Clinical Practice Statements-Oral Contact Allergy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
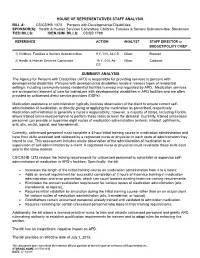
CS/CS/HB 1373 Persons with Developmental Disabilities
HOUSE OF REPRESENTATIVES STAFF ANALYSIS BILL #: CS/CS/HB 1373 Persons with Developmental Disabilities SPONSOR(S): Health & Human Services Committee; Children, Families & Seniors Subcommittee; Stevenson TIED BILLS: IDEN./SIM. BILLS: CS/SB 1788 REFERENCE ACTION ANALYST STAFF DIRECTOR or BUDGET/POLICY CHIEF 1) Children, Families & Seniors Subcommittee 9 Y, 0 N, As CS Gilani Brazzell 2) Health & Human Services Committee 16 Y, 0 N, As Gilani Calamas CS SUMMARY ANALYSIS The Agency for Persons with Disabilities (APD) is responsible for providing services to persons with developmental disabilities. Persons with developmental disabilities reside in various types of residential settings, including community-based residential facilities licensed and regulated by APD. Medication services are an important element of care for individuals with developmental disabilities in APD facilities and are often provided by unlicensed direct service providers (DSPs). Medication assistance or administration typically involves observation of the client to ensure correct self- administration of medication, or directly giving or applying the medication as prescribed, respectively. Medication administration is generally a nurse’s responsibility; however, a majority of states, including Florida, allows trained unlicensed personnel to perform these tasks to meet the demand. Currently, trained unlicensed personnel can provide or supervise eight routes of medication administration (enteral, inhaled, ophthalmic, oral, otic, rectal, topical, and transdermal). Currently, unlicensed personnel must complete a 4-hour initial training course in medication administration and have their skills assessed and validated by a registered nurse or physician in each route of administration they intend to use. This assessment includes onsite observation of the administration of medication to or supervision of self-administration by a client. -

White Lesions of the Oral Cavity and Derive a Differential Diagnosis Four for Various White Lesions
2014 self-study course four course The Ohio State University College of Dentistry is a recognized provider for ADA, CERP, and AGD Fellowship, Mastership and Maintenance credit. ADA CERP is a service of the American Dental Association to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP does not approve or endorse individual courses or instructors, nor does it imply acceptance of credit hours by boards of dentistry. Concerns or complaints about a CE provider may be directed to the provider or to ADA CERP at www.ada.org/goto/cerp. The Ohio State University College of Dentistry is approved by the Ohio State Dental Board as a permanent sponsor of continuing dental education ABOUT this FREQUENTLY asked COURSE… QUESTIONS… Q: Who can earn FREE CE credits? . READ the MATERIALS. Read and review the course materials. A: EVERYONE - All dental professionals in your office may earn free CE contact . COMPLETE the TEST. Answer the credits. Each person must read the eight question test. A total of 6/8 course materials and submit an questions must be answered correctly online answer form independently. for credit. us . SUBMIT the ANSWER FORM Q: What if I did not receive a ONLINE. You MUST submit your confirmation ID? answers ONLINE at: A: Once you have fully completed your p h o n e http://dent.osu.edu/sterilization/ce answer form and click “submit” you will be directed to a page with a . RECORD or PRINT THE 614-292-6737 unique confirmation ID. CONFIRMATION ID This unique ID is displayed upon successful submission Q: Where can I find my SMS number? of your answer form. -

Features of Reactive White Lesions of the Oral Mucosa
Head and Neck Pathology (2019) 13:16–24 https://doi.org/10.1007/s12105-018-0986-3 SPECIAL ISSUE: COLORS AND TEXTURES, A REVIEW OF ORAL MUCOSAL ENTITIES Frictional Keratosis, Contact Keratosis and Smokeless Tobacco Keratosis: Features of Reactive White Lesions of the Oral Mucosa Susan Müller1 Received: 21 September 2018 / Accepted: 2 November 2018 / Published online: 22 January 2019 © Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract White lesions of the oral cavity are quite common and can have a variety of etiologies, both benign and malignant. Although the vast majority of publications focus on leukoplakia and other potentially malignant lesions, most oral lesions that appear white are benign. This review will focus exclusively on reactive white oral lesions. Included in the discussion are frictional keratoses, irritant contact stomatitis, and smokeless tobacco keratoses. Leukoedema and hereditary genodermatoses that may enter in the clinical differential diagnoses of frictional keratoses including white sponge nevus and hereditary benign intraepithelial dyskeratosis will be reviewed. Many products can result in contact stomatitis. Dentrifice-related stomatitis, contact reactions to amalgam and cinnamon can cause keratotic lesions. Each of these lesions have microscopic findings that can assist in patient management. Keywords Leukoplakia · Frictional keratosis · Smokeless tobacco keratosis · Stomatitis · Leukoedema · Cinnamon Introduction white lesions including infective and non-infective causes will be discussed -

Topical Medication Administration
Wisconsin Department of Public Instruction Medication Administration Assessment for Topical Medication Administration Name: ____________________________________________ Please circle the correct answer and take the completed test to the school nurse or school district administrator for scoring. 1. Which of the following is not a common form of topical skin medication administration in schools? a. Ointment b. Patches c. Solutions d. Gelatin 2. Which of the following is not considered one of the five rights or guidelines to administer medications? a. Right time b. Right drug c. Right location d. Right route 3. What is the most correct sequence of event for administration of a topical medicated patch? a. Wash hands and apply gloves, check the 5 rights, write date, time and initials on patch, open package and apply medicated patch, remove gloves and record on medication administration record. b. Apply gloves, check the 4 rights, open package and apply medicated patch, write date, time and initials on patch, remove gloves and wash hands, and record on medication administration record. c. Record on medication administration record, wash hands and apply gloves, check the first 5 rights, open package and apply medicated patch, write date, time and initials on patch, remove gloves and wash hands. d. Wash hands and apply gloves, check the 5 rights, open package and apply medicated patch, write date, time and initials on patch, remove gloves and wash hands and record on medication administration record. WI DPI 07/06/2016 Wisconsin Department of Public Instruction Medication Administration 4. It is important to report to the school nurse or parent any signs of skin irritation. -
Medication Administration
© adistockShutterStock, Inc. CHAPTER 3 Medication Administration Tara Kavanaugh Medication error KEY TERMS CHAPTER OBJECTIVES Oral Buccal Subcutaneous At the end of the chapter, the reader will be Depot preparations Sublingual able to: Injectable pen Transdermal 1. Define key terms. Intramuscular Transmucosal 2. Discuss the nurse’s role in medication Intraosseous administration. Intravenous 3. Identify the eight medication rights and Medication three patient checks. administration 4. Identify the steps in administering error medications using different delivery methods. 5. Discuss current trends in medication administration. 6. Identify methods to help reduce medication errors. © Jones & Bartlett Learning, LLC. NOT FOR SALE OR DISTRIBUTION. 9781449689391_CH03_055_088.indd 55 08/09/14 10:10 am 56 CHAPTER 3 Medication Administration Introduction Medication is transferred into the body’s tissues in one of three ways: (1) by ingestion and absorption in the digestive tract; (2) by passive transfer through porous tissues, such as the skin, the alveoli of the lungs, and the mucous membranes; or (3) by insertion directly into the interior tissues via subcutaneous, intramuscular, or intrathecal injection or intravenous/intraosseous infusion. The central goal of nursing pharmacology is to enable nurses to provide medications to patients safely and appropriately using the route best suited for the administration. Within that seemingly simple statement is held a complex set of information defining the nurse’s relationship with his or her patients. To safely administer medications, a nurse must States. Contemplating these facts makes it clear that know the answers to a range of potential questions nurses must take an approach toward medicating about his or her patients and their medications: who, patients that focuses on ensuring the right amount what, when, how, and why (TABLE 31). -

The Effect of Diclofenac Mouthwash on Periodontal Postoperative Pain
Original Article The Effect of Diclofenac Mouthwash on Periodontal Postoperative Pain Jaber Yaghini1, Ahmad Moghareh Abed2, Seyed Abolfazl Mostafavi3, Najmeh Roshanzamir4 ABSTRACT Background: The need to relieve pain and inflammation after periodontal surgery and the side effects of systemic drugs and advantages of topical drugs, made us to evaluate the effect of Diclofenac mouthwash on periodontal postoperative pain. Methods: In this double-blind, randomized clinical trial study 20 quadrants of 10 patients(n = 20) aged between 22-54 who also acted as their own controls, were treated using Modified Widman Flap procedure in two quadrants of the same jaw with one month interval between the operations. After the operation in addition to ibuprofen 400 mg, one quadrant randomly received Diclofenac mouthwash (0/01%) for 30 seconds, 4 times a day (for a week) and for the contrary quadrant, ibupro- fen and placebo mouthwash was given to be used in the same manner. The patients scored the num- ber of ibuprofen consumption and their pain intensity based on VAS index in a questionnaire in days 1, 2, 3 and the first week after operation. The findings were analysed using two-way ANOVA, t-test and Wilcoxon. P-value less than 0.05 considered to be significant. Results: There was a significant difference between the mean values of pain intensity of two quad- rants in four periods (P = 0.031). But, there was no significant difference between the average ibupro- fen consumption in two groups (P = 0.51). Postoperative satisfaction was not significantly different in two quadrants (P = 0.059). 60% of patients preferred Diclofenac mouthwash. -
Nbde Part 2 Decks and Remembed-Arroz Con Mango
ARROZ CON MANGO Dear friends, these are remembered/repeated questions (RQs) and answers I COPIED and PASTED from different discussions on Facebook. I feel sorry because I couldn’t organize the file the way I wanted but I hope it helps. Probably you’ll find some wrong answers in this file, but PLEASE … DO NOT CRITICIZE! Find out the right answer, learn it, share it, PASS your test and BE HAPPY J I wish you all the best GOD BLESS YOU! PAITO 1. All of the following are adverse effects of opioids except? diarrhea and somnolence 2. Advantage of osteogenesis distraction is? less relapse, large movements 3. An investigation that is not accurate but consistent is: reliability 4. Remineralized enamel is rough and cavitation? Dark hard and opaque 5. Characteristics of a child with autism - repetitive action, sensitive to light and noise 6. S,z,che sounds : Teeth barely touching – True 7. Something about bio-transformation, more polar and less lipid soluble? - True 8. How much of he population has herpes? 80% - (65-90% worldwide; 80-85% USA) More than 3.7 billion people under the age of 50 – or 67% of the population – are infected with herpes simplex virus type 1 (HSV-1), according to WHO's first global estimates of HSV-1 infection published today in the journal PLOS ONE. 9. Steps of plaque formation: pellicle, biofilm, materia alba, plaque 10. Dose of hydrocortisone taken per year that will indicate have adrenal insufficiency and need supplement dose for surgery - 20 mg 2 weeks for 2 years 11. Rpd clasp breakage due to what? Work hardening 12. -

Topical Treatments of Skin Pain Associated with Hidradenitis Supprurativa
UC Davis Dermatology Online Journal Title Topical treatments of skin pain: a general review with a focus on hidradenitis suppurativa with topical agents Permalink https://escholarship.org/uc/item/4m57506k Journal Dermatology Online Journal, 20(7) Author Scheinfeld, Noah Publication Date 2014 DOI 10.5070/D3207023131 License https://creativecommons.org/licenses/by-nc-nd/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Volume 20 Number 7 July 2014 Review Topical treatments of skin pain: a general review with a focus on hidradenitis suppurativa with topical agents Noah Scheinfeld MD JD Dermatology Online Journal 20 (7): 3 Assistant Clinical Professor of Dermatology Weil Cornel Medical College Correspondence: Noah Scheinfeld 150 West 55th Street NYC NY 10019 (212) 991-6490 [email protected] Abstract Hidradenitis Supprurativa (HS) is a painful chronic follicular disease. Few papers have addressed pain control for this debilitating condition. Possible topical agents include tricyclic antidepressants, opioids, anticonvulsants, NSAIDs, NMDA receptor antagonists, local anesthetics and other agents. The first line agents for the topical treatment of the cutaneous pain of HS are diclonefac gel 1% and liposomal xylocaine 4% and 5% cream or 5% ointment. The chief advantage of topical xylocaine is that is quick acting i.e. immediate however with a limited duration of effect 1-2 hours. The use of topical ketamine, which blocks n- methyl-D-aspartate receptors in a non-competitive fashion, might be a useful tool for the treatment of HS pain. Topical doxepin, which available in a 5% commercially preparation (Zonalon®) , makes patients drowsy and is not useful for controlling the pain of HS . -

Clinical Effectiveness of Compounded Topical Medications in Oral Medicine: a Meta-Analysis
Margono et al. Stomatological Dis Sci 2020;4:3 Stomatological DOI: 10.20517/2573-0002.2019.18 Disease and Science Meta-Analysis Open Access Clinical effectiveness of compounded topical medications in oral medicine: a meta-analysis Her Basuki Margono1, Irna Sufiawati2 1Oral Medicine Residency Program, Faculty of Dentistry, Padjadjaran University, Bandung 40132, West Java, Indonesia. 2Department of Oral Medicine, Faculty of Dentistry, Padjadjaran University, Bandung 40132, West Java, Indonesia. Correspondence to: Dr. Irna Sufiawati, Department of Oral Medicine, Faculty of Dentistry, Padjadjaran University: Jl. Sekeloa Selatan I, Bandung 40132, West Java, Indonesia. E-mail: [email protected] How to cite this article: Margono HB, Sufiawati I. Clinical effectiveness of compounded topical medications in oral medicine: a meta-analysis. Stomatological Dis Sci 2020;4:3. http://dx.doi.org/10.20517/2573-0002.2019.18 Received: 16 Oct 2019 First Decision: 11 Nov 2019 Revised: 14 May 2020 Accepted: 21 Jul 2020 Published: 19 Aug 2020 Academic Editor: Letizia Perillo Copy Editor: Cai-Hong Wang Production Editor: Jing Yu Abstract Aim: To assess the evidence of the efficacy and safety of compounded topical medications in oral medicine cases. Methods: Electronic databases were searched from inception to October 2019 for studies that evaluated compounded topical medications in oral medicine cases to assess their efficacy and safety. Search terms included drug compounding, topical administration, clinical efficacy, and oral lesions. Only randomized controlled trials (RCTs) or cross-over trials of compounded topical drug versus non-compounded drug or placebo or standard treatment were included. The exclusion criteria included compounded topical medications with herbal ingredients in the intervention group to compare with the non-compounded drug. -

Allergic and Immunologic Response of the Oral Mucosa: an Overview Snehashish Ghosh1, Shwetha Nambiar1, Shankargouda Patil2, Vanishri C
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by eDENT Journals International Journal of Clinical Dental Sciences (2016), 6, 1–7 REVIEW ARTICLE Allergic and immunologic response of the oral mucosa: An overview Snehashish Ghosh1, Shwetha Nambiar1, Shankargouda Patil2, Vanishri C. Haragannavar1, Dominic Augustine1, Sowmya S.V1, Roopa S. Rao1 1Department of Oral Pathology & Microbiology, Faculty of Dental Sciences, M.S. Ramaiah University of Applied Sciences, Bengaluru, Karnataka, India, 2Department of Maxillofacial Surgery and Diagnostic Sciences, Division of Oral Pathology, College of Dentistry, Jazan University, Jazan, Saudi Arabia Keywords Abstract Allergic disease, diagnosis, oral lesions, Allergic and immunologic diseases very often manifest oral lesions in their earliest pathogenesis stages, an early diagnosis, which may be spurred by a dental examination, is a key for improved outcomes. After systemic diagnosis, oral lesions benefi t from special care Correspondence Dr. Snehashish Ghosh, Department of Oral by dentists in alliance with the medical team. This review aims to highlight the most Pathology & Microbiology, Faculty of Dental relevant allergic and immunologic conditions of the oral cavity, their pathogenesis, and Sciences, M.S. Ramaiah University of Applied their pathognomonic diagnostic features, which will navigate the clinicians to arrive at a Sciences, M.S.R.I.T. Post, MSR Nagar, prompt diagnosis and subsequent management. Bengaluru - 560 054, Karnataka, India. Email: [email protected] Received 12 January 2016; Accepted 14 June 2016 doi: 10.15713-ins-ijcds-07-01 Introduction emergence of immunotherapeutics will help to ameliorate these diseases.[2] An allergy is defi ned as an altered or changed response of the immune system to foreign proteins. -

Short-Contact Clobetasol Propionate Shampoo 0.05% Improves Quality of Life in Patients with Scalp Psoriasis
THERAPEUTICS FOR THE CLINICIAN Short-Contact Clobetasol Propionate Shampoo 0.05% Improves Quality of Life in Patients With Scalp Psoriasis Jerry Tan, MD, FRCPC; Richard Thomas, MD; Béatrice Wang, MD; David Gratton, MD; Ronald Vender, MD; Nabil Kerrouche, MSc; Hervé Villemagne, MSc; for the CalePso Study Team Scalp psoriasis has a considerable impact on the on their QOL increased from 45.6% at baseline to quality of life (QOL) of patients, and most patients 81.7% at week 4. Most participants were satisfied are dissatisfied with available treatments. Clo- with the cosmetic acceptability and the efficacy betasol propionate shampoo 0.05% has been and safety aspects of the product, considered shown to be effective and safe for moderate to it better than prior treatments, and would use it severe scalp psoriasis. We evaluated the effect again in the future. Therefore, we conclude that of clobetasol propionate shampoo on QOL and treatment with clobetasol propionate shampoo the degree of participant satisfaction with the improved the QOL of participants and resulted in product. Participants received once-daily treat- high satisfaction. ment for up to 4 weeks. Their QOL and degree Cutis. 2009;83:157-164. of satisfaction were evaluated by questionnaires. The mean (standard deviation) Dermatology Life Quality Index (DLQI) score decreased signifi- calp psoriasis is a common inflammatory disease cantly from 7.0 (4.9) at baseline to 3.2 (3.2) at that has a considerable impact on the quality of week 4 (P,.001). Participants who considered S life (QOL) of patients because of its associated the disease as having a small effect or no effect pruritus, the visibility of lesions, and the chronicity of disease.1 Approximately 50% of patients in one Accepted for publication January 26, 2009. -

1: Oral Mucosa Diseases in Dogs: How Helpful Are The
Oral mucosal diseases in dogs: How helpful are the fundamentals of dermatopathology? Cynthia M. Bell, MS, DVM, Diplomate ACVP Associate Professor, Kansas State University Manhattan, KS, USA [email protected] The objective of this presentation is to provide a broad overview of stomatitis in dogs, including immune-mediated mucosal and mucocutaneous diseases. There is little emphasis on gingivitis since this condition is so often related to primary dental and periodontal disease. Particular attention is given to regionally extensive or generalized oral mucosal inflammation, with emphasis on distinguishing features that will help the pathologist formulate and rank a differential diagnosis. Oral mucosal diseases in dogs • Plaque-associated stomatitis/CUPS • Immune-mediated/autoimmune diseases o Skin diseases with oral involvement § Pemphigus vulgaris § Mucous membrane pemphigoid § Paraneoplastic pemphigoid § Erythema multiforme § Lupus erythematosus, mostly DLE o Chronic stomatitis • Mucosal drug eruption • Other infectious (Candidiasis, acute viral infection) • Other non-infectious causes (thermal or chemical burn, uremia) • Neoplasia (e.g. epitheliotropic T cell lymphoma) Plaque-associated stomatitis (aka. contact stomatitis, CUPS) The most singular form of stomatitis in dogs has, for the past ~20 years, been referred to as CUPS (canine ulcerative paradental stomatitis). As a disease entity, CUPS was conceived within the clinical setting; therefore, many pathologists may not be aware of or have only a casual familiarity with the syndrome. It is common for dogs to develop oral mucosal ulcerations (“kissing lesions”) at sites of contact—usually where the buccal mucosa and lateral lingual mucosa contacts the larger tooth surfaces (i.e. canine teeth and carnassial teeth). 1 This condition is thought to be an exaggerated immune-mediated inflammatory response to plaque on the tooth surface (“plaque intolerance”), therefore, “plaque associated stomatitis” is a term that is favored by many veterinarians, myself included.