1: Oral Mucosa Diseases in Dogs: How Helpful Are The
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Practice Statements-Oral Contact Allergy
Clinical Practice Statements-Oral Contact Allergy Subject: Oral Contact Allergy The American Academy of Oral Medicine (AAOM) affirms that oral contact allergy (OCA) is an oral mucosal response that may be associated with materials and substances found in oral hygiene products, common food items, and topically applied agents. The AAOM also affirms that patients with suspected OCA should be referred to the appropriate dental and/or medical health care provider(s) for comprehensive evaluation and management of the condition. Replacement and/or substitution of dental materials should be considered only if (1) a reasonable temporal association has been established between the suspected triggering material and development of clinical signs and/or symptoms, (2) clinical examination supports an association between the suspected triggering material and objective clinical findings, and (3) diagnostic testing (e.g., dermatologic patch testing, skin-prick testing) confirms a hypersensitivity reaction to the suspected offending material. Originators: Dr. Eric T. Stoopler, DMD, FDS RCSEd, FDS RCSEng, Dr. Scott S. De Rossi, DMD. This Clinical Practice Statement was developed as an educational tool based on expert consensus of the American Academy of Oral Medicine (AAOM) leadership. Readers are encouraged to consider the recommendations in the context of their specific clinical situation, and consult, when appropriate, other sources of clinical, scientific, or regulatory information prior to making a treatment decision. Originator: Dr. Eric T. Stoopler, DMD, FDS RCSEd, FDS RCSEng, Dr. Scott S. De Rossi, DMD Review: AAOM Education Committee Approval: AAOM Executive Committee Adopted: October 17, 2015 Updated: February 5, 2016 Purpose The AAOM affirms that oral contact allergy (OCA) is an oral mucosal response that may be associated with materials and substances found in oral hygiene products, common food items, and topically applied agents. -

White Lesions of the Oral Cavity and Derive a Differential Diagnosis Four for Various White Lesions
2014 self-study course four course The Ohio State University College of Dentistry is a recognized provider for ADA, CERP, and AGD Fellowship, Mastership and Maintenance credit. ADA CERP is a service of the American Dental Association to assist dental professionals in identifying quality providers of continuing dental education. ADA CERP does not approve or endorse individual courses or instructors, nor does it imply acceptance of credit hours by boards of dentistry. Concerns or complaints about a CE provider may be directed to the provider or to ADA CERP at www.ada.org/goto/cerp. The Ohio State University College of Dentistry is approved by the Ohio State Dental Board as a permanent sponsor of continuing dental education ABOUT this FREQUENTLY asked COURSE… QUESTIONS… Q: Who can earn FREE CE credits? . READ the MATERIALS. Read and review the course materials. A: EVERYONE - All dental professionals in your office may earn free CE contact . COMPLETE the TEST. Answer the credits. Each person must read the eight question test. A total of 6/8 course materials and submit an questions must be answered correctly online answer form independently. for credit. us . SUBMIT the ANSWER FORM Q: What if I did not receive a ONLINE. You MUST submit your confirmation ID? answers ONLINE at: A: Once you have fully completed your p h o n e http://dent.osu.edu/sterilization/ce answer form and click “submit” you will be directed to a page with a . RECORD or PRINT THE 614-292-6737 unique confirmation ID. CONFIRMATION ID This unique ID is displayed upon successful submission Q: Where can I find my SMS number? of your answer form. -

Features of Reactive White Lesions of the Oral Mucosa
Head and Neck Pathology (2019) 13:16–24 https://doi.org/10.1007/s12105-018-0986-3 SPECIAL ISSUE: COLORS AND TEXTURES, A REVIEW OF ORAL MUCOSAL ENTITIES Frictional Keratosis, Contact Keratosis and Smokeless Tobacco Keratosis: Features of Reactive White Lesions of the Oral Mucosa Susan Müller1 Received: 21 September 2018 / Accepted: 2 November 2018 / Published online: 22 January 2019 © Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract White lesions of the oral cavity are quite common and can have a variety of etiologies, both benign and malignant. Although the vast majority of publications focus on leukoplakia and other potentially malignant lesions, most oral lesions that appear white are benign. This review will focus exclusively on reactive white oral lesions. Included in the discussion are frictional keratoses, irritant contact stomatitis, and smokeless tobacco keratoses. Leukoedema and hereditary genodermatoses that may enter in the clinical differential diagnoses of frictional keratoses including white sponge nevus and hereditary benign intraepithelial dyskeratosis will be reviewed. Many products can result in contact stomatitis. Dentrifice-related stomatitis, contact reactions to amalgam and cinnamon can cause keratotic lesions. Each of these lesions have microscopic findings that can assist in patient management. Keywords Leukoplakia · Frictional keratosis · Smokeless tobacco keratosis · Stomatitis · Leukoedema · Cinnamon Introduction white lesions including infective and non-infective causes will be discussed -
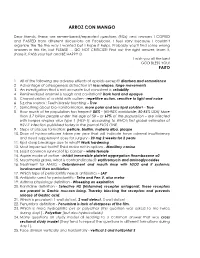
Nbde Part 2 Decks and Remembed-Arroz Con Mango
ARROZ CON MANGO Dear friends, these are remembered/repeated questions (RQs) and answers I COPIED and PASTED from different discussions on Facebook. I feel sorry because I couldn’t organize the file the way I wanted but I hope it helps. Probably you’ll find some wrong answers in this file, but PLEASE … DO NOT CRITICIZE! Find out the right answer, learn it, share it, PASS your test and BE HAPPY J I wish you all the best GOD BLESS YOU! PAITO 1. All of the following are adverse effects of opioids except? diarrhea and somnolence 2. Advantage of osteogenesis distraction is? less relapse, large movements 3. An investigation that is not accurate but consistent is: reliability 4. Remineralized enamel is rough and cavitation? Dark hard and opaque 5. Characteristics of a child with autism - repetitive action, sensitive to light and noise 6. S,z,che sounds : Teeth barely touching – True 7. Something about bio-transformation, more polar and less lipid soluble? - True 8. How much of he population has herpes? 80% - (65-90% worldwide; 80-85% USA) More than 3.7 billion people under the age of 50 – or 67% of the population – are infected with herpes simplex virus type 1 (HSV-1), according to WHO's first global estimates of HSV-1 infection published today in the journal PLOS ONE. 9. Steps of plaque formation: pellicle, biofilm, materia alba, plaque 10. Dose of hydrocortisone taken per year that will indicate have adrenal insufficiency and need supplement dose for surgery - 20 mg 2 weeks for 2 years 11. Rpd clasp breakage due to what? Work hardening 12. -

Allergic and Immunologic Response of the Oral Mucosa: an Overview Snehashish Ghosh1, Shwetha Nambiar1, Shankargouda Patil2, Vanishri C
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by eDENT Journals International Journal of Clinical Dental Sciences (2016), 6, 1–7 REVIEW ARTICLE Allergic and immunologic response of the oral mucosa: An overview Snehashish Ghosh1, Shwetha Nambiar1, Shankargouda Patil2, Vanishri C. Haragannavar1, Dominic Augustine1, Sowmya S.V1, Roopa S. Rao1 1Department of Oral Pathology & Microbiology, Faculty of Dental Sciences, M.S. Ramaiah University of Applied Sciences, Bengaluru, Karnataka, India, 2Department of Maxillofacial Surgery and Diagnostic Sciences, Division of Oral Pathology, College of Dentistry, Jazan University, Jazan, Saudi Arabia Keywords Abstract Allergic disease, diagnosis, oral lesions, Allergic and immunologic diseases very often manifest oral lesions in their earliest pathogenesis stages, an early diagnosis, which may be spurred by a dental examination, is a key for improved outcomes. After systemic diagnosis, oral lesions benefi t from special care Correspondence Dr. Snehashish Ghosh, Department of Oral by dentists in alliance with the medical team. This review aims to highlight the most Pathology & Microbiology, Faculty of Dental relevant allergic and immunologic conditions of the oral cavity, their pathogenesis, and Sciences, M.S. Ramaiah University of Applied their pathognomonic diagnostic features, which will navigate the clinicians to arrive at a Sciences, M.S.R.I.T. Post, MSR Nagar, prompt diagnosis and subsequent management. Bengaluru - 560 054, Karnataka, India. Email: [email protected] Received 12 January 2016; Accepted 14 June 2016 doi: 10.15713-ins-ijcds-07-01 Introduction emergence of immunotherapeutics will help to ameliorate these diseases.[2] An allergy is defi ned as an altered or changed response of the immune system to foreign proteins. -

5 Allergic Diseases (And Differential Diagnoses)
Chapter 5 5 Allergic Diseases (and Differential Diagnoses) 5.1 Diseases with Possible IgE Involve- tions (combination of type I and type IVb reac- ment (“Immediate-Type Allergies”) tions). Atopic eczema will be discussed in a separate section (see Sect. 5.5.3). There are many allergic diseases manifesting in The maximal manifestation of IgE-mediated different organs and on the basis of different immediate-type allergic reaction is anaphylax- pathomechanisms (see Sect. 1.3). The most is. In the development of clinical symptoms, common allergies develop via IgE antibodies different organs may be involved and symp- and manifest within minutes to hours after al- toms of well-known allergic diseases of skin lergen contact (“immediate-type reactions”). and mucous membranes [also called “shock Not infrequently, there are biphasic (dual) re- fragments” (Karl Hansen)] may occur accord- action patterns when after a strong immediate ing to the severity (see Sect. 5.1.4). reactioninthecourseof6–12harenewedhy- persensitivity reaction (late-phase reaction, LPR) occurs which is triggered by IgE, but am- 5.1.1 Allergic Rhinitis plified by recruitment of additional cells and 5.1.1.1 Introduction mediators.TheseLPRshavetobedistin- guished from classic delayed-type hypersensi- Apart from being an aesthetic organ, the nose tivity (DTH) reactions (type IV reactions) (see has several very interesting functions (Ta- Sect. 5.5). ble 5.1). It is true that people can live without What may be confusing for the inexperi- breathing through the nose, but disturbance of enced physician is familiar to the allergist: The this function can lead to disease. Here we are same symptoms of immediate-type reactions interested mostly in defense functions against are observed without immune phenomena particles and irritants (physical or chemical) (skin tests or IgE antibodies) being detectable. -

Allergy and Oral Mucosal Disease
Allergy and Oral Mucosal Disease Shiona Rachel Rees B.D.S. F.D.S. R.C.P.S. A thesis presented for the degree of Doctor of Dental Surgery of the University of Glasgow Faculty of Medicine University of Glasgow Glasgow Dental Hospital & School May 2001 © Shiona Rachel Rees, May 2001 ProQuest Number: 13833984 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a com plete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest ProQuest 13833984 Published by ProQuest LLC(2019). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States C ode Microform Edition © ProQuest LLC. ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106- 1346 fGLASGOW UNIVERSITY .LIBRARY: \ 1 ^ 5 SUMMARY The purpose of this study was to assess the prevalence of positive results to cutaneous patch testing in patients with oral mucosal diseases and to assess the relevance of exclusion of identified allergens to the disease process. It was also attempted to identify microscopic features that were related to a hypersensitivity aetiology in patients with oral lichenoid eruptions. The analysis was carried out retrospectively in the Departments of Oral Medicine and Oral Pathology in Glasgow Dental Hospital And School and the Contact Dermatitis Investigation Unit in the Royal Infirmary, Glasgow. -

Statistical Analysis Plan
Cover Page for Statistical Analysis Plan Sponsor name: Novo Nordisk A/S NCT number NCT03061214 Sponsor trial ID: NN9535-4114 Official title of study: SUSTAINTM CHINA - Efficacy and safety of semaglutide once-weekly versus sitagliptin once-daily as add-on to metformin in subjects with type 2 diabetes Document date: 22 August 2019 Semaglutide s.c (Ozempic®) Date: 22 August 2019 Novo Nordisk Trial ID: NN9535-4114 Version: 1.0 CONFIDENTIAL Clinical Trial Report Status: Final Appendix 16.1.9 16.1.9 Documentation of statistical methods List of contents Statistical analysis plan...................................................................................................................... /LQN Statistical documentation................................................................................................................... /LQN Redacted VWDWLVWLFDODQDO\VLVSODQ Includes redaction of personal identifiable information only. Statistical Analysis Plan Date: 28 May 2019 Novo Nordisk Trial ID: NN9535-4114 Version: 1.0 CONFIDENTIAL UTN:U1111-1149-0432 Status: Final EudraCT No.:NA Page: 1 of 30 Statistical Analysis Plan Trial ID: NN9535-4114 Efficacy and safety of semaglutide once-weekly versus sitagliptin once-daily as add-on to metformin in subjects with type 2 diabetes Author Biostatistics Semaglutide s.c. This confidential document is the property of Novo Nordisk. No unpublished information contained herein may be disclosed without prior written approval from Novo Nordisk. Access to this document must be restricted to relevant parties.This -

Oral Lesions and Contact Allergy -Clinical, Histopathological, Molecular Biological and Immunological Investigations
S e c t i o n o f Oral Pathology and Oral Medicine Department of Odontology UNIVERSITY OF COPENH AGEN FACULTY OF HEALTH AN D MEDICAL SCIENCES Oral lesions and contact allergy -clinical, histopathological, molecular biological and immunological investigations Kristine Røn Larsen PhD Thesis December 2016 This thesis has been submitted to the Graduate School of The Faculty of Health and Medical nd Sciences, University of Copenhagen December 2 2016 1 Evaluation committee Chairperson Associate Professor, PhD Ana Raquel Benetti University of Copenhagen Faculty of Health and Medical Sciences Department of Odontology Copenhagen, Denmark Assessor Professor, Dr. Med. Dent. Gottfried Schmalz University of Regensburg Faculty of Medicine Regensburg, Germany Assessor Professor, PhD Anne Christine Johannessen University of Bergen Faculty of Medicine and Dentistry Bergen, Norway 2 Table of contents Preface ……………………………………………………………………………………………………………..………………………… 5 Financial support ……………………………………………………………………………………………………………..…….. 6 Acknowledgements ……………………………………………………………………………………………………………….... 7 List of abbreviations ……………………………………………………………………………………………………………..…. 8 Summary ……………………………………………………………………………………………………………………………..……. 9 Summary in Danish …………………………………………………………………………………………………………….……. 11 Introduction ………………………………………………………………………………………………………………………..…… 13 Background ………………………………………………………………………………………………………………………..……. 14 The oral cavity ………………………………………………………………………………………………………………..…….. 14 The oral mucosa ……………………………………………………………………………………………………………….….. 14 Saliva -

Adverse Effects of Medicinal and Non-Medicinal Substances
Benign? Not So Fast: Challenging Oral Diseases presented with DDX June 21st 2018 Dolphine Oda [email protected] Tel (206) 616-4748 COURSE OUTLINE: Five Topics: 1. Oral squamous cell carcinoma (SCC)-Variability in Etiology 2. Oral Ulcers: Spectrum of Diseases 3. Oral Swellings: Single & Multiple 4. Radiolucent Jaw Lesions: From Benign to Metastatic 5. Radiopaque Jaw Lesions: Benign & Other Oral SCC: Tobacco-Associated White lesions 1. Frictional white patches a. Tongue chewing b. Others 2. Contact white patches 3. Smoker’s white patches a. Smokeless tobacco b. Cigarette smoking 4. Idiopathic white patches Red, Speckled lesions 5. Erythroplakia 6. Georgraphic tongue 7. Median rhomboid glossitis Deep Single ulcers 8. Traumatic ulcer -TUGSE 9. Infectious Disease 10. Necrotizing sialometaplasia Oral Squamous Cell Carcinoma: Tobacco-associated If you suspect that a lesion is malignant, refer to an oral surgeon for a biopsy. It is the most common type of oral SCC, which accounts for over 75% of all malignant neoplasms of the oral cavity. Clinically, it is more common in men over 55 years of age, heavy smokers and heavy drinkers, more in males especially black males. However, it has been described in young white males, under the age of fifty non-smokers and non-drinkers. The latter group constitutes less than 5% of the patients and their SCCs tend to be in the posterior mouth (oropharynx and tosillar area) associated with HPV infection especially HPV type 16. The most common sites for the tobacco-associated are the lateral and ventral tongue, followed by the floor of mouth and soft palate area. -

Oral Lichenoid Lesions Related to Contact with Dental Materials: a Literature Review
Med Oral Patol Oral Cir Bucal. 2009 Oct 1;14 (10):e514-20. Oral lichenoid lesions related to dental materials Journal section: Oral Medicine and Pathology doi:10.4317/medoral.14.e514 Publication Types: Review Oral lichenoid lesions related to contact with dental materials: A literature review María-José Cobos-Fuentes 1, Ángel Martínez-Sahuquillo-Márquez 2, Isabel Gallardo-Castillo 3, Jose-Ramón Armas-Padrón 4, Ana Moreno-Fernández 4, Pedro Bullón-Fernández 5 1 Associate Professor of Oral Medicine; Faculty of Dentistry; University of Seville 2 Full-time Professor of Oral Medicine; Faculty of Dentistry; University of Seville 3 Visiting Professor of Oral Medicine; Faculty of Dentistry; University of Seville 4 Full-time Professor of Pathological Anatomy; Department of Cell Biology and Normal or Pathological Histology; University of Seville 5 Professor of Oral Medicine and Periodontology; University of Seville Correspondence: Facultad de Odontología Universidad de Sevilla Cobos-Fuentes MJ, Martínez-Sahuquillo-Márquez A, Gallardo-Castillo C/. Avicena, s/n I, Armas-Padrón JR, Moreno-Fernández A, Bullón-Fernández P. Oral 41009 Sevilla (Spain) lichenoid lesions related to contact with dental materials: A literature re- [email protected] view. Med Oral Patol Oral Cir Bucal. 2009 Oct 1;14 (10):e514-20. http://www.medicinaoral.com/medoralfree01/v14i10/medoralv14i10p514.pdf Article Number: 2002 http://www.medicinaoral.com/ Received: 21/11/2008 © Medicina Oral S. L. C.I.F. B 96689336 - pISSN 1698-4447 - eISSN: 1698-6946 Accepted: 07/07/2009 eMail: [email protected] Indexed in: -SCI EXPANDED -JOURNAL CITATION REPORTS -Index Medicus / MEDLINE / PubMed -EMBASE, Excerpta Medica -SCOPUS -Indice Médico Español Abstract Oral lichenoid lesions related to contact are defined as oral-cavity eruptions with an identifiable etiology, and are clinically and histologically similar to oral lichen planus. -

Contact Stomatitis to Toothpaste: Importance of Differential Diagnosis
Revista Brasileira de Odontologia Brazilian Journal of Dentistry Associação Brasileira de Odontologia - Seção Rio de Janeiro DOI: http://dx.doi.org/10.18363/rbo.v76.2019.e1375 Short Communication/Oral Pathology and Stomatology Contact stomatitis to toothpaste: importance of differential diagnosis Simone Macedo Amaral,1 Águida Maria Menezes Aguiar Miranda,1,2 Juliana de Noronha Santos Netto,1,2 Fábio Ramôa Pires1,2,3 1Brazilian Dental Association – Rio de Janeiro Section (ABO), RJ, Brazil 2School of Dentistry, Estácio de Sá University, RJ, Brazil 3Department of Diagnosis and Therapeutics, School of Dentistry, Rio de Janeiro State University (UERJ), RJ, Brazil • Conflicts of interest: none declared. ABSTRACT Objective: the aim of the present study is to report four cases of toothpaste-related contact stomatitis focusing on their clinical presentation and the importance of differential diagnosis with other reactive, inflammatory and potentially malignant disorders of the oral cavity. Case report: the four cases affected adult females and presented as multifocal whitish and/or erythematous patches and plaques affecting the tongue, floor of mouth, and labial mucosa, showing mild burning sensation, and lasting 7 to 15 days. All patients reported starting the use of new toothpastes few days before the onset of the symptoms and all lesions disappeared in 5 to 7 days after suspension of its use. Conclusion: contact stomatitis to toothpastes should be considered in the differential diagnosis of oral white and red patches and plaques, and detailed clinical history is essential for prompt and correct final diagnosis. As the use of new oral rinses, toothpastes and other oral hygiene products is increasing, clini- cians should be aware of the possibility of oral local reactions associated with their use.