Narratives of Perceived Social Support As a Mediator for Increased Coping Resources and Optimism Among Cancer Patients and Survi
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Three Priests Ordained for the Diocese of Oakland
The Catholic Voice is on Facebook VOL. 57, NO. 11 DIOCESE OF OAKLAND JUNE 10, 2019 www.catholicvoiceoakland.org Serving the East Bay Catholic Community since 1963 Copyright 2019 Three priests ordained for the Diocese of Oakland By Michele Jurich Staff writer Addressing the three men before him, “Soon-to-be Father Mark, Father John and Father Javier,” Bishop Michael C. Barber, SJ, told them, “you are called and chosen” and told them what serving means today. In front of a crowded Cathedral of Christ the Light Bishop Barber told them he was zeroing in on the third vow they would take shortly, to celebrate the Mass and administer the Sacrament of Confession worthily. “You will never violate the Seal of Confession,” Bishop Barber told the three new priests. “No state or government can oblige you to betray your penitents.” Legislation — SB 360 — has passed the state Senate and is moving to the Assembly. It will compel a priest to reveal to police some sins he hears in confession. The new priests, John Anthony Pietruszka, 32, Javier Ramirez, 43, and Mark Ruiz, 56, listened attentively. Father Pietruszka is from Fall River Massachusetts; Father Ramirez from Culiacán, Sinaloa, Mexico; and Mark Father Ruiz was born and raised in Oakland. They would not be alone, the bishop assured them. To show that support, more than 70 VOICE CATHOLIC PACCIORINI/THE C. ALBERT priests, mostly diocesan, were present to With Bishop Michael C. Barber, SJ, at left, the trio of men prostrate themselves at the altar. This symbolizes each man’s offer blessings and the sign of peace to unworthiness for the office to be assumed and his dependence upon God and the prayers of the Christian community. -
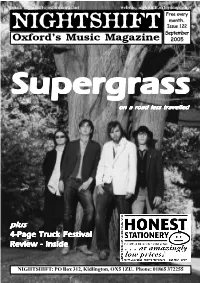
[email protected] Website: Nightshift.Oxfordmusic.Net Free Every Month
email: [email protected] website: nightshift.oxfordmusic.net Free every month. NIGHTSHIFT Issue 122 September Oxford’s Music Magazine 2005 SupergrassSupergrassSupergrass on a road less travelled plus 4-Page Truck Festival Review - inside NIGHTSHIFT: PO Box 312, Kidlington, OX5 1ZU. Phone: 01865 372255 NEWNEWSS Nightshift: PO Box 312, Kidlington, OX5 1ZU Phone: 01865 372255 email: [email protected] THE YOUNG KNIVES won You Now’, ‘Water and Wine’ and themselves a coveted slot at V ‘Gravity Flow’. In addition, the CD Festival last month after being comes with a bonus DVD which picked by Channel 4 and Virgin features a documentary following Mobile from over 1,000 new bands Mark over the past two years as he to open the festival on the Channel recorded the album, plus alternative 4 stage, alongside The Chemical versions of some tracks. Brothers, Doves, Kaiser Chiefs and The Magic Numbers. Their set was THE DOWNLOAD appears to have then broadcast by Channel 4. been given an indefinite extended Meanwhile, the band are currently in run by the BBC. The local music the studio with producer Andy Gill, show, which is broadcast on BBC recording their new single, ‘The Radio Oxford 95.2fm every Saturday THE MAGIC NUMBERS return to Oxford in November, leading an Decision’, due for release on from 6-7pm, has had a rolling impressive list of big name acts coming to town in the next few months. Transgressive in November. The monthly extension running through After their triumphant Truck Festival headline set last month, The Magic th Knives have also signed a publishing the summer, and with the positive Numbers (pictured) play at Brookes University on Tuesday 11 October. -

Isabella Mils M
mulit bur btonittr, ^ C. _id. ..i1OTTE(R, Editor cS- Publisher. Established by SAMUEL MOTTER in 1879. TEP.,115.4.z.c o a Year in Advance. VOL. XIII. EMMITSBURG-, MARYLAND, FRIDAY, APRIL, 22, 1892. SONG. DIRECTORY A SPRING l and dry the hides, and "keep speeches, and last, though not least, A LEGAL vtEw. FOR FREDERICK COUNTY Old Mother Earth woke up from sleep, house" generally. Three, including divine service was held with a hymn Qtlad'w Little ea ery ef it Lawyer and a Railroad Aceidi nt. And found she was cold and bare; myself and Vandewater, were by and prayer, led by a devout man Circuit Com t. The Winter was o'er, the Spring was lie sat just opposite to me in the "drawing straws" detailed to follow Chief Judge--Hon. James atesheery. by the name of Captain Burehard, Amioclate Judges-Hon. John T. Vinson and near, train, and from the legal documents the hunters with the wagon. The and we closed the night's festivi- Bon. John A. Lynch. And she had not a dress to wear. Attorney-Edw. S. Eicheitiorger. he was perusing .had lit doubt State's hunters were paired off in couples Clerk of the Court-John L. Jordan. "Alas l" she sighed, with great dismay, ties by voting Roland Simmons the Court. that he was a lawyer. I looked tint Orphan's "Oh, where shall I get my clothes? to describe a circle of five or six hero of the day. elteleee-Betiard Collitiower, John R. Mille. of the window as the blew There's whistle Harriman not a place to buy a suit, miles, each couple having a horn, Our sport was kept up for six Register of Wills-James K. -

Mark Summers Sunblock Sunburst Sundance
Key - $ = US Number One (1959-date), ✮ UK Million Seller, ➜ Still in Top 75 at this time. A line in red Total Hits : 1 Total Weeks : 11 indicates a Number 1, a line in blue indicate a Top 10 hit. SUNFREAKZ Belgian male producer (Tim Janssens) MARK SUMMERS 28 Jul 07 Counting Down The Days (Sunfreakz featuring Andrea Britton) 37 3 British male producer and record label executive. Formerly half of JT Playaz, he also had a hit a Souvlaki and recorded under numerous other pseudonyms Total Hits : 1 Total Weeks : 3 26 Jan 91 Summers Magic 27 6 SUNKIDS FEATURING CHANCE 15 Feb 97 Inferno (Souvlaki) 24 3 13 Nov 99 Rescue Me 50 2 08 Aug 98 My Time (Souvlaki) 63 1 Total Hits : 1 Total Weeks : 2 Total Hits : 3 Total Weeks : 10 SUNNY SUNBLOCK 30 Mar 74 Doctor's Orders 7 10 21 Jan 06 I'll Be Ready 4 11 Total Hits : 1 Total Weeks : 10 20 May 06 The First Time (Sunblock featuring Robin Beck) 9 9 28 Apr 07 Baby Baby (Sunblock featuring Sandy) 16 6 SUNSCREEM Total Hits : 3 Total Weeks : 26 29 Feb 92 Pressure 60 2 18 Jul 92 Love U More 23 6 SUNBURST See Matt Darey 17 Oct 92 Perfect Motion 18 5 09 Jan 93 Broken English 13 5 SUNDANCE 27 Mar 93 Pressure US 19 5 08 Nov 97 Sundance 33 2 A remake of "Pressure" 10 Jan 98 Welcome To The Future (Shimmon & Woolfson) 69 1 02 Sep 95 When 47 2 03 Oct 98 Sundance '98 37 2 18 Nov 95 Exodus 40 2 27 Feb 99 The Living Dream 56 1 20 Jan 96 White Skies 25 3 05 Feb 00 Won't Let This Feeling Go 40 2 23 Mar 96 Secrets 36 2 Total Hits : 5 Total Weeks : 8 06 Sep 97 Catch Me (I'm Falling) 55 1 20 Oct 01 Pleaase Save Me (Sunscreem -

The George-Anne Student Media
Georgia Southern University Digital Commons@Georgia Southern The George-Anne Student Media 10-23-1997 The George-Anne Georgia Southern University Follow this and additional works at: https://digitalcommons.georgiasouthern.edu/george-anne Part of the Higher Education Commons Recommended Citation Georgia Southern University, "The George-Anne" (1997). The George-Anne. 1496. https://digitalcommons.georgiasouthern.edu/george-anne/1496 This newspaper is brought to you for free and open access by the Student Media at Digital Commons@Georgia Southern. It has been accepted for inclusion in The George-Anne by an authorized administrator of Digital Commons@Georgia Southern. For more information, please contact [email protected]. The Georgia 30460nne unded 192 GOLD EDITION Thursday Faculty Senate approves midterm break for fall semester By Mike Bowdoin for a midterm break. Stone, professor of math and computer October 23,1997 News Editor The senate vote officially sent the fall "THIS IS A TRIUMPH; THIS IS science. Vol. 70, No. 30 GSU's Faculty Senate voted Monday to calendar back to the committee to be "I can't imagine having to jump start A VICTORY FOR STUDENTS." The oldest continuously amend the Calendar Committee's pro- amended. Harry Carter, GSU's vice-presi- students after a nine day break - which is published newspaper in posed schedule for the fall semester in dent of academic affairs, began the debate as long of a break as we've had between Bulloch County favor of Student Government Association's by explaining the actions of the Calendar — CUNT MURPHY, winter and spring quarter," said Pam plan, which will give students a midterm Committee. -

DEPUTY VICE-CHANCELLOR: ACADEMIC Reflective Report 2020
DEPUTY VICE-CHANCELLOR: ACADEMIC Reflective Report 2020 Contents DEPUTY VICE-CHANCELLOR (ACADEMIC) Reflective Report 2020 2 FACULTY OF ARTS AND HUMANITIES 26 FACULTY OF COMMUNITY AND HEALTH SCIENCES 46 FACULTY OF DENTISTRY 62 FACULTY OF EDUCATION 80 FACULTY OF ECONOMIC AND MANAGEMENT SCIENCES 108 FACULTY OF LAW 130 FACULTY OF NATURAL SCIENCES 140 ACADEMIC PLANNING UNIT 156 COMMUNITY ENGAGEMENT UNIT 160 CENTRE FOR INNOVATIVE EDUCATION & COMMUNICATION TECHNOLOGIES (CIECT) 168 CENTRE FOR THE PERFORMING ARTS 186 DIRECTORATE OF LEARNING, TEACHING AND STUDENT SUCCESS (DLTSS) 192 page Deputy Vice-Chancellor: Academic | Reflective Report 2020 1 DEPUTY VICE-CHANCELLOR: ACADEMIC PROF VIVIENNE LAWACK Reflective Report 2020 Since 2017, every Dean and Director within my line has compiled a Reflective Report, which I consolidate, adding my own reflections. The consolidated DVC (Academic) Reflective Report is intended to reflect on the state of the academic project, through the lenses of the seven faculties at the University of the Western Cape (UWC), together with the academic professional support directorates within this portfolio. Given the cataclysmic effects of the ongoing pandemic, it would be remiss not to reflect fully on the impact of the pandemic on the academic project and how we managed to complete the 2020 academic year and start the 2021 academic year timeously. This Reflective Report contains an overview of our academic approach and decision-making during the COVID-19 pandemic in 2020, as well as a self-evaluation of the most pertinent work done during the course of the current Institutional Operation Plan (IOP 2016—2020), including the successes and work that need to be consolidated or accelerated, and opportunities for innovation in the next IOP. -

Music Recommendation and Discovery in the Long Tail
MUSIC RECOMMENDATION AND DISCOVERY IN THE LONG TAIL Oscar` Celma Herrada 2008 c Copyright by Oscar` Celma Herrada 2008 All Rights Reserved ii To Alex and Claudia who bring the whole endeavour into perspective. iii iv Acknowledgements I would like to thank my supervisor, Dr. Xavier Serra, for giving me the opportunity to work on this very fascinating topic at the Music Technology Group (MTG). Also, I want to thank Perfecto Herrera for providing support, countless suggestions, reading all my writings, giving ideas, and devoting much time to me during this long journey. This thesis would not exist if it weren’t for the the help and assistance of many people. At the risk of unfair omission, I want to express my gratitude to them. I would like to thank all the colleagues from MTG that were —directly or indirectly— involved in some bits of this work. Special mention goes to Mohamed Sordo, Koppi, Pedro Cano, Mart´ın Blech, Emilia G´omez, Dmitry Bogdanov, Owen Meyers, Jens Grivolla, Cyril Laurier, Nicolas Wack, Xavier Oliver, Vegar Sandvold, Jos´ePedro Garc´ıa, Nicolas Falquet, David Garc´ıa, Miquel Ram´ırez, and Otto W¨ust. Also, I thank the MTG/IUA Administration Staff (Cristina Garrido, Joana Clotet and Salvador Gurrera), and the sysadmins (Guillem Serrate, Jordi Funollet, Maarten de Boer, Ram´on Loureiro, and Carlos Atance). They provided help, hints and patience when I played around with the machines. During my six months stage at the Center for Computing Research of the National Poly- technic Institute (Mexico City) in 2007, I met a lot of interesting people ranging different disciplines. -

500 Drugstore Feat. Thom Yorke El President 499 Blink
500 DRUGSTORE FEAT. EL PRESIDENT THOM YORKE 499 BLINK 182 ADAMS SONG 498 SCREAMING TREES NEARLY LOST YOU 497 LEFTFIELD OPEN UP 496 SHIHAD BEAUTIFUL MACHINE 495 TEGAN AND SARAH WALKING WITH A GHOST 494 BOMB THE BASS BUG POWDER DUST 493 BAND OF HORSES IS THERE A GHOST 492 BLUR BEETLEBUM 491 DISPOSABLE HEROES TELEVISION THE DRUG OF THE OF... NATION 490 FOO FIGHTERS WALK 489 AIR SEXY BOY 488 IGGY POP CANDY 487 NINE INCH NAILS THE HAND THAT FEEDS 486 PEARL JAM NOT FOR YOU 485 RADIOHEAD EVERYTHING IN ITS RIGHT PLACE 484 RANCID TIME BOMB 483 RED HOT CHILI MY FRIENDS PEPPERS 482 SANTIGOLD LES ARTISTES 481 SMASHING PUMPKINS AVA ADORE 480 THE BIG PINK DOMINOS 479 THE STROKES REPTILIA 478 THE PIXIES VELOURIA 477 BON IVER SKINNY LOVE 476 ANIMAL COLLECTIVE MY GIRLS 475 FILTER HEY MAN NICE SHOT 474 BRAD 20TH CENTURY 473 INTERPOL SLOW HANDS 472 MAD SEASON SLIP AWAY 471 OASIS SOME MIGHT SAY 470 SLEIGH BELLS RILL RILL 469 THE AFGHAN WHIGS 66 468 THE FLAMING LIPS FIGHT TEST 467 ALICE IN CHAINS MAN IN THE BOX 466 FAITH NO MORE A SMALL VICTORY 465 THE THE DOGS OF LUST 464 ARCTIC MONKEYS R U MINE 463 BECK DEADWEIGHT 462 GARBAGE MILK 461 BEN FOLDS FIVE BRICK 460 NIRVANA PENNYROYAL TEA 459 SHIHAD YR HEAD IS A ROCK 458 SNEAKER PIMPS 6 UNDERGROUND 457 SOUNDGARDEN BURDEN IN MY HAND 456 EMINEM LOSE YOURSELF 455 SUPERGRASS RICHARD III 454 UNDERWORLD PUSH UPSTAIRS 453 ARCADE FIRE REBELLION (Lies) 452 RADIOHEAD BLACK STAR 451 BIG DATA DANGEROUS 450 BRAN VAN 3000 DRINKING IN LA 449 FIONA APPLE CRIMINAL 448 KINGS OF LEON USE SOMEBODY 447 PEARL JAM GETAWAY 446 BEASTIE -

Thugs Sent Round to Threaten Tenants LANDLORD DRAFTS IN
Incorporating juice magazine Guardian/ NUS Student Newspaper of the Year Thugs sent round to threaten tenants LANDLORD DRAFTS IN HEAVBy GARETH EVANS Y MOB THREE finalists fled their house days before their exams, claiming a gang threatened them with violence if they refused to pay outstanding rent. Merewyn Fenton, Chris Greenfield and Scott Dinnis left EXCLUSIVE! their house within a day of the alleged threats and stayed at home. First British They claim they were threatened by a gang of men who barged into their house review of and warned they could expect violence if they did not pay up. It is the latest chapter in a year of conflict with their estate agents, which looks set to end up in court. Demands The agencx sent letters demanding more thai) two thousand pounds which also co\ered repair \\ork. The students took legal ad\ ice. convinced thcx \\ ere not liable tor these expenses and claim the agents reacted b\ sending oxer the thugs. "Scott and 1 xxerc out so Chris xxas alone in the house." said Merexxxn. "these txxo blokes came around asking lo look round the house, \\heii he opened the door thex pushed him inside and told him it xxc didn't pax up. thex xxould come back and beat us all up. Chris is usuallx an casx -going bloke, but he xxas really shaken up." The trouble began xxhen one housemate left in September lor a xxork placement leax ing the remaining BRAVE BATTLER: LMU graduate Vicki Hunter is suing three to find another person to till their house Birmingham Health Authority for damages, claiming a A I'orlugiicsc waiter moxed in but left txxo months misdiagnosis resulted in the loss of her leg which was later \\ithout pax ing an\ deposit, rent or hills. -

Artist Song Weird Al Yankovic My Own Eyes .38 Special Caught up in You .38 Special Hold on Loosely 3 Doors Down Here Without
Artist Song Weird Al Yankovic My Own Eyes .38 Special Caught Up in You .38 Special Hold On Loosely 3 Doors Down Here Without You 3 Doors Down It's Not My Time 3 Doors Down Kryptonite 3 Doors Down When I'm Gone 3 Doors Down When You're Young 30 Seconds to Mars Attack 30 Seconds to Mars Closer to the Edge 30 Seconds to Mars The Kill 30 Seconds to Mars Kings and Queens 30 Seconds to Mars This is War 311 Amber 311 Beautiful Disaster 311 Down 4 Non Blondes What's Up? 5 Seconds of Summer She Looks So Perfect The 88 Sons and Daughters a-ha Take on Me Abnormality Visions AC/DC Back in Black (Live) AC/DC Dirty Deeds Done Dirt Cheap (Live) AC/DC Fire Your Guns (Live) AC/DC For Those About to Rock (We Salute You) (Live) AC/DC Heatseeker (Live) AC/DC Hell Ain't a Bad Place to Be (Live) AC/DC Hells Bells (Live) AC/DC Highway to Hell (Live) AC/DC The Jack (Live) AC/DC Moneytalks (Live) AC/DC Shoot to Thrill (Live) AC/DC T.N.T. (Live) AC/DC Thunderstruck (Live) AC/DC Whole Lotta Rosie (Live) AC/DC You Shook Me All Night Long (Live) Ace Frehley Outer Space Ace of Base The Sign The Acro-Brats Day Late, Dollar Short The Acro-Brats Hair Trigger Aerosmith Angel Aerosmith Back in the Saddle Aerosmith Crazy Aerosmith Cryin' Aerosmith Dream On (Live) Aerosmith Dude (Looks Like a Lady) Aerosmith Eat the Rich Aerosmith I Don't Want to Miss a Thing Aerosmith Janie's Got a Gun Aerosmith Legendary Child Aerosmith Livin' On the Edge Aerosmith Love in an Elevator Aerosmith Lover Alot Aerosmith Rag Doll Aerosmith Rats in the Cellar Aerosmith Seasons of Wither Aerosmith Sweet Emotion Aerosmith Toys in the Attic Aerosmith Train Kept A Rollin' Aerosmith Walk This Way AFI Beautiful Thieves AFI End Transmission AFI Girl's Not Grey AFI The Leaving Song, Pt. -

A Framework for Progressively Improving Small Area Population Estimates
J. R. Statist. Soc. A (2004) 167, Part 1, pp. 5–36 A framework for progressively improving small area population estimates Philip Rees, University of Leeds, UK Paul Norman University of Manchester, UK and Dominic Brown University of Queensland, Australia [Received April 2002. Final revision May 2003] Summary. The paper presents a framework for small area population estimation that enables users to select a method that is fit for the purpose.The adjustments to input data that are needed before use are outlined, with emphasis on developing consistent time series of inputs. We show how geographical harmonization of small areas, which is crucial to comparisons over time, can be achieved. For two study regions, the East of England and Yorkshire and the Humber, the dif- ferences in output and consequences of adopting different methods are illustrated. The paper concludes with a discussion of how data, on stream since 1998, might be included in future small area estimates. Keywords: Estimation methods; Geographical harmonization; Population estimates; Small area populations 1. Introduction Changes in small area populations occur through aging and the processes of natural change, births and deaths. Population change also occurs through migration within and between small areas, whether urban, suburban or rural, with different migration patterns for people of differ- ent age groups. In some locations the tendency is for people to age in situ; other areas have more transient populations. In the UK, since information from the decennial census, the principal source of sociodemographic data, is only available for one date per decade, there is a need to esti- mate small area populations from the latest census forwards and then to revise these estimates when the next census is published. -

1 Giant Leap Dreadlock Holiday -- 10Cc I'm Not in Love
Dumb -- 411 Chocolate -- 1975 My Culture -- 1 Giant Leap Dreadlock Holiday -- 10cc I'm Not In Love -- 10cc Simon Says -- 1910 Fruitgum Company The Sound -- 1975 Wiggle It -- 2 In A Room California Love -- 2 Pac feat. Dr Dre Ghetto Gospel -- 2 Pac feat. Elton John So Confused -- 2 Play feat. Raghav & Jucxi It Can't Be Right -- 2 Play feat. Raghav & Naila Boss Get Ready For This -- 2 Unlimited Here I Go -- 2 Unlimited Let The Beat Control Your Body -- 2 Unlimited Maximum Overdrive -- 2 Unlimited No Limit -- 2 Unlimited The Real Thing -- 2 Unlimited Tribal Dance -- 2 Unlimited Twilight Zone -- 2 Unlimited Short Short Man -- 20 Fingers feat. Gillette I Want The World -- 2Wo Third3 Baby Cakes -- 3 Of A Kind Don't Trust Me -- 3Oh!3 Starstrukk -- 3Oh!3 ft Katy Perry Take It Easy -- 3SL Touch Me, Tease Me -- 3SL feat. Est'elle 24/7 -- 3T What's Up? -- 4 Non Blondes Take Me Away Into The Night -- 4 Strings Dumb -- 411 On My Knees -- 411 feat. Ghostface Killah The 900 Number -- 45 King Don't You Love Me -- 49ers Amnesia -- 5 Seconds Of Summer Don't Stop -- 5 Seconds Of Summer She Looks So Perfect -- 5 Seconds Of Summer She's Kinda Hot -- 5 Seconds Of Summer Stay Out Of My Life -- 5 Star System Addict -- 5 Star In Da Club -- 50 Cent 21 Questions -- 50 Cent feat. Nate Dogg I'm On Fire -- 5000 Volts In Yer Face -- 808 State A Little Bit More -- 911 Don't Make Me Wait -- 911 More Than A Woman -- 911 Party People..