Medications – Administration of the First Dose of Medication SECTION: 16.01 Strength of Evidence Level: 3
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
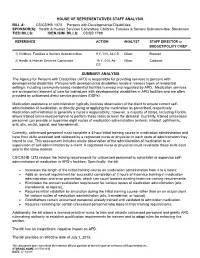
CS/CS/HB 1373 Persons with Developmental Disabilities
HOUSE OF REPRESENTATIVES STAFF ANALYSIS BILL #: CS/CS/HB 1373 Persons with Developmental Disabilities SPONSOR(S): Health & Human Services Committee; Children, Families & Seniors Subcommittee; Stevenson TIED BILLS: IDEN./SIM. BILLS: CS/SB 1788 REFERENCE ACTION ANALYST STAFF DIRECTOR or BUDGET/POLICY CHIEF 1) Children, Families & Seniors Subcommittee 9 Y, 0 N, As CS Gilani Brazzell 2) Health & Human Services Committee 16 Y, 0 N, As Gilani Calamas CS SUMMARY ANALYSIS The Agency for Persons with Disabilities (APD) is responsible for providing services to persons with developmental disabilities. Persons with developmental disabilities reside in various types of residential settings, including community-based residential facilities licensed and regulated by APD. Medication services are an important element of care for individuals with developmental disabilities in APD facilities and are often provided by unlicensed direct service providers (DSPs). Medication assistance or administration typically involves observation of the client to ensure correct self- administration of medication, or directly giving or applying the medication as prescribed, respectively. Medication administration is generally a nurse’s responsibility; however, a majority of states, including Florida, allows trained unlicensed personnel to perform these tasks to meet the demand. Currently, trained unlicensed personnel can provide or supervise eight routes of medication administration (enteral, inhaled, ophthalmic, oral, otic, rectal, topical, and transdermal). Currently, unlicensed personnel must complete a 4-hour initial training course in medication administration and have their skills assessed and validated by a registered nurse or physician in each route of administration they intend to use. This assessment includes onsite observation of the administration of medication to or supervision of self-administration by a client. -

Oral Dosage Forms That Should Not Be Crushed Formulary-Specific List for VCMC and SPH
Oral Dosage Forms That Should Not be Crushed Formulary-Specific List for VCMC and SPH Generic Brand Dosage Form(s) Reasons/Comments amoxicillin-clavulanate Augmentin XR Tablet Slow-release (b,h) aspirin Aspirin EC Caplet; Tablet Slow-release; Enteric-coated aspirin and dipyridamole Aggrenox XR Capsule Slow-release atazanavir Reyataz Capsule Note: an oral powder is available, see prescribing information for administration instructions atomoxetine Strattera Capsule Note: capsule contents can cause ocular irritation - Do not open capsules as contents are an ocular irritant benzonatate Tessalon Perles Capsule Note: swallow whole; local anesthesia of the oral mucosa; choking could occur - Capsules are liquid-filled “perles” - Do not alter (break, cut, chew) integrity of dosage form; local mucosal irritant and anesthetic bisacodyl Dulcolax Capsule; Tablet Enteric-coated (c) bosentan Tracleer Tablet Note: women who are, or may become, pregnant, should not handle crushed or broken tablets brivaracetam Briviact Tablet Film-coated (b) budesonide Entocort EC Capsule Enteric-coated (a) - Capsules contain enteric-coated granules in extended-release matrix; can open capsules but do not crush contents - Products are formulated to release active drug at mid- to late small intestine buPROPion Wellbutrin XL Tablet Slow-release - Do not crush extended-release tablets - Immediate-release tablet products may be film-coated March 2019 carvedilol phosphate Coreg CR Capsule Slow-release (a) (Note: may add contents of capsule to chilled, not warm, applesauce -

Intravenous Therapy Procedure Manual
INTRAVENOUS THERAPY PROCEDURE MANUAL - 1 - LETTER OF ACCEPTANCE __________________________________________ hereby approves (Facility) the attached Reference Manual as of _____________________. (Date) The Intravenous Therapy Procedure Manual will be reviewed at least annually or more often when deemed appropriate. Revisions will be reviewed as they occur. Current copies of the Intravenous Therapy Procedure Manual shall be maintained at each appropriate nursing station. I have reviewed this manual and agree to its approval. __________________________ (Administrator) __________________________ (Director of Nursing) __________________________ (Medical Director) - 2 - TABLE OF CONTENTS TABLE OF CONTENTS INTRODUCTION A. Purpose 1 B. Local Standard of Practice 1 RESPONSIBILITIES A. Responsibilities: M Chest Pharmacy 1 B. Responsibilities: Administrator 1 C. Responsibilities: Director of Nursing Services (DON/DNS) 1 D. Skills Validation 2 AMENDMENTS GUIDELINES A. Resident Candidacy for IV Therapy 1 B. Excluded IV Medications and Therapies 1 C. Processing the IV Order 1 D. IV Solutions/Medications: Storage 2 E. IV Solutions/Medications: Handling 3 F. IV Solutions and Supplies: Destroying and Returning 4 G. IV Tubing 5 H. Peripheral IV Catheters and Needles 6 I. Central Venous Devices 7 J. Documentation and Monitoring 8 K. IV Medication Administration Times 9 L. Emergency IV Supplies 10 I TABLE OF CONTENTS PROTOCOLS A. IV Antibiotic 1 1. Purpose 2. Guidelines 3. Nursing Responsibilities B. IV Push 2 1. Purpose 2. Guidelines C. Anaphylaxis Allergic Reaction 4 1. Purpose 2. Guidelines 3. Nursing Responsibilities and Interventions 4. Signs and Symptoms of Anaphylaxis 5. Drugs Used to Treat Anaphylaxis 6. Physician Protocol PRACTICE GUIDELINES A. Purpose 1 B. Personnel 1 C. Competencies 1 D. -

Download Book
Methods in Molecular Biology 2000 Volkmar Weissig Tamer Elbayoumi Editors Pharmaceutical Nanotechnology Basic Protocols M ETHODS IN M OLECULAR B IOLOGY Series Editor John M. Walker School of Life and Medical Sciences University of Hertfordshire Hatfield, Hertfordshire AL10 9AB, UK For further volumes: http://www.springer.com/series/7651 Pharmaceutical Nanotechnology Basic Protocols Edited by Volkmar Weissig and Tamer Elbayoumi Department of Pharmaceutical Sciences, College of Pharmacy, Midwestern University, Glendale, AZ, USA Nanomedicine Center of Excellence in Translational Cancer Research, Midwestern University, Glendale, AZ, USA Editors Volkmar Weissig Tamer Elbayoumi Department of Pharmaceutical Sciences Department of Pharmaceutical Sciences College of Pharmacy, Midwestern University College of Pharmacy, Midwestern University Glendale, AZ, USA Glendale, AZ, USA Nanomedicine Center of Excellence Nanomedicine Center of Excellence in Translational Cancer Research in Translational Cancer Research Midwestern University Midwestern University Glendale, AZ, USA Glendale, AZ, USA ISSN 1064-3745 ISSN 1940-6029 (electronic) Methods in Molecular Biology ISBN 978-1-4939-9515-8 ISBN 978-1-4939-9516-5 (eBook) https://doi.org/10.1007/978-1-4939-9516-5 © Springer Science+Business Media, LLC, part of Springer Nature 2019 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, specifically the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on microfilms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. The use of general descriptive names, registered names, trademarks, service marks, etc. -

Clinical Practice Statements-Oral Contact Allergy
Clinical Practice Statements-Oral Contact Allergy Subject: Oral Contact Allergy The American Academy of Oral Medicine (AAOM) affirms that oral contact allergy (OCA) is an oral mucosal response that may be associated with materials and substances found in oral hygiene products, common food items, and topically applied agents. The AAOM also affirms that patients with suspected OCA should be referred to the appropriate dental and/or medical health care provider(s) for comprehensive evaluation and management of the condition. Replacement and/or substitution of dental materials should be considered only if (1) a reasonable temporal association has been established between the suspected triggering material and development of clinical signs and/or symptoms, (2) clinical examination supports an association between the suspected triggering material and objective clinical findings, and (3) diagnostic testing (e.g., dermatologic patch testing, skin-prick testing) confirms a hypersensitivity reaction to the suspected offending material. Originators: Dr. Eric T. Stoopler, DMD, FDS RCSEd, FDS RCSEng, Dr. Scott S. De Rossi, DMD. This Clinical Practice Statement was developed as an educational tool based on expert consensus of the American Academy of Oral Medicine (AAOM) leadership. Readers are encouraged to consider the recommendations in the context of their specific clinical situation, and consult, when appropriate, other sources of clinical, scientific, or regulatory information prior to making a treatment decision. Originator: Dr. Eric T. Stoopler, DMD, FDS RCSEd, FDS RCSEng, Dr. Scott S. De Rossi, DMD Review: AAOM Education Committee Approval: AAOM Executive Committee Adopted: October 17, 2015 Updated: February 5, 2016 Purpose The AAOM affirms that oral contact allergy (OCA) is an oral mucosal response that may be associated with materials and substances found in oral hygiene products, common food items, and topically applied agents. -

Attachment 3
CURRICULUM CLINICAL BASE / CA-1 / CA-2 / CA-3 ANESTHESIOLOGY RESIDENCY PROGRAM GOALS AND OBJECTIVES AND CORE COMPETENCIES Department of Anesthesiology University of Missouri at Kansas City School of Medicine Saint Luke’s Hospital Truman Medical Center Children’s Mercy Hospital Revised 2011 Table of Contents Pages Introduction – Statement of Curriculum ................................................................................................................... 3 I. Rendering Patient Insensible to Pain ............................................................................................................. 4-10 II. Support of Life Functions ............................................................................................................................. 11-16 III. Clinical Base Year A. Cardiology ................................................................................................................................................. 17-32 B. Emergency Medicine ................................................................................................................................. 33-44 C. General Medicine ....................................................................................................................................... 45-49 D. Infectious Disease ...................................................................................................................................... 50-59 E. Nephrology .............................................................................................................................................. -

Nicotine Patches Appear Safe for CAD Patients
May 1, 2007 • www.internalmedicinenews.com Cardiovascular Medicine 37 Nicotine Patches Appear Safe for CAD Patients BY BRUCE JANCIN 30%, but many physicians have been re- induced myocardial defect on single-photon ment arm jumped from 10.9 to 25.2 Denver Bureau luctant to recommend it for their patients emission computed tomography (SPECT) ng/mL, Dr. Leja said. After 1 week, patients with coronary artery disease (CAD) be- to receive either 21-mg nicotine patches or were encouraged to quit smoking while N EW O RLEANS — Nicotine patches cause nicotine is known to increase heart placebo in addition to continuing their usu- continuing to use their assigned patches. are safe for use in smokers with known rate and blood pressure, and can induce al amount of cigarette smoking. The pri- Upon SPECT imaging at week 4, the coronary artery disease and stress-induced vasoconstriction as well, Dr. Monika J. Leja mary end point of the study was change in size of the perfusion defects in the nico- myocardial ischemia, according to the re- reported at the annual scientific session of total perfusion defect size upon repeat stress tine patch group remained unchanged sults of the first-ever randomized, place- the American College of Cardiology. SPECT imaging performed at 1 week. from baseline, although their plasma nico- bo-controlled, multicenter clinical trial to Dr. Leja and her coinvestigators at the There was no change in the total or is- tine levels remained as high as at week 1. examine this issue. Methodist DeBakey Heart Center in Hous- chemic perfusion defect size, compared The trial was supported by Glaxo- Nicotine replacement therapy doubles ton randomized 55 heavy smokers with with baseline, in either group even though SmithKline Consumer Healthcare. -

SUMMARY of PRODUCT CHARACTERISTICS 2.1 General Description 2.2 Qualitative and Quantitative Composition
THERADOL 50 mg Effervescent tablets 1 Summary of product characteristics SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT THERADOL 50 mg Effervescent tablets. 2. QUALITATIVE AND QUANTITATIVE COMPOSITION 2.1 General description Round, biplane white or off-white tablets with bevel-edges on both sides. 2.2 Qualitative and quantitative composition Tramadol hydrochloride 50 mg per effervescent tablet. This product also contains sodium 214 mg, lactose 75 mg and aspartame 10 mg per tablet. For a full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Effervescent tablet. 4. CLINICAL PARTICULARS 4.1. Therapeutic indications Treatment of moderate to severe acute and chronic pain, such as pain due to surgery, trauma, malignancy. 4.2. Posology and method of administration Posology As with all analgesic drugs, the dose of THERADOL 50 mg Effervescent tablets should be adjusted according to the intensity of the pain and the sensitivity of the individual patient. The lowest effective dose for analgesia should generally be selected. Adults and children aged 12 years and over: The usual dose is 50 to 100 mg (1 to 2 effervescent tablets), 3 to 4 times a day. In children from 12 to 14 years, it is recommended to use the lowest dose. Geriatric patients THERADOL 50 mg Effervescent tablets 2 Summary of product characteristics A dose adjustment is not usually necessary in patients up to 75 years without clinically manifest hepatic or renal insufficiency. In elderly patients over 75 years elimination may be prolonged. Therefore, if necessary the dosage interval is to be extended according to the patient's requirements. -

Topical Medication Administration
Wisconsin Department of Public Instruction Medication Administration Assessment for Topical Medication Administration Name: ____________________________________________ Please circle the correct answer and take the completed test to the school nurse or school district administrator for scoring. 1. Which of the following is not a common form of topical skin medication administration in schools? a. Ointment b. Patches c. Solutions d. Gelatin 2. Which of the following is not considered one of the five rights or guidelines to administer medications? a. Right time b. Right drug c. Right location d. Right route 3. What is the most correct sequence of event for administration of a topical medicated patch? a. Wash hands and apply gloves, check the 5 rights, write date, time and initials on patch, open package and apply medicated patch, remove gloves and record on medication administration record. b. Apply gloves, check the 4 rights, open package and apply medicated patch, write date, time and initials on patch, remove gloves and wash hands, and record on medication administration record. c. Record on medication administration record, wash hands and apply gloves, check the first 5 rights, open package and apply medicated patch, write date, time and initials on patch, remove gloves and wash hands. d. Wash hands and apply gloves, check the 5 rights, open package and apply medicated patch, write date, time and initials on patch, remove gloves and wash hands and record on medication administration record. WI DPI 07/06/2016 Wisconsin Department of Public Instruction Medication Administration 4. It is important to report to the school nurse or parent any signs of skin irritation. -

Immediate Hypersensitivity Reactions Caused by Drug Excipients: a Literature Review Caballero ML, Quirce S
REVIEWS Immediate Hypersensitivity Reactions Caused by Drug Excipients: A Literature Review Caballero ML, Quirce S Department of Allergy, La Paz University Hospital, IdiPAZ, Madrid, Spain J Investig Allergol Clin Immunol 2020; Vol. 30(2): 86-100 doi: 10.18176/jiaci.0476 Abstract The European Medicines Agency defines excipients as the constituents of a pharmaceutical form apart from the active substance. Immediate hypersensitivity reactions (IHRs) caused by excipients contained in the formulation of medications have been described. However, there are no data on the prevalence of IHRs due to drug excipients. Clinical manifestations of allergy to excipients can range from skin disorders to life-threatening systemic reactions. The aim of this study was to review the literature on allergy to pharmaceutical excipients and to record the IHRs described with various types of medications, specifically reactions due to the excipients contained in their formulations. The cases reported were sorted alphabetically by type of medication and excipient in order to obtain a list of the excipients most frequently involved for each type of medication. Key words: Allergy. Drug immediate hypersensitivity reaction. Excipient. Pharmaceutical excipients. Resumen La Agencia Europea de Medicamentos define los excipientes como los componentes de una forma farmacéutica diferenciados del principio activo. Se han descrito reacciones de hipersensibilidad inmediata causadas por los excipientes contenidos en la formulación de medicamentos. Sin embargo, no hay datos sobre la prevalencia de dichas reacciones. Las manifestaciones clínicas de la alergia a los excipientes pueden ir desde trastornos de la piel hasta reacciones sistémicas que ponen en peligro la vida. El objetivo de este estudio fue realizar una revisión de la literatura sobre la alergia a los excipientes farmacéuticos y recopilar las reacciones inmediatas descritas con diferentes tipos de medicamento, debido solo a excipientes contenidos en sus formulaciones. -

Spanish 2018 Rx4 Traditional Drug List
Cambios Anuales de Rx4 Traditional 2018 Fecha de entrada en vigor: 01/01/2018 Para visualizarlo en español, haga clic aquí. To view your full Drug List, click here. ¡Bienvenido a Humana! Los cambios al formulario adjunto, o Lista de medicamentos, entran en vigor el 1 de enero de 2018. Visite Humana.com e inicie sesión en MyHumana –su cuenta en línea segura y personal– a partir de la fecha de su renovación para ver los beneficios de medicamentos recetados específicos, incluidos los copagos o el costo compartido, las limitaciones y las exclusiones. También puede consultar su Certificado de cobertura/seguro o su Descripción resumida del plan/Póliza de seguro. Si tiene preguntas: • Posibles afiliados: llamar a Atención al Cliente al número que aparece en los materiales de inscripción • Afiliados actuales: llamar al número indicado al reverso de su tarjeta de identificación de Humana Cómo leer los cambios a su Lista de medicamentos anual Algunos medicamentos cubiertos pueden tener requisitos adicionales o límites en la cobertura. Hable con su médico o proveedor de atención médica si su medicamento tiene un requisito adicional. Estos requisitos y límites pueden incluir: Estatus de la cobertura (CVG, por sus siglas en inglés): Ciertos medicamentos que anteriormente no estaban cubiertos en virtud de los beneficios de su plan se agregarán a su Lista de medicamentos para 2018, mientras que otros medicamentos que quizás estaban cubiertos en el pasado, se eliminarán. Tenga en cuenta que si usted surte o repite la receta de cualquier medicamento no cubierto en virtud de los beneficios de su plan, quizás deba pagar el costo total de su medicamento recetado. -
Intravenous Infusion Drug Administration: Flushing Guidance
Intravenous Infusion Drug Administration: Flushing Guidance April 2019 Acknowledgements: Andrew Barton – Author/reviewer NIVAS Chair Advanced Nurse Practitioner, IV Therapy and Vascular Access Frimley Health NHS Foundation Trust Tim Jackson – Reviewer/contributor, NIVAS Board Deputy Chair Consultant in Anesthesia & Intensive Care Medicine Calderdale & Huddersfield NHS Foundation Trust Gemma Oliver - Reviewer/contributor NIVAS Board Nurse Consultant, Integrated IV Care East Kent Hospitals NHS Foundation Trust Nicola York - Reviewer/contributor NIVAS Board Clinical Nurse Manager Vascular Access and Nutrition support Oxford University Hospitals NHS Foundation Trust Matt Jones - Reviewer/contributor NIVAS Board Consultant Anaesthetist East Kent Hospitals NHS Foundation Trust Steve Hill - Reviewer/contributor NIVAS Board Procedural Team Manger The Christie NHS Foundation Trust Marie Woodley - Reviewer/contributor NIVAS Board Clinical Nurse Specialist IV therapy/OPAT Lead Buckinghamshire Healthcare Trust Contents: Introduction………………………………………………………………………… Page 1 Methods of administering intravenous therapy………………………………… Page 2 Intravenous bolus injection…………………………………………….… Page 2 Continuous, variable dose syringe driver injection……………………. Page 2 Intravenous infusion…………………………………………………….… Page 3 Option 1: Discarding the infusion set………………………………….… Page 3 Option 2: Flushing the Infusion set manually…………………………... Page 4 Option 3: Flushing the infusion set with a closed system…………….. Page 4 General Guidance…………………………………………………………………. Page 5 Conclusion………………………………………………………………………….