Professor Balasubramaniam Ramamurthi
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Padma Bhushan Prof. Jacob Chandy the Founder President of Neurological Society of India
Padma Bhushan Prof. Jacob Chandy The Founder President of Neurological Society of India M. SAMBASIVAN "Some are born great, some attain greatness by their effort and for some greatness is thrust upon them". Prof. Jacob Chandy (J.C) belongs to the second category. I deem it a privilege to pen the biography of my teacher, philosopher, guide and friend. Forgetting Prof. Jacob Chandy, would mean forgetting the development of Neurosciences in India and particularly the very beginnings of N.S.I. Tall, dark, rough looking and rough voiced giving a different impression at first sight, Prof. Jacob Chandy is a per fect person with a loving heart. As an artistic surgeon he was a Leonardo Da vinci, as an administrator he was a Bismarck, an avid planner and organiser as Winston Churchill, an erudite teacher as Nagarjuna, as devout as John the Baptist and a visionary as Asoka. Rare combinations indeed!. Now let me look into the details of the history in the life of Prof. Jacob Chandy. J. C. was born in an orthodox Christian family, father a presbyter of Anglican church and mother a house wife. In 1910, they were living' in the rural areas near Kottayam. These places in those days medical care was well neigh impossible. At 7th year of J. C's age his mother suddenly took ill and died, obviously without getting any medical help. This event made a sharp dent in the mind of young J. C. which gave him the im- petus to take to medicine, with the sole purpose of improving health care system in the villages. -

Summaries of Phds Awarded by University of Kerala (2015)
Summaries of PhDs awarded by University of Kerala (2015) Internal Quality Assurance Cell (IQAC) University of Kerala 2016 Compilation: Ms. Bindu Kumary S. DEO, University of Kerala This is one of the reports compiled by IQAC to enable study and analysis of research activities of the University. This is meant for private circulation only. © University of Kerala 2016 1 Summaries of PhDs awarded by University of Kerala (2015) Internal Quality Assurance Cell (IQAC) University of Kerala 2016 2 Summaries of PhDs Awarded in 2015 Contents Stream: Science & Technology 1 Biochemistry 5 - 14 2 Botany 15 - 24 3 Chemistry 25 - 46 4 Dentistry 47 - 49 5 Aquatic Biology and Fisheries 50 - 54 6 Demography 55 - 56 7 Environmental Sciences 57 - 59 8 Geology 60 - 64 9 Mathematics 65 - 68 10 Medicine 69 - 71 11 Nursing 72 - 74 12 Physical Education 75 - 78 13 Physics 79 - 86 14 Psychology 87 - 92 15 Statistics 93 - 94 16 Zoology 95 - 105 17 Geography 106 - 108 18 Futures Studies 109 - 110 19 Biotechnology 111 - 128 20 Organic Chemistry 129 - 130 21 Engineering 131 - 140 Stream: Social Science 1 Commerce 141 - 145 2 Economics 146 - 149 3 Education 150 - 158 4 History 159 - 165 5 Home Science 166 - 168 6 Law 169 - 171 7 Learning Disability 172 - 173 8 Library & Information Science 174 - 177 9 Management Studies 178 - 183 10 Philosophy 184 - 186 11 Physical Education 187 - 190 12 Political Science 191 - 194 13 Social Work 195 - 197 14 Sociology 198 - 201 Stream: Arts and Humanities 1 Arabic 202 - 203 2 English 204 - 210 3 German 211 - 212 4 Malayalam 213 - 220 5 Music 221 - 226 6 Sanskrit 227 - 232 7 Tamil 233 - 235 8 Hindi 236 - 247 9 Linguistics 248 - 249 3 Preface University of Kerala accepted 343 PhD dissertations in 2015. -

Jacob Chandy: Pioneering Neurosurgeon of India
LEGACY—INSTITUTIONS AND PEOPLE Jacob Chandy: Pioneering Neurosurgeon of India Jacob Abraham, MS JACOB CHANDY, WHO passed away in 2007 at the age of 97, was born into a deeply reli- Department of Neurological Sciences, gious Christian family in Kerala, South India. After obtaining his medical education at Christian Medical College, the Madras Medical College, Madras, he serendipitously came to work with Dr Paul Vellore, India Harrison, a renowned medical missionary, in the Gulf state of Bahrain. Harrison urged K. V. Mathai, MS Chandy to pursue training in the fledgling specialty of neurosurgery in North America. Department of Neurological Sciences, Chandy received his neurosurgical training at the Montreal Neurological Institute with Christian Medical College, Wilder Penfield and in Chicago with Theodore Rasmussen. At Harrison’s urging, Chandy Vellore, India decided to return to India after completing his training to work at the Christian Medical College in Vellore,. Thus, it was in 1949 that Chandy established the first neurosurgery depart- Vedantam Rajshekhar, MCh ment in south Asia in Vellore. He initiated the first neurosurgical training program in Department of Neurological Sciences, India at the Christian Medical College in 1957, with a distinct North American neurosur- Christian Medical College, Vellore, India gical tradition. He went on to train nearly 20 neurosurgeons, many of whom set up new departments of neurosurgery in their home states. Chandy also had several other remark- Raj K. Narayan, MD able achievements to his credit. Despite the pressures of clinical practice, he insisted on Department of Neurosurgery, fostering both basic and clinical neurosciences within his department, an arrangement Harvey Cushing Institutes of that persists to this day in the Department of Neurological Sciences at the Christian Neuroscience, North Shore University Hospital, Medical College, Vellore. -

CMC-2012-2013-Facts
Contents CMC Statistics 2 Diagnostic Tests and Therapeutic Procedures 3 Outpatient Statistics in the Main Hospital 4 Geographical Distribution of Inpatients 6 Outreach 7 General Services 8 Medical Education 9 Fellowship Courses 10 College of Nursing 11 Allied Health Sciences 12 Members of the CMC Council - India 13 Overseas Member Churches and Organizations 13 Administrators 14 Heads of Units and Departments 15 Events 2012-2013 17 Awards and Honours 22 Invitation to Share 24 Contact Information 25 Acknowledgements 25 CMC Statistics Diagnostic Tests and Therapeutic Procedures Beds Inpatients Outpatients Births Outreach Diagnostic Tests Therapeutic Procedures Main Hospital 2,082 1,02,738 16,72,207 13,316 - Allergy Skin Testing 2,525 Anaesthetic Procedures (in OR) 31,367 Community Health and Development 130 12,077 90,848 3,307 76,919 Audiometries 15,305 Anaesthetic Procedures (outside OR) 9,827 Rural Unit for Health and Social Affairs 69 3,758 1,07,654 1,063 36,831 Biopsies 44,949 Antenatal Diagnosis by DNA Testing 129 Schell Eye Hospital 100 7,040 1,07,301 - 21,140 Bronchoscopy and Medical Thoracoscopy 2,156 Blood Transfusions 61,513 Low Cost Effective Care Unit 46 1,913 58,888 197 872 Cardiac Angiograms & Electrophysiology 3,087 Bone Marrow Transplants 193 Mental Health Centre 98 878 1,01,623 - - Cardiac Tests 535 Brachytherapy Procedures 336 Nambikkai Nilayam 24 104 4,102 - 187 Clinical Biochemistry Tests 39,53,163 CPAP 217 Rehabilitation Institute 83 519 - - 50 Clinical Pathology & Blood Bank Tests 58,36,664 Cardiac Interventions 2,215 -
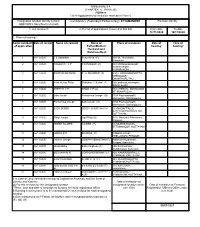
Christian Medical College Vellore This Prospectus Is Common to All Courses Around the Year and Needs to Be Read with the Appropriate Admission Bulletin for the Course
Admissions 2018-2019 Christian Medical College Vellore This prospectus is common to all courses around the year and needs to be read with the appropriate admission bulletin for the course ALL COURSES AND ADMISSIONS TO OUR COLLEGE ARE SUBJECT TO APPLICABLE REGULATIONS BY UNIVERSITY/GOVERNMENT/MEDICAL COUNCIL OF INDIA/NATIONAL BOARD OF EXAMS NO FEE OR DONATION OR ANY OTHER PAYMENTS ARE ACCEPTED IN LIEU OF ADMISSIONS, OTHER THAN WHAT HAS BEEN PRESCRIBED IN THE PROSPECTUS THE GENERAL PUBLIC ARE THEREFORE CAUTIONED NOT TO BE LURED BY ANY PERSON/ PERSONS OFFERING ADMISSION TO ANY OF THE COURSES CONDUCTED BY US SHOULD ANY PROSPECTIVE CANDIDATE BE APPROACHED BY ANY PERSON/PERSONS, THIS MAY IMMEDIATELY BE REPORTED TO THE LAW ENFORCEMENT AGENCIES FOR SUITABLE ACTION AND ALSO BROUGHT TO THE NOTICE OF OUR COLLEGE AT THE ADDRESS GIVEN BELOW OUR COLLEGE WILL NOT BE RESPONSIBLE FOR ANY CANDIDATES OR PARENTS DEALING WITH SUCH PERSONS CORRESPONDENCE All correspondence should refer to the Application number or to the Hall Ticket number and be addressed to: The Registrar Christian Medical College, Vellore-632002 Tamil Nadu, India Phone: (0416)2284255 Fax: (0416) 2262788 Email: [email protected] Website: http://admissions.cmcvellore.ac.in PLEASE NOTE: WE DO NOT ADMIT STUDENTS THROUGH AGENTS OR AGENCIES Important Information: “The admission process contained in this Bulletin shall be subject to any order that maybe passed by the Hon’ble Supreme Court or the High Court in the proceedings relating to the challenge to the NEET, common counselling or -

Supplement Book 2013
CMC Statistics Diagnostic Tests and Therapeutic Procedures Beds Inpatients Outpatients Births Diagnostic Tests Therapeutic Procedures Main Hospital 2,122 1,06,423 17,44,529 13,867 Allergy Skin Testing 2,250 Anaesthetic Procedures (in OR) 31,628 Community Health and Development 135 10,601 83,356 3,191 Antenatal Diagnosis by DNA Testing 105 Anaesthetic Procedures (outside OR) 10,221 Rural Unit for Health and Social Affairs 70 3,535 94,913 894 Audiometries 27,630 Blood Transfusions 66,195 Schell Eye Hospital 100 7,063 1,05,937 - Biopsies 47,064 Bone Marrow Transplants 205 Bronchoscopy and Medical Thoracoscopy 2,238 Low Cost Effective Care Unit 46 1,753 67,290 220 Brachytherapy Procedures 210 Cardiac Diagnostic Angiograms 3,317 Mental Health Centre 98 980 1,09,530 - CPAP 733 Clinical Biochemistry Tests 25,31,869 Cardiac Interventions 2,177 Nambikkai Nilayam 24 112 4,505 - Clinical Path. and Blood Bank Tests 59,93,960 Conventional Radiotherapy 1,453 Rehabilitation Institute 83 557 - - Clinical Pharmacology Tests 22,535 3D Conformal Radiotherapy 386 Total 2,678 1,31,024 22,10,060 18,172 Cytology and FNAC 20,001 Dental Procedures 62,042 Cystoscopies 2,666 Developmental Paediatric Assessment / Daily in CMC Personnel CT Scans 31,259 Assistance 4,361 Outpatients* 7,175 Outpatients** 5,628 Administrative Staff and Clerks 899 ECG 1,05,917 Developmental Paediatric Therapy and Inpatients* 2,015 Inpatients** 1,651 Chaplains 16 ECHO 41,227 Surveillance 2,415 Operations* 158 Bed Occupancy** 78.1% Doctors 1,413 EEG 7,699 Dermatology Procedures 18, 879 Births* 50 Av. -
(CHAPTER V , PARA 25) FORM 9 List of Applications for Inclusion
ANNEXURE 5.8 (CHAPTER V , PARA 25) FORM 9 List of Applications for inclusion received in Form 6 Designated location identity (where Constituency (Assembly/£Parliamentary): ETTUMANOOR Revision identity applications have been received) 1. List number@ 2. Period of applications (covered in this list) From date To date 16/11/2020 16/11/2020 3. Place of hearing * Serial number$ Date of receipt Name of claimant Name of Place of residence Date of Time of of application Father/Mother/ hearing* hearing* Husband and (Relationship)# 1 16/11/2020 T S Sasankan Sukumaran (F) 10/314, Thoranathu, Aymanam, , 2 16/11/2020 PRASANTH V P P D PRASAD (F) 189 VENGALIKKALAM, KUMARAKOM , KUMARAKOM, , 3 16/11/2020 SWATHY KRISHNA P G PRADEEP (F) 4/314 PADINJAREKUTTU, NEENDOOR, ONAMTHURUTHU, , 4 16/11/2020 Kiran Kurian Philip Shibymon C Kurian (F) 550, padinjattumbhagam, Athirampuzha, , 5 16/11/2020 KEERTHI C P KIRAN C P (O) 553 CHERIVIL, MANNANAM, ATHIRAMPUZHA, , 6 16/11/2020 Babu Jacob Ponnamma Joseph (O) 510A Pazhayampallil, Mannanam, Athirampuzha, , 7 16/11/2020 Ponnamma Joseph Babu Jacob (H) 510A Pazhayampallil, Mannanam, Athirampuzha, , 8 16/11/2020 SUBY BOBBY BOBBY CHERIYAN (H) 233/MADAPPALLIL, SREEKANDAMANGALAM, KOTTAYAM, , 9 16/11/2020 Philip Joseph Sigi Philip (O) B412 Maniyalil, Ettumanoor, Kottayam, , 10 16/11/2020 AMEER NAJEEB NAJEEB (F) 13,NAJEEB MANZIL, ETTUMANOOR, KOTTAYAM, , 11 16/11/2020 GOKUL K R SIVADAS (F) 1 REMALAYAM, THELLAKOM, PEROOR, , 12 16/11/2020 Naveen Joseph JOSEPH SEBASTIAN (F) Pathinanchil parambil, Karippa, Arpookara, , 13 16/11/2020 -

Kerala Chapter
Kerala Chapter Sr. No. Membership_No member_name 1 F02473 Appu Prabhakaran 2 A04793 Sasidharan M. Nair 3 A05200 Ramaswamy Ayyappan 4 A05218 Aniparambil R. Menon 5 A05235 S Soman 6 A05257 John Jocob 7 A05307 K. A. Kurien 8 A05332 A. Rajasekharan 9 A05401 Kocherry J. John 10 A05527 Paily George Thekkummottil 11 A05533 John A. 12 A05614 T. V. Kaladharan 13 A05617 Maliakal Chandy Mathew 14 F05703 Bhaskaran Rajam Ajit 15 F05758 Cherthedoth Muraleedharan 16 A05796 S. V. Abdunnazir 17 A05870 Baby Paul Karikuzhiyil 18 A05905 Sunny Joseph 19 A05927 Santhosh Paul Manvettom 20 A05976 Mony D. S Darley 21 A05985 Gopala Mohanan 22 A05992 Samuel Eapen 23 A06140 Atchuthan R. Nair 24 A06244 Jayanand Mukund Kilikar 25 A06247 K. P. Nileena 26 A06596 Chandy Jacob Francis 27 A06994 K S Vasanth Kumar 28 A07030 Balakrishnan Panampulli 29 A07061 K. J. Martin Thomas 30 A07074 Beena Ravindran 31 A07097 Mariamma Jacob Philip 32 A07099 Jabeen Lalichan Zacharias 33 F07103 Mathew Joseph 34 A07109 Mathew Mathai 35 A07117 M. M. Philip 36 F07126 Saira Abraham 37 A07136 Payikad G Varughese 38 A07207 Isaac K Shery 39 A07338 Tom J Nedumthacady 40 A07415 Gabriel Constant Kochiraman 41 A07486 Joseph George 42 A07487 J. Jayasankar 43 A07515 M. A. Sebastian 44 A07873 Sunil John George 45 A08023 Ranjini T. Bhattathiripad 46 F08221 Anand D K 47 A08223 A. V. Abraham 48 A08224 A. Vijayachandran 49 A08338 Thomas Jose Karimpanal 50 F08475 Meera Ashok 51 A08806 K. C. George 52 A08823 Sajan Ipe Pulimood 53 A08832 Rama Anandavallyamma Sreedhar Sr. No. Membership_No member_name 54 A08834 Suresh Kumar Sreedharannair 55 A08910 Jacob M Thomas 56 A08985 Paul Isaac 57 A08994 John Joseph 58 A08995 Rajesh Joseph 59 A09025 George Nedumchalil Mathai 60 A09034 Sali M. -

Prof. B. Ramamurthi 1922-2003
Prof. B. Ramamurthi 1922-2003 Prof. B. Ramamurthi was born on January, 30th 1922 at the unique distinction of establishing the heading one more Sirkali, a small town in Tamilnadu where his father Capt. T S centre of excellence in the city of Madras, the Dr. A. Balasubramaniam was an Assistant Surgeon in the Govern- Lakshmipathi Neurosurgical Centre, at the Voluntary Health ment Hospital. He was a brilliant student at the E R High Services Hospital. School and St Joseph’s College, Trichy, before he joined the In recognition of his services he received numerous awards Madras Medical College. He was awarded the Johnstone Gold including the Padma Bhushan from the Government of India, medal as the Best Outgoing Student when he passed out of and the Dhanvantri Award. The Armed Forces of India con- the Madras Medical College in 1943. He secured his Master ferred on him the title of Hony. Brigadier in the Army, for of Surgery (M.S.) degree and his Fellowship to the Royal Col- Services rendered to the armed forces. In 1989, he was made lege of Edinburgh (FRCS) in 1947. the Hony. President of the World Congress of Neurological He was selected by the Madras Government for training in Surgery. He was the senior most practicing Neurosurgeon of Neurosurgery and reached Newcastle, UK, on 2nd January the world and was till his demise the Professor and Head of 1949. He trained in the UK and then in Europe and Canada. Dr. A. Lakshmipathi Neurosurgical Centre and Post-gradu- On completing his training Dr. Ramamurthi returned to Ma- ate Institute of Neurological Surgery, VHS and Malar Hospi- dras, bringing back with him the traditions of the British, tals, Chennai. -

Professor Jacob Chandy (1910-2007)
Obituary Professor Jacob Chandy (1910-2007) K. V. Mathai Retired Professor of Neurosurgery and Head of the Department of Neurological Sciences, Christian Medical College, Vellore, India. Padmabhushan Professor Dr. Jacob Chandy, born on the ’50s, in many other centers in India, Neurology and January 23, 1910, is no more with us physically from Neurosurgery were put under General Medicine and June 23, 2007. However, he shall remain in our hearts General Surgery which hindered the effective growth forever. There are individuals and institutions among us of these specialties to some extent. The lesson learned but there are a few individuals who are not only eminent was “Be independent but be fully cooperative”. individuals but are also synonymous with institutions. The development of Neurological Sciences as an Dr. Jacob Chandy was one such individual. In the 1950s integrated department was an idea that Dr. Jacob and ’60s the mention of neurological sciences or medical Chandy inherited from the Montreal Neurological education brought the image of Dr. Jacob Chandy to Institute (MNI), Canada. This was not a popular idea in one’s mind. India at that time. It was Dr. Chandy’s personality and He started the first department of Neurological foresight that made the system function in a smooth Sciences in India in 1949 at the Christian Medical manner. The individual disciplines had the full freedom College, Vellore. He was the founder President of the of functioning under unit heads. The head of the Neurological Society of India. He was a founder member department of Neurological Sciences, a rotating job every of the National Academy of Medical Sciences and the five years, coordinated the work and the development Indian Association for the Advancement of Medical process. -

Prof. B. Ramamurthi (1922-2003), the Pioneer Neurosurgeon Dr
Chettinad Health City Medical Journal Volume 3, Number 2 From the Pages of History Prof. B. Ramamurthi (1922-2003), The Pioneer Neurosurgeon Dr. V.G.Ramesh, Professor and HOD, Dept. of Neuro Surgery, Chettinad Hospital and Research Institute, Chennai, India Chettinad Health City Medical Journal 2014; 3(2): 91 Professor B. Ramamurthi (popularly known as BRM), was the pioneer Neurosurgeon, recognized as the Father of Indian Neurosurgery. He was born on 31st January, 1922 at Sirkali in Tamil Nadu. He completed his MBBS in 1943, MS (General Surgery) in 1947 from Madras Medical College and FRCS (Ed) thereafter. He was sent for training in Neurosurgery by the Government of Madras to Newcastle (UK) in 1949 at a time when Neurosurgery was not known in India. He was trained under Prof. G. F. Rowbotham at Newcastle. He also spent time with doyens of Neurosurgery like Prof. Geoffrey Jefferson (Manchester), Prof. Krayenbuhl (Zurich), Dr. Edward Busch (Copenhagen), Prof. Olivecrona (Stockholm) and Prof. Wilder Penfield (Montreal). He returned to Madras in 1950, bringing back with him the traditions of the British, American, Canadian and European schools of Neurosurgery and started Neurosurgery in Madras General Hospital and Madras Medical Prof. B. Ramamurthi College on October 24th (Vijayadasami day). This was the second Neurosurgery department to be started in India(Prof. Jacob Chandy had started his department at Christian Medical College, Vellore a year earlier). Against great odds and difficulties, Dr B. Ramamurthi built and developed the neurosurgical department, which later developed into the Institute of Neurology at the Government General Hospital, where he was the Professor and Head till his retirement in 1978. -

Alphabetic List of All Candidates Who Applied for Recruitment for the Post of Programmer Registration No
Alphabetic List of All Candidates who Applied for Recruitment for the Post of Programmer Registration No. Name of Candidate Fathers/ Husband Name of Candidate 813409 Aanchal Malhotra Balbir Mahlotra 813527 Aarti Joshi R C Joshi 813330 Abhay Shankar Pandey Late Ravi Shankar Pandey 813088 Abhey Sood Rajender Sood 813333 Abhilash Vijayan P P Vijayan 813360 Abhimanyu Arjun Lal Sharma 813290 Abhinav Anand Abdhesh Prasad Verma 813428 Abhinav Singh Mahendra Singh Rawat 813273 Abhishek Ramesh Chandra Mishra 813279 Abhishek Dubey Braj Mohan Dubey 813082 Abhishek Kumar Dabas Shri Satish Chander Dabas 813367 Abhishek Kumar Dubey Rajesh Dubey 813342 Abhishek Sharma Rajkumar Sharma 813397 Abhishek Thapliyal L N Thapliyal 813569 Adil Mudasir Malla Gulam Hassan Malla 813395 Aditya Chettri Ganesh Cheetri 813509 Aditya Maheshwari Lalchand Chandak 813207 Ajaya Singh Bhure Singh 813616 Ajeet Khem Chand 813217 Ajit Kumar Dhaneshwar Kamat 813199 Ajith Kumar K Kumaran E 813306 Akanksha Sharma Dr O P Sharma 813149 Akansha Srivastava Anil Kumar Srivastava 813633 Akash Deep Deep Chandra 813459 Akash Singh Prabhat Kumar Singh 813620 Akhil Kumar Hans Kumar 813152 Akhilesh Mishra Ram Kishun Mishra 813498 Akshay Dawar Man Mohan Dawar 813036 Alka Dharm Prakash Gangal 813210 Alok Kumar Shri Suresh Chand 813144 Alok Kumar Mishra Birendra Kumar Mishra 813053 Alok Singh Negi Alam Singh Negi 813129 Aman Gupta Ishwar Gupta 813473 Amardeep Singh Mahavir Singh 813525 Ambar Dixit Brajesh Kumar Dixit 813244 Ameer Ulla Siddiqui Ameen Uddin Siddiqui 813180 Amit Dahiya Sukhbir Singh Dahiya 813338 Amit Diwan Ashok Diwan 813002 Amit Gupta Jai Prakash Gupta 813014 Amit Kumar Yogendra Roy 813185 Amit Kumar Sri Chandra Datta Sharma 813331 Amit Kumar K E Prasad 813033 Amit Kumar Pathak Ram Prakash Pathak 813256 Amit Kumar Tyagi Satish Kumar Tyagi 813436 Amit Kumar Tyagi Dharam Vir Tyagi 1 Alphabetic List of All Candidates who Applied for Recruitment for the Post of Programmer Registration No.