Oral Mucosal Lesions Associated with Use of Quid
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Rebamipide to Manage Stomatopyrosis in Oral Submucous Fibrosis 1Joanna Baptist, 2Shrijana Shakya, 3Ravikiran Ongole
JCDP Rebamipide to Manage Stomatopyrosis10.5005/jp-journals-10024-1972 in Oral Submucous Fibrosis ORIGINAL RESEARCH Rebamipide to Manage Stomatopyrosis in Oral Submucous Fibrosis 1Joanna Baptist, 2Shrijana Shakya, 3Ravikiran Ongole ABSTRACT Source of support: Nil Introduction: Oral submucous fibrosis (OSF) causes progres- Conflict of interest: None sive debilitating symptoms, such as oral burning sensation (sto- matopyrosis) and limited mouth opening. The standard of care INTRODUCTION (SOC) protocol includes habit cessation, intralesional steroid and hyaluronidase injections, and mouth opening exercises. The Oral submucous fibrosis (OSF) is commonly seen in objective of the study was to evaluate efficacy of rebamipide the Indian subcontinent affecting individuals of all age in alleviating burning sensation of the oral mucosa in OSF in groups. It is a potentially malignant disorder caused comparison with SOC intralesional steroid injections. almost exclusively by the use of smokeless form of Materials and methods: Twenty OSF patients were divided into tobacco products. The malignant transformation rates two groups [rebamipide (100 mg TID for 21 days) and betametha- vary from 3 to 19%.1,2 sone (4 mg/mL biweekly for 4 weeks)] of 10 each by random Oral submucous fibrosis causes progressive debilitat- sampling. Burning sensation was assessed every week for 1 month. Burning sensation scores were analyzed using repeated ing symptoms affecting the oral cavity, such as burning measures analysis of variance (ANOVA) and paired t-test. sensation, loss of cheek elasticity, restricted tongue move- Results: Change in burning sensation score was significant ments, and limited mouth opening. Oral submucous (p < 0.05) in the first four visits. However, score between the fibrosis is an irreversible condition and the management 4th and 5th visit was not statistically significant (p > 0.05). -

Harm Reduction Journal Biomed Central
Harm Reduction Journal BioMed Central Research Open Access My first time: initiation into injecting drug use in Manipur and Nagaland, north-east India Michelle Kermode*1, Verity Longleng2, Bangkim Chingsubam Singh2, Jane Hocking3, Biangtung Langkham2 and Nick Crofts1 Address: 1Nossal Institute for Global Health, University of Melbourne, Carlton, Victoria, Australia, 2c/- Project ORCHID, CBCNEI Mission Compound, Guwahati, Assam, India and 3Key Centre for Women's Health, University of Melbourne, Carlton, Victoria, Australia Email: Michelle Kermode* - [email protected]; Verity Longleng - [email protected]; Bangkim Chingsubam Singh - [email protected]; Jane Hocking - [email protected]; Biangtung Langkham - [email protected]; Nick Crofts - [email protected] * Corresponding author Published: 5 December 2007 Received: 3 July 2007 Accepted: 5 December 2007 Harm Reduction Journal 2007, 4:19 doi:10.1186/1477-7517-4-19 This article is available from: http://www.harmreductionjournal.com/content/4/1/19 © 2007 Kermode et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Background: The north-east Indian states of Manipur and Nagaland are two of the six high HIV prevalence states in the country, and the main route of HIV transmission is injecting drug use. Understanding the pathways to injecting drug use can facilitate early intervention with HIV prevention programs. While several studies of initiation into injecting drug use have been conducted in developed countries, little is known about the situation in developing country settings. -

Zeroing in on the Cause of Your Patient's Facial Pain
Feras Ghazal, DDS; Mohammed Ahmad, Zeroing in on the cause MD; Hussein Elrawy, DDS; Tamer Said, MD Department of Oral Health of your patient's facial pain (Drs. Ghazal and Elrawy) and Department of Family Medicine/Geriatrics (Drs. Ahmad and Said), The overlapping characteristics of facial pain can make it MetroHealth Medical Center, Cleveland, Ohio difficult to pinpoint the cause. This article, with a handy at-a-glance table, can help. [email protected] The authors reported no potential conflict of interest relevant to this article. acial pain is a common complaint: Up to 22% of adults PracticE in the United States experience orofacial pain during recommendationS F any 6-month period.1 Yet this type of pain can be dif- › Advise patients who have a ficult to diagnose due to the many structures of the face and temporomandibular mouth, pain referral patterns, and insufficient diagnostic tools. disorder that in addition to Specifically, extraoral facial pain can be the result of tem- taking their medication as poromandibular disorders, neuropathic disorders, vascular prescribed, they should limit disorders, or atypical causes, whereas facial pain stemming activities that require moving their jaw, modify their diet, from inside the mouth can have a dental or nondental cause and minimize stress; they (FIGURE). Overlapping characteristics can make it difficult to may require physical therapy distinguish these disorders. To help you to better diagnose and and therapeutic exercises. C manage facial pain, we describe the most common causes and underlying pathological processes. › Consider prescribing a tricyclic antidepressant for patients with persistent idiopathic facial pain. C Extraoral facial pain Extraoral pain refers to the pain that occurs on the face out- 2-15 Strength of recommendation (SoR) side of the oral cavity. -

Immediate Effect of Tobacco Chewing in the Form of 'Paan'
April-June 1988 Ind. J. Physiol. Pharmac. e and high altitude stress on humans. behaviour and pituitary adrenal axis IMMEDIATE EFFECT OF TOBACCO CHEWING IN THE FORM of corticosteroids in lactating goats OF 'PAAN' ON CERTAIN CARDIO-RESPIRATORY PARAMETERS r lactating rats : Parallel changes P. K. NANDA AND M. M. SHARMA I-hydroxy corticosteroids in human Department of Physiology, Indira Gandhi Medical College, Shimla - 171 001 on serum transaminase and lactic of Physiological Sciences, New Delhi (Received on May 17, 1987 ) ofstress on serum enzyme levels in Summary: Immediate effect of tobacco in the form of chewing was evaluated in 40 healthy males (mean age 26.27 yrs.) not habituated to tobacco, who were given paan containing 200 mg of of drug metabolizing enzymes and tobacco to chew (group T). Heart rate (HR), blood pressure (BP), forced vital capacity (FVC), nal stress, Ind. J. Med, Res., 83 : FEV} and peak expiratory flow rate (PEFR) were measured twice for each subject, once before chewing and again immediately after completion of chewing. Another 24 age and sex matched ry and clearace in sheep before and controls (group C) were given paan without tobacco to chew and cardiorespiratory parameters 1970. were recorded as for group T subjects. Electrocardiography was recorded in lO group T and 10 ase Process" Ed. J. M. Raamsey , group C subjects. Effect of tobacco chewing was also evaluated in 10 habitual tobacco chewers. Results showed statistically significant increments in HR and BP as well as a decline in T wave of serum Glutamic oxalacetic and amplitude in ECG following tobacco chewing (group T subjects). -

IMS Data Reference Tables
IMS REFERENCE DATA – VERSION 1.7 TABLES 1. Substance .............................................................................................................................................................................. 2 2. Local Authority ....................................................................................................................................................................... 6 3. Drug Action Team (DAT) ...................................................................................................................................................... 13 4. Nationality ........................................................................................................................................................................... 17 5. Ethnicity ............................................................................................................................................................................... 22 6. Sexual Orientation ............................................................................................................................................................... 22 7. Religion or Belief .................................................................................................................................................................. 22 8. Employment Status .............................................................................................................................................................. 23 9. Accommodation Status -

OCTOBER 2019 Network Bulletin an Important Message from Unitedhealthcare to Health Care Professionals and Facilities
OCTOBER 2019 network bulletin An important message from UnitedHealthcare to health care professionals and facilities. Enter UnitedHealthcare respects the expertise of the physicians, health care professionals and their staff who participate in our network. Our goal is to support you and your patients in making the most informed decisions regarding the choice of quality and cost-effective care, and to support practice staff with a simple and predictable administrative experience. The Network Bulletin was developed to share important updates regarding UnitedHealthcare procedure and policy changes, as well as other useful administrative and clinical information. Where information in this bulletin conflicts with applicable state and/or federal law, UnitedHealthcare follows such applicable federal and/or state law. UnitedHealthcare Network Bulletin October 2019 Table of Contents Front & Center PAGE 3 Stay up to date with the latest news and information. UnitedHealthcare Commercial PAGE 22 Learn about program revisions and requirement updates. UnitedHealthcare Community Plan PAGE 29 Learn about Medicaid coverage changes and updates. UnitedHealthcare Medicare Advantage PAGE 35 Learn about Medicare policy, reimbursement and guideline changes. UnitedHealthcare Affiliates PAGE 37 Learn about updates with our company partners. PREV NEXT 2 | For more information, call 877-842-3210 or visit UHCprovider.com. UnitedHealthcare Network Bulletin October 2019 Table of Contents Front & Center Stay up to date with the latest news and information. Smart Edits Help Speed Up Radiology Program Outpatient Injectable Your Claims Cycle Procedure Code Changes Chemotherapy and Our Smart Edits claims tool catches Effective Jan. 1, 2020, Related Cancer Therapies errors and gives you an opportunity UnitedHealthcare will update Prior Authorization/ to resolve and resubmit a claim the procedure code list for the Notification Updates before it enters the claims cycle. -

Download Download
628 Indian Journal of Forensic Medicine & Toxicology, July-September 2021, Vol. 15, No. 3 Tongue Lesions - A Review N.Anitha1, Dharini Jayachandran2 1Reader, Department of Oral Pathology and Microbiology,2Undergraduate Student, Sree Balaji Dental College and Hospital, Bharath Institute of Higher Education and Research Abstract Tongue is a vital organ within the oral cavity that has varied function,and it may act as an index for the underlying systemic diseases.The investigation of the tongue diseases may begin with mere clinical examination .This review is to highlight the signs and symptoms of the various lesions that affects the tongue and especially to talk in brief about the benign and malignant tumours that affect the tongue along with other inherited and congenital abnormalities.Tongue lesions are categorized as tumours,infections, reactionary,congenital,developmental,acquired,autoimmune and potentially malignant disorders for easy understanding and to arrive at appropriate diagnosis.Tongue playing an important role in maintaining the harmony in the oral environment,it should be treated from diseases. Keywords: Tongue lesions,benign tumours,malignant tumours,diseases of tongue. CLASSIFICATION OF LESIONS ● Pyogenic granuloma AFFECTING THE TONGUE. ● Frictional keratosis BENIGN TUMOURS OF THE TONGUE INFECTIOUS LESIONS OF TONGUE ● Capillary hemangioma ● Oral squamous papilloma ● Fibroma ● Oral hairy leukoplakia ● Cavernous hemangioma ● Candidiasiis ● Giant cell granuloma ● Median rhomboid glossitis ● Lipoma ● Sublingual abcess ● Lymphangioma INHERITED,CONGENITAL,DEVELOPMENT ● Schwannoma AND ACQUIRED ABNORMALITIES OF TONGUE MALIGNANT TUMOURS OF TONGUE ● White sponge nevus ● Squamous cell carcinoma ● Foliate papillitis ● Veruccous carcinoma ● Angina bullosa hemorrhagica ● Non-Hodgkin’s lymphoma ● Geographic tongue TRAUMATIC/REACTIONARY LESIONS OF ● Fissured tongue THE TONGUE ● Median rhomboid glossitis ● Fibrous reactive hyperplasia ● Bifurcated/tetrafurcated tongue ● Traumatic ulcer Indian Journal of Forensic Medicine & Toxicology, July-September 2021, Vol. -

Tobacco Use: a Smart Guide
1 Tobacco Use: A Smart Guide “STOPPING TAKES HARD WORK AND A LOT OF EFFORT, BUT – YOU CAN STOP TOBACCO” THE PROCESS OF QUITTING Do you find quitting tobacco difficult? The reason you continue to use tobacco is not because you are weak-willed or irresponsible, but because you are addicted. Nicotine is said to be more addictive than brown sugar (heroin) or cocaine. That is why people find it so difficult to stop, once they are habituated. The quitting process involves three steps: A. Preparation before quitting B. Actual quitting and C. Life after quitting. This manual will guide you through each of these steps. YOU NEED TO KNOW Before trying to quit tobacco you need to know a few facts about tobacco: • Tobacco comes in different forms….and all contain nicotine, the addictive substance. • Smoking forms of tobacco are beedis, cigarettes, cigars, chuttas, dhumti, pipe, hooklis, and hookah. • Smokeless forms of tobacco include chewing paan (betel quid) with zarda (tobacco), guthka, pan masala, manipuri tobacco, mawa, khaini, kaddi pudi, chewing tobacco leaves, mishri, gul, snuff, tobacco tooth paste and as tobacco water. Tobacco Facts • Tobacco is the leading cause of preventable death. • Each year tobacco kills 40,00,000 people. 2500 Indians die EVERYDAY due to tobacco related diseases. Deaths from tobacco use world wide are more than that from cocaine, heroin, alcohol, fires, accidents, murder, suicide, and AIDS COMBINED. • If you use tobacco, you are likely to die 15 years earlier. Tobacco Use: A Smart Guide 2 • Tobacco affects all the organs in the body from head to toe. -

Tobacco Induced Oral Keratosis. Oral Sub-Mucous Fibrosis. Nicotine Stomatitis
Tobacco induced oral keratosis. Oral sub-mucous fibrosis. Nicotine stomatitis. Actinic keratosis. Actinic cheilitis Assoc. prof. Zornitsa Mihaylova, DDS, PhD Dept. of Dental, oral and maxillofacial surgery, Faculty of Dental medicine, Medical Universtity- Sofia Precancerous lesions are morphologically altered tissues that possess greater than normal tissues risk of malignant transformation. The term “potentially malignant disorders” (PMD) is broadly accepted in order to avoid terminological confusion. In significant number of cases the oral cancer is preceded by a premalignancy. On the other hand PMD may not undergo malignant transformation (especially when the bad habits are ceased and proper treatment with long-term follow up have been conducted). The following risk factors may play a significant role in the development of PMD and cancer: tobacco smoking, smokeless tobacco, betel quid, alcohol consumption (the combination of smoking and alcohol significantly increases the risk of malignant transformation), oral HPV infection, radiation, vitamin deficiency, bacterial infections, immunosuppression and immunodeficiency, drugs, poor oral hygiene, chronic trauma. It is well established that the effects of the etiologic factors may vary depending on the geographic region, the lifestyle and the habits of the population. Tobacco induced oral keratosis There are three types of smokeless tobacco: dry snuff, moist snuff and chewing tobacco. Smokeless tobacco is mainly used by young males. The long-term/chronic smokeless tobacco use causes local alterations of the oral structures due to the significant nicotine absorption. Some of the most common oral changes related to smokeless tobacco are oral mucosa lesions, periodontal disease and dental caries. Clinically asymptomatic white lesions of the oral mucosa are identified. -
Opioid Prescriber Reference Guide
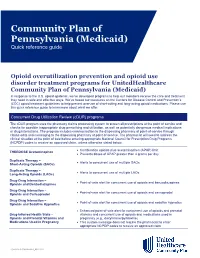
Community Plan of Pennsylvania (Medicaid) Quick reference guide Opioid overutilization prevention and opioid use disorder treatment programs for UnitedHealthcare Community Plan of Pennsylvania (Medicaid) In response to the U.S. opioid epidemic, we’ve developed programs to help our members receive the care and treatment they need in safe and effective ways. We’ve based our measures on the Centers for Disease Control and Prevention’s (CDC) opioid treatment guidelines to help prevent overuse of short-acting and long-acting opioid medications. Please use this quick reference guide to learn more about what we offer. Concurrent Drug Utilization Review (cDUR) programs The cDUR program uses the pharmacy claims processing system to screen all prescriptions at the point of service and checks for possible inappropriate drug prescribing and utilization, as well as potentially dangerous medical implications or drug interactions. The program includes communication to the dispensing pharmacy at point-of-service through claims edits and messaging to the dispensing pharmacy at point of service. The pharmacist will need to address the clinical situation at the point of sale before entering appropriate National Council for Prescription Drug Programs (NCPDP) codes to receive an approved claim, unless otherwise stated below. • Combination opioids plus acetaminophen (APAP) limit THERDOSE Acetaminophen • Prevents doses of APAP greater than 4 grams per day Duplicate Therapy – • Alerts to concurrent use of multiple SAOs Short-Acting Opioids (SAOs) Duplicate Therapy -

Paraneoplastic Pemphigus with Clinical Features of Lichen Planus Associated with Low-Grade B Cell Lymphoma
Report Paraneoplastic pemphigus with clinical features of lichen planus associated with low-grade B cell lymphoma Sónia Coelho, MD, José Pedro Reis, MD, Oscar Tellechea, MD, PhD, Américo Figueiredo, MD, PhD, and Martin Black, MD, PhD From the Department of Dermatology, Abstract University Hospital, Coimbra, Portugal, St Background Neoplasia-induced lichen planus is described as a cell-mediated reaction to John’s Institute of Dermatology, St Thomas’ unknown epithelial antigens. Paraneoplastic pemphigus (PNP), characterized by the presence Hospital, London, UK of a specific array of autoantibodies, probably represents a different form of presentation of the Correspondence same autoimmune syndrome where the mucocutaneous expression depends on the dominant Sónia Coelho pathologic mechanism. Clínica de Dermatologia, Hospital da Methods The authors report a case of PNP with predominant lichen planus-like lesions and Universidade review the relevant literature. We observed a 74-year-old female with vesico-bullous, erosive, P.3000–075 Coimbra target-shaped and flat papular lichenoid lesions on the lower legs, palms and soles, evolving for Portugal E-mail: [email protected] 3 weeks. Histopathology revealed a lichenoid dermatitis. Direct immunofluorescence showed C3 deposition around keratinocytes and epidermal IgG intranuclear deposition. Indirect immunofluorescence revealed circulating IgG with intercellular staining on rat bladder substrate. Immunoblotting demonstrated bands of 130, 190, 210 and 250 kDa antigens. A pararenal B cell lymphoma was found. Results Oral corticotherapy with 40 mg prednisolone daily was initiated with a good cutaneous response. Four months later, cyclophosphamide (50 mg/day) was introduced because of a discrete enlargement of the pararenal mass. The patient died on the seventh month of follow up as a result of respiratory insufficiency. -

Cardiovascular Drugs-Induced Oral Toxicities: a Murky Area to Be Revisited and Illuminated
Pharmacological Research 102 (2015) 81–89 Contents lists available at ScienceDirect Pharmacological Research j ournal homepage: www.elsevier.com/locate/yphrs Review Cardiovascular drugs-induced oral toxicities: A murky area to be revisited and illuminated a, b b Pitchai Balakumar ∗, Muthu Kavitha , Suresh Nanditha a Pharmacology Unit, Faculty of Pharmacy, AIMST University, Semeling, 08100 Bedong, Malaysia b Faculty of Dentistry, AIMST University, 08100 Bedong, Malaysia a r t i c l e i n f o a b s t r a c t Article history: Oral health is an imperative part of overall human health. Oral disorders are often unreported, but are Received 20 July 2015 highly troublesome to human health in a long-standing situation. A strong association exists between Received in revised form 22 August 2015 cardiovascular drugs and oral adverse effects. Indeed, several cardiovascular drugs employed clinically Accepted 8 September 2015 have been reported to cause oral adverse effects such as xerostomia, oral lichen planus, angioedema, Available online 25 September 2015 aphthae, dysgeusia, gingival enlargement, scalded mouth syndrome, cheilitis, glossitis and so forth. Oral complications might in turn worsen the cardiovascular disease condition as some reports suggest an Keywords: adverse correlation between periodontal oral disease pathogenesis and cardiovascular disease. These are Cardiovascular drugs certainly important to be understood for a better use of cardiovascular medicines and control of associated Oral adverse effects oral adverse effects. This review sheds lights on the oral adverse effects pertaining to the clinical use of Dry mouth Angioedema cardiovascular drugs. Above and beyond, an adverse correlation between oral disease and cardiovascular Dysgeusia disease has been discussed.