analyte 1.1 Name of analyte 17-Hydroxyprogesterone (17-OHP). 1.2 Alternative names 17α-hydroxyprogesterone, 17-OH progesterone, 17-hydroxypregn-4-ene-3,20-dione. 1.3 NLMC code (to follow) 1.4 Description of analyte 17-Hydroxyprogesterone (C21H30O3; MW = 330.46 Da) is an endogenous progestogen produced from 17-hydroxypregnenolone and progesterone through the actions of 3β-hydroxysteroid dehydrogenase and 17-hydroxylase, respectively. 17-OHP synthesis is stimulated by pituitary adrenocorticotrophic hormone (ACTH) as part of the hypothalamic–pituitary–adrenal (HPA) axis. 1.5 Function(s) of analyte 17-Hydroxyprogesterone is primarily produced within the zona fasciculata of the adrenal cortex; however, it can also be produced by the corpus luteum, gonads, and placenta. 17-OHP is an intermediate in the production of cortisol in the zona fasciculata, and an intermediate in the production of adrenal androgens in the zona reticularis (via 17,20 lyase) and 17α- hydroxyallopregnanolone (via 5α-reductase). In addition, 17-OHP is a relatively weak agonist of the progesterone receptor, a partial agonist of the glucocorticoid receptor, and an antagonist of the mineralocorticoid receptor. 2 Sample requirements and precautions 2.1 Medium in which measured 17-hydroxyprogesterone is predominantly measured in serum or EDTA or heparinised plasma; however, saliva, hair, and dried blood spot measurements can also be performed. 2.2 Precautions re: sampling, handling etc. Concomitant corticosteroid treatment can suppress 17-OHP. Serum and plasma samples should be separated upon receipt. Saliva samples should be frozen to precipitate salivary glycoproteins. Neonatal samples for the diagnosis of suspected congenital adrenal hyperplasia (CAH) should be taken prior to the administration of exogenous corticosteroids (where possible). -

11-Deoxycortisol Is a Corticosteroid Hormone in the Lamprey
11-Deoxycortisol is a corticosteroid hormone in the lamprey David A. Closea,b,1,2, Sang-Seon Yuna,3, Stephen D. McCormickc, Andrew J. Wildbilla, and Weiming Lia,1 aDepartment of Fisheries and Wildlife, Michigan State University, East Lansing, MI 48824; bDepartment of Natural Resources, Confederated Tribes of the Umatilla Indian Reservation, Pendleton, OR 97801; and cUS Geological Survey, Conte Anadromous Fish Research Center, Turner Falls, MA 01376 Edited* by Jan-Åke Gustafsson, Karolinska Institutet, Huddinge, Sweden, and approved June 18, 2010 (received for review December 8, 2009) Corticosteroid hormones are critical for controlling metabolism, assay using the ligand binding domain (LBD) of lamprey CR fused hydromineral balance, and the stress response in vertebrates. with a mammalian GAL4-DBD (6). To better understand the evo- Although corticosteroid hormones have been well characterized in lution of CRs, Stolte et al. (7) performed phylogenetic analysis using most vertebrate groups, the identity of the earliest vertebrate the lamprey CR. Their findings showed that the gene clustered with corticosteroid hormone has remained elusive. Here we provide extant MR genes, suggesting that an MC complex evolved first. evidence that 11-deoxycortisol is the corticosteroid hormone in the Because aldosterone was not found at physiologically relevant levels lamprey, a member of the agnathans that evolved more than 500 in the lamprey (6), receptor sensitivity to aldosterone was suggested million years ago. We used RIA, HPLC, and mass spectrometry to be a by-product of sensitivity to 11-deoxycorticosterone, a postu- analysis to determine that 11-deoxycortisol is the active corticoste- lated ancestral hormone (8). Notably lacking, however, have been roid present in lamprey plasma. -

Corticosterone Concentrations in Blood and Excretion in Faeces After ACTH Administration in Male Sprague-Dawley Rats
in vivo 22 : 435-440 (2008) Corticosterone Concentrations in Blood and Excretion in Faeces after ACTH Administration in Male Sprague-Dawley Rats HARRY SISWANTO 1, JANN HAU 1,2 , HANS-ERIK CARLSSON 1, RENÉE GOLDKUHL 1 and KLAS S.P. ABELSON 1 1Division of Comparative Medicine, Department of Neuroscience, Biomedical Centre, Uppsala University, Uppsala, Sweden; 2Department of Experimental Medicine, University of Copenhagen and National Hospital, Copenhagen, Denmark Abstract. The aim of the present study was to analyse the homeostatic mechanisms of the body, including the immune, corticosterone response to exogenous ACTH in the the endocrine, and the reproductive systems (3-5). Stress is circulation of catheterised male rats and to investigate the therefore generally acknowledged not only as a confounding sensitivity of faecal corticosterone output as a measure of variable in experimental results, but also as a major cause of preceding elevated levels in the circulation. A total of 21 suffering in laboratory animals. Refinement of stressful adult male Sprague-Dawley rats permanently catheterised (v. procedures to which laboratory animals are subjected is jugularis externa for intravenous administration of ACTH therefore essential. In order to achieve this, development of and a. carotis communis for blood sampling), were used. adequate objective methods for the assessment and Administration of both 10 and 100 μg/kg ACTH resulted in a recognition of stress in laboratory animals is a major rapid and pronounced corticosterone increase three minutes challenge in biomedical research. Stress can be assessed by after injection (226 and 220 ng/ml, respectively), but the quantifying different endogenous stress markers, of which duration of the response was different. -
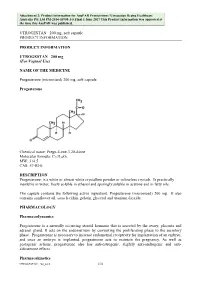
Attachment 2. Product Information for Progesterone
Attachment 2: Product information for AusPAR Prometrium / Utrogestan Besins Healthcare Australia Pty Ltd PM-2014-03908-1-5 Final 1 June 2017 This Product Information was approved at the time this AusPAR was published. UTROGESTAN 200 mg, soft capsule PRODUCT INFORMATION PRODUCT INFORMATION UTROGESTAN 200 mg (For Vaginal Use) NAME OF THE MEDICINE Progesterone (micronised) 200 mg, soft capsule Progesterone Chemical name: Pregn-4-ene-3,20-dione Molecular formula: C21H30O2. MW: 314.5 CAS: 57-83-0. DESCRIPTION Progesterone: is a white or almost white crystalline powder or colourless crystals. Is practically insoluble in water, freely soluble in ethanol and sparingly soluble in acetone and in fatty oils. The capsule contains the following active ingredient: Progesterone (micronised) 200 mg. It also contains sunflower oil, soya lecithin, gelatin, glycerol and titanium dioxide. PHARMACOLOGY Pharmacodynamics Progesterone is a naturally occurring steroid hormone that is secreted by the ovary, placenta and adrenal gland. It acts on the endometrium by converting the proliferating phase to the secretory phase. Progesterone is necessary to increase endometrial receptivity for implantation of an embryo, and once an embryo is implanted, progesterone acts to maintain the pregnancy. As well as gestagenic actions, progesterone also has anti-estrogenic, slightly anti-androgenic and anti- aldosterone effects. Pharmacokinetics UTROGESTAN 200_0416 1/10 Attachment 2: Product information for AusPAR Prometrium / Utrogestan Besins Healthcare Australia Pty Ltd PM-2014-03908-1-5 Final 1 June 2017 This Product Information was approved at the time this AusPAR was published. UTROGESTAN 200 mg, soft capsule PRODUCT INFORMATION Absorption Following oral administration, micronised progesterone is absorbed by the digestive tract. -

Dehydroepiandrosterone Sulfate and Dehydroepiandrosterone Sulfate/Cortisol Ratio in Cirrhotic Patients with Septic Shock: Anothe
Tsai et al. Critical Care (2017) 21:214 DOI 10.1186/s13054-017-1768-0 RESEARCH Open Access Dehydroepiandrosterone sulfate and dehydroepiandrosterone sulfate/cortisol ratio in cirrhotic patients with septic shock: another sign of hepatoadrenal syndrome? Ming-Hung Tsai1†, Hui-Chun Huang2,3,4†, Yun-Shing Peng5,6, Yung-Chang Chen6,7, Ya-Chung Tian6,7, Chih-Wei Yang6,7, Jau-Min Lien1, Ji-Tseng Fang6,7, Cheng-Shyong Wu6,8, Sen-Yung Hsieh1 and Fa-Yauh Lee2,3* Abstract Background: Cirrhotic patients are susceptible to sepsis and critical illness-related corticosteroid insufficiency (CIRCI). Dehydroepiandrosterone sulfate (DHEAS) is a corticotropin-dependent adrenal androgen, which has immunostimulating and antiglucocorticoid effects. Considering the synchronized synthesis of cortisol and DHEAS and their opposing effects to each other, investigators have proposed measuring these two hormones as a ratio. Severe sepsis has been associated with low DHEAS, especially relative to high cortisol. Despite growing interest in the role of adrenal androgen replacement in critical illness, there have been no data about DHEAS and the DHEAS/cortisol ratio in patients with liver cirrhosis. We studied whether low concentrations of DHEAS and decreased DHEAS/cortisol ratio are associated with poor outcome in patients with liver cirrhosis and septic shock. Methods: We recruited 46 cirrhotic patients with septic shock, and 46 noncirrhotic counterparts matched by age and sex. We evaluated adrenal function using the short corticotropin stimulation test and analyzed the relation between DHEAS and cortisol. Results: While the nonsurvivors in the cirrhotic group had significantly lower baseline DHEAS, lower baseline DHEAS/cortisol ratio, and reduced increments of both DHEAS and cortisol upon corticotropin stimulation, the survivors had lower baseline cortisol. -

Adrenal Suppression Secondary to Exogenous Glucocorticoids See Also: Clinical Guidelines for Adrenal Crisis and Acute Adrenal In
Adrenal suppression secondary to exogenous glucocorticoids See also: Clinical guidelines for Adrenal Crisis and Acute Adrenal insufficiency Background to condition: Glucocorticoids (also known as corticosteroids) are used widely for their anti-inflammatory and immunosuppressive properties in many different conditions e.g. Inflammatory Bowel Disease, induction treatment of Acute Lymphoblastic Leukaemia, Nephrotic Syndrome, Juvenile Rheumatoid Arthritis. Patients for whom reduction and /or cessation of corticosteroid is planned, may be at risk of adrenal insufficiency if the duration of corticosteroid use was prolonged beyond 4 weeks, with increasing risk for longer exposure, such as 6-12+months. In general, doses may be reduced quite rapidly to physiologic levels (10mg/m2/day), then weaned slowly over weeks to several months depending on individual situation. If the patient has a Cushingoid appearance this should be assumed to reflect high or prolonged corticosteroid exposure with increased risk for adrenal suppression. However, the absence of cushingoid appearance does not mean that the patient is not at risk of adrenal suppression. How to assess: (Refer to the Adrenal Crisis and Acute Adrenal insufficiency CPG for assessment and management of adrenal crisis) Hydrocortisone stress dose for significant illness/emergency is 50-100 mg/m2/day Hydrocortisone stress dose for mild to moderate illness is 20-30 mg/m2/day Hydrocortisone maintenance daily requirement is 10 mg/m2/day As a general guide: Hydrocortisone IM/IV Stat Dose < 3 years: 25mg 3-12 years: 50mg >12 years: 100mg Refer to the Adrenal Crisis and Acute Adrenal Insufficiency CPG for ongoing dosing Normal daily glucocorticoid requirement in adults, children and infants is hydrocortisone 5- 10mg/m2/day. -

Serum Dehydroepiandrosterone Sulfate Concentration As an Indicator of Adrenocortical Suppression During Inhaled Steroid Therapy
European Journal of Endocrinology (2004) 150 687–690 ISSN 0804-4643 CLINICAL STUDY Serum dehydroepiandrosterone sulfate concentration as an indicator of adrenocortical suppression during inhaled steroid therapy in adult asthmatic patients Senja Kannisto, Anne Laatikainen1, Antti Taivainen1, Kari Savolainen2, Hannu Tukiainen1 and Raimo Voutilainen Departments of Pediatrics, 1Pulmonary Diseases and 2Clinical Chemistry, Kuopio University Hospital, Kuopio, Finland (Correspondence should be addressed to R Voutilainen, Department of Pediatrics, Kuopio University Hospital, PO Box 1777, FIN–70211 Kuopio, Finland; Email: Raimo.Voutilainen@uku.fi) Abstract Objective: Supraphysiological doses of exogenous glucocorticosteroids cause adrenocortical suppres- sion. Dehydroepiandrosterone sulfate (DHEA-S) is the most abundant adrenal androgen and estrogen precursor. We studied to what extent inhaled glucocorticosteroid therapy for asthma decreases serum DHEA-S concentrations. Design and methods: We measured serum DHEA-S and cortisol concentrations in 101 adult patients with newly detected mild asthma before and after 2 and 12 weeks of treatment with inhaled gluco- corticosteroids. The patients were randomized to receive budesonide 200 mg/day (low dose group, n ¼ 50) or 800 mg/day (high dose group, n ¼ 51) in two parallel groups double-blindly. Results: In the low dose group, serum DHEA-S concentrations decreased from the baseline by a mean of 8 % (95 % confidence interval (CI), 3–13 %, P , 0.01) after 2 weeks of therapy, and by 2 % (95 % CI, 9 % decrease to 5 % increase, NS) after 12 weeks. In the high dose group, the respective decreases were 16 % (95 % CI, 10–21 %, P , 0.001) and 18 % (95 % CI, 12–24 %, P , 0.001). The difference between the treatment groups was significant at both 2 and 12 weeks.