Protocol Alert
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Single Dose of the CXCR4 Antagonist BL-8040 Induces Rapid
Published OnlineFirst August 23, 2017; DOI: 10.1158/1078-0432.CCR-16-2919 Cancer Therapy: Clinical Clinical Cancer Research Single Dose of the CXCR4 Antagonist BL-8040 Induces Rapid Mobilization for the Collection of Human CD34þ Cells in Healthy Volunteers Michal Abraham1, Yaron Pereg2, Baruch Bulvik1, Shiri Klein3, Inbal Mishalian3, Hana Wald1, Orly Eizenberg1, Katia Beider4, Arnon Nagler4, Rottem Golan2, Abi Vainstein2, Arnon Aharon2, Eithan Galun3, Yoseph Caraco5, Reuven Or6, and Amnon Peled3,4 Abstract Purpose: The potential of the high-affinity CXCR4 antagonist systemic reactions were mitigated by methylprednisolone, BL-8040 as a monotherapy-mobilizing agent and its derived paracetamol, and promethazine pretreatment. In the first part graft composition and quality were evaluated in a phase I clinical of the study, BL-8040 triggered rapid and substantial mobili- þ study in healthy volunteers (NCT02073019). zation of WBCs and CD34 cells in all tested doses. Four hours Experimental Design: The first part of the study was a ran- postdose, the count rose to a mean of 8, 37, 31, and 35 cells/mL domized, double-blind, placebo-controlled dose escalation (placebo, 0.5, 0.75, and 1 mg/kg, respectively). FACS analysis phase. The second part of the study was an open-label phase, in revealed substantial mobilization of immature dendritic, T, B, þ which 8 subjects received a single injection of BL-8040 (1 mg/kg) and NK cells. In the second part, the mean CD34 cells/kg and approximately 4 hours later underwent a standard leukapher- collected were 11.6 Â 106 cells/kg. The graft composition was esis procedure. -

European Iron Club 7
EUROPEAN IRON CLUB 7 - 10 MEETING IN April INNSBRUCK 2016 Programme Kein Eisen unter der Oberfläche Novartis Pharma GmbH Stella-Klein-Loew-Weg 17 | 1020 Wien www.novartispharma.at | +43 1 866 57-0 Erstellungsdatum 02/2016 | AT1602436490 CONTENTS Welcome 6 Committees 7 Masterclass in Iron Therapies 8 Thursday, 7 April 2016 European Iron Club Annual Meeting 10 Friday, 8 April 2016 European Iron Club Annual Meeting 20 Saturday, 9 April 2016 Scientific Programme 31 Kein Eisen Sunday, 10 April 2016 Innsbruck city map 34 unter der General Information 35 Exhibitors & Sponsors 40 Oberfläche Drug labels 41 Notes 42 Novartis Pharma GmbH 3 Stella-Klein-Loew-Weg 17 | 1020 Wien www.novartispharma.at | +43 1 866 57-0 Erstellungsdatum 02/2016 | AT1602436490 CONGRESS INFORMATION DATES CONGRESS ORGANISER Masterclass in Iron Therapies PCO TYROL CONGRESS Thursday, 7 April, 2016 MMag. Ina Kähler Mechthild Walter European Iron Club Annual Rennweg 3 Meeting 6020 Innsbruck Friday, 8 April – Saturday, 9 April, Austria 2016 T: +43 (0) 512 575600 F: +43 (0) 512 575607 Non HFE Hemochromatosis E: [email protected] Registry Meeting I: www.pco-tyrolcongress.at Sunday, 10 April, 2016 Meeting of Patient Organisations Sunday, 10 April, 2016 EXHIBITION MANAGEMENT AND SPONSORING VENUE (THU - SAT) S12! STUDIO12 GMBH CONGRESS INNSBRUCK Ralph Kerschbaumer Rennweg 3 Kaiser Josef Straße 9 6020 Innsbruck 6020 Innsbruck Austria Austria www.cmi.at T: +43 (0) 512 890438 F: +43 (0) 512 890438 15 E: [email protected] I: www.studio12.co.at VENUE (SUN) AUSTRIA TREND HOTEL Rennweg 12a -

How I Treat Myelofibrosis
From www.bloodjournal.org by guest on October 7, 2014. For personal use only. Prepublished online September 16, 2014; doi:10.1182/blood-2014-07-575373 How I treat myelofibrosis Francisco Cervantes Information about reproducing this article in parts or in its entirety may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests Information about ordering reprints may be found online at: http://www.bloodjournal.org/site/misc/rights.xhtml#reprints Information about subscriptions and ASH membership may be found online at: http://www.bloodjournal.org/site/subscriptions/index.xhtml Advance online articles have been peer reviewed and accepted for publication but have not yet appeared in the paper journal (edited, typeset versions may be posted when available prior to final publication). Advance online articles are citable and establish publication priority; they are indexed by PubMed from initial publication. Citations to Advance online articles must include digital object identifier (DOIs) and date of initial publication. Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036. Copyright 2011 by The American Society of Hematology; all rights reserved. From www.bloodjournal.org by guest on October 7, 2014. For personal use only. Blood First Edition Paper, prepublished online September 16, 2014; DOI 10.1182/blood-2014-07-575373 How I treat myelofibrosis By Francisco Cervantes, MD, PhD, Hematology Department, Hospital Clínic, IDIBAPS, University of Barcelona, Barcelona, Spain Correspondence: Francisco Cervantes, MD, Hematology Department, Hospital Clínic, Villarroel 170, 08036 Barcelona, Spain. Phone: +34 932275428. -

Tracks 1-9 David P Steensma, MD Select Excerpts from the Interview
INTERVIEW David P Steensma, MD Dr Steensma is Faculty Member in the Adult Leukemia Program at Dana-Farber Cancer Institute and Associate Professor of Medicine at Harvard Medical School in Boston, Massachusetts. Tracks 1-9 Track 1 Novel agents under investigation for Track 6 Case discussion: A 68-year-old man FLT3-ITD-mutated acute myeloid with postpolycythemia vera myelofi- leukemia (AML) brosis whose symptoms begin to recur Track 2 Activity and tolerability of the orally after 2 years of ruxolitinib therapy administered inhibitor of FLT3/AXL Track 7 Activity and toxicities of novel JAK gilteritinib (ASP2215) in AML inhibitors — pacritinib, momelotinib — Track 3 Recent developments in myelodys- in myeloproliferative disorders plastic syndromes (MDS) Track 8 Case discussion: A 65-year-old woman Track 4 Clinical experience with lenalidomide with hydroxyurea-resistant polycythemia for patients with MDS with and vera treated with ruxolitinib without del(5q) Track 9 Clinical experience with dosing and Track 5 Management of MDS in patients with continuation of ruxolitinib therapy disease progression on a hypomethyl- in patients experiencing treatment- ating agent associated cytopenias Select Excerpts from the Interview Tracks 1-2 DR LOVE: Would you discuss some of the most promising new agents and strate- gies under investigation for patients with acute myeloid leukemia (AML)? DR STEENSMA: One area of interest involves investigation of agents targeting FLT3 mutations, which are driver mutations commonly associated with AML. The 2 general classes of FLT3 mutations are internal tandem duplication (ITD) mutations and tyrosine kinase domain (TKD) mutations. Both constitutively activate the FLT3 receptor, but ITD mutations tend to be associated with more proliferative disease and a poorer prognosis, and they’re more common than TKD mutations. -

WO 2014/194127 Al 4 December 2014 (04.12.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/194127 Al 4 December 2014 (04.12.2014) P O P C T (51) International Patent Classification: Songyuan; c/o Plexxikon Inc., 9 1 Bolivar Drive, Berkeley, C07D 213/75 (2006.01) C07D 487/04 (2006.01) California 94710 (US). SPEVAK, Wayne; c/o Plexxikon C07D 417/04 (2006.01) A61K 31/519 (2006.01) Inc., 9 1 Bolivar Drive, Berkeley, California 94710 (US). C07D 471/04 (2006.01) HABETS, Gaston G.; c/o Plexxikon Inc., 9 1 Bolivar Drive, Berkeley, California 94710 (US). BURTON, Betsy; (21) International Application Number: c/o Plexxikon Inc., 9 1 Bolivar Drive, Berkeley, California PCT/US20 14/040076 94710 (US). (22) International Filing Date: (74) Agents: TANNER, Lorna L. et al; Sheppard Mullin 29 May 2014 (29.05.2014) Richter & Hampton LLP, 379 Lytton Avenue, Palo Alto, (25) Filing Language: English California 94301-1479 (US). (26) Publication Language: English (81) Designated States (unless otherwise indicated, for every kind of national protection available): AE, AG, AL, AM, (30) Priority Data: AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, 61/829,190 30 May 2013 (30.05.2013) US BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, (71) Applicant: PLEXXIKON INC. [US/US]; 1 Bolivar DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, Drive, Berkeley, California 94710 (US). HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, (72) Inventors: ZHANG, Chao; c/o Plexxikon Inc., 9 1 Bolivar MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, Drive, Berkeley, California 94710 (US). -

Modulators of CXCR4 and CXCR7/ACKR3 Function
Molecular Pharmacology Fast Forward. Published on September 23, 2019 as DOI: 10.1124/mol.119.117663 This article has not been copyedited and formatted. The final version may differ from this version. MOL # 117663 Modulators of CXCR4 and CXCR7/ACKR3 function Ilze Adlere*, Birgit Caspar*, Marta Arimont*, Sebastian Dekkers, Kirsten Visser, Jeffrey Stuijt, Chris de Graaf, Michael Stocks, Barrie Kellam, Stephen Briddon, Maikel Wijtmans, Iwan de Esch, Stephen Hill, Rob Leurs# * These authors contributed equally to this work. Downloaded from # Corresponding author molpharm.aspetjournals.org Griffin Discoveries BV, Amsterdam, The Netherlands (IA, IE, RL), Division of Physiology, Pharmacology and Neuroscience, School of Life Sciences, University of Nottingham, Nottingham, UK (BC, SJB, SJH), Centre of Membrane Proteins and Receptors (COMPARE), Universities of Birmingham and Nottingham, The Midlands, U.K. (BC, BK, SD, SB, SH), at ASPET Journals on September 26, 2021 School of Pharmacy, University of Nottingham, Nottingham, U.K. (SD, BK, MS), Division of Medicinal Chemistry, Amsterdam Institute for Molecules, Medicines and Systems, Faculty of Science, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands (MA, KS, JS, CG, MW, IE, RL), Sosei Heptares, Cambridge, U.K. (CG) 1 Molecular Pharmacology Fast Forward. Published on September 23, 2019 as DOI: 10.1124/mol.119.117663 This article has not been copyedited and formatted. The final version may differ from this version. MOL # 117663 Running title: Modulators of CXCR4 and CXCR7/ACKR3 function Corresponding -

Dynamic Chemotherapy-Induced Upregulation of CXCR4 Expression: a Mechanism of Therapeutic Resistance in Pediatric AML
Published OnlineFirst June 10, 2013; DOI: 10.1158/1541-7786.MCR-13-0114 Molecular Cancer Cell Death and Survival Research Dynamic Chemotherapy-Induced Upregulation of CXCR4 Expression: A Mechanism of Therapeutic Resistance in Pediatric AML Edward Allan R. Sison, Emily McIntyre, Daniel Magoon, and Patrick Brown Abstract Cure rates in pediatric acute leukemias remain suboptimal. Overexpression of the cell-surface chemokine receptor CXCR4 is associated with poor outcome in acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML). Certain nonchemotherapeutic agents have been shown to modulate CXCR4 expression and alter leukemia interactions with stromal cells in the bone marrow microenvironment. Because chemotherapy is the mainstay of AML treatment, it was hypothesized that standard cytotoxic chemotherapeutic agents induce dynamic changes in leukemia surface CXCR4 expression, and that chemotherapy-induced upregulation of CXCR4 repre- sents a mechanism of acquired therapeutic resistance. Here, it was shown that cell lines variably upregulate CXCR4 with chemotherapy treatment. Those that showed upregulation were differentially protected from chemotherapy- induced apoptosis when cocultured with stroma. The functional effects of chemotherapy-induced CXCR4 up- regulation in an AML cell line (MOLM-14, which harbors consistent upregulated CXCR4) and clinical specimens were explored. Importantly, enhanced stromal-cell derived factor-1a (SDF1A/CXCL12)-mediated chemotaxis and stromal protection from additional chemotherapy-induced apoptosis was found. Furthermore, treatment with plerixafor, a CXCR4 inhibitor, preferentially decreased stromal protection with higher chemotherapy-induced upregulation of surface CXCR4. Thus, increased chemokine receptor CXCR4 expression after treatment with conventional chemotherapy may represent a mechanism of therapeutic resistance in pediatric AML. Implications: CXCR4 may be a biomarker for the stratification and optimal treatment of patients using CXCR4 inhibitors. -

Overview of Current Targeted Anti-Cancer Drugs for Therapy in Onco-Hematology
medicina Review Overview of Current Targeted Anti-Cancer Drugs for Therapy in Onco-Hematology Stefania Crisci 1 , Filomena Amitrano 2, Mariangela Saggese 1, Tommaso Muto 3, Sabrina Sarno 4, Sara Mele 1, Pasquale Vitale 1, Giuseppina Ronga 1, Massimiliano Berretta 5 and Raffaele Di Francia 6,* 1 Hematology-Oncology and Stem Cell Transplantation Unit, Istituto Nazionale Tumori, Fondazione “G. Pascale” IRCCS, 80131 Naples, Italy 2 Gruppo Oncologico Ricercatori Italiano GORI ONLUS, 33100 Pordenone, Italy 3 Hematology and Cellular Immunology (Clinical Biochemistry) A.O. dei Colli Monaldi Hospital, 80131 Naples, Italy 4 Anatomia Patologica, Istituto Nazionale Tumori, Fondazione “G. Pascale” IRCCS, 80131 Naples, Italy 5 Department of Medical Oncology, CRO National Cancer Institute, 33081 Aviano (PN), Italy 6 Italian Association of Pharmacogenomics and Molecular Diagnostics (IAPharmagen), 60125 Ancona, Italy * Correspondence: [email protected] Received: 12 May 2019; Accepted: 24 July 2019; Published: 28 July 2019 Abstract: The upgraded knowledge of tumor biology and microenviroment provides information on differences in neoplastic and normal cells. Thus, the need to target these differences led to the development of novel molecules (targeted therapy) active against the neoplastic cells’ inner workings. There are several types of targeted agents, including Small Molecules Inhibitors (SMIs), monoclonal antibodies (mAbs), interfering RNA (iRNA) molecules and microRNA. In the clinical practice, these new medicines generate a multilayered step in pharmacokinetics (PK), which encompasses a broad individual PK variability, and unpredictable outcomes according to the pharmacogenetics (PG) profile of the patient (e.g., cytochrome P450 enzyme), and to patient characteristics such as adherence to treatment and environmental factors. This review focuses on the use of targeted agents in-human phase I/II/III clinical trials in cancer-hematology. -

Promising Therapeutic Targets for Treatment of Rheumatoid Arthritis
REVIEW published: 09 July 2021 doi: 10.3389/fimmu.2021.686155 Promising Therapeutic Targets for Treatment of Rheumatoid Arthritis † † Jie Huang 1 , Xuekun Fu 1 , Xinxin Chen 1, Zheng Li 1, Yuhong Huang 1 and Chao Liang 1,2* 1 Department of Biology, Southern University of Science and Technology, Shenzhen, China, 2 Institute of Integrated Bioinfomedicine and Translational Science (IBTS), School of Chinese Medicine, Hong Kong Baptist University, Hong Kong, China Rheumatoid arthritis (RA) is a systemic poly-articular chronic autoimmune joint disease that mainly damages the hands and feet, which affects 0.5% to 1.0% of the population worldwide. With the sustained development of disease-modifying antirheumatic drugs (DMARDs), significant success has been achieved for preventing and relieving disease activity in RA patients. Unfortunately, some patients still show limited response to DMARDs, which puts forward new requirements for special targets and novel therapies. Understanding the pathogenetic roles of the various molecules in RA could facilitate discovery of potential therapeutic targets and approaches. In this review, both Edited by: existing and emerging targets, including the proteins, small molecular metabolites, and Trine N. Jorgensen, epigenetic regulators related to RA, are discussed, with a focus on the mechanisms that Case Western Reserve University, result in inflammation and the development of new drugs for blocking the various United States modulators in RA. Reviewed by: Åsa Andersson, Keywords: rheumatoid arthritis, targets, proteins, small molecular metabolites, epigenetic regulators Halmstad University, Sweden Abdurrahman Tufan, Gazi University, Turkey *Correspondence: INTRODUCTION Chao Liang [email protected] Rheumatoid arthritis (RA) is classified as a systemic poly-articular chronic autoimmune joint † disease that primarily affects hands and feet. -

Extrinsic Targeting Strategies Against Acute Myeloid Leukemic Stem Cells Noureldien H
Integrative Cancer Science and Therapeutics Review Article ISSN: 2056-4546 Extrinsic targeting strategies against acute myeloid leukemic stem cells Noureldien H. E. Darwish1,2 and Shaker A. Mousa2* 1Department of Clinical Pathology, Hematology Unit, Mansoura University, Egypt 2The Pharmaceutical Research Institute, Albany College of Pharmacy and Health Sciences (ACPHS), USA Abstract Despite advances in the treatment of acute myeloid leukemia (AML), patients still show high relapse and resistance against conventional chemotherapy. This resistance is related to a small clone referred to as Leukemia Stem Cells (LSCs). New targeted strategies are directed against the LSCs’ extrinsic regulators including their microenvironment such as a CXCR4 antagonist that is used to interfere with LSCs’ homing. Targeting LSCs’ surface molecules such as CD33 for selective elimination of LSCs has variable degrees of success that may require further assessments. Trials with CARs cells were effective in eradication of acute lymphoblastic leukemia, and they may have an effective role also in AML. Other strategies are directed against the intrinsic regulators such as self-renewal mechanisms and epigenetic reprogramming of LSCs. This review highlights targeting of the extrinsic regulators of the LSCs and identifies biological differences between them and normal hematopoietic stem cells. Introduction LSCs theory and properties Acute myeloid leukemia (AML) is a hematological disorder LSCs are able to divide to progeny clonogenic blast cells, leading to characterized by a malignant clone thought to be derived from a small the concept that AML is arranged in a hierarchy, with the LSCs present number of cells known as leukemic stem cells (LSCs). LSCs have a at the apex and the more “differentiated” blasts representing the main great ability for limitless self-renewal and also generation of leukemic tumor bulk [7]. -

New Strategies in Myeloproliferative Neoplasms: the Evolving Genetic and Therapeutic Landscape Ami B
CCR New Strategies Clinical Cancer Research New Strategies in Myeloproliferative Neoplasms: The Evolving Genetic and Therapeutic Landscape Ami B. Patel1, Nadeem A. Vellore2, and Michael W. Deininger3 Abstract The classical BCR–ABL1-negative myeloproliferative neo- off-target toxicities and, as monotherapy, has shown limited plasms (MPN) include essential thrombocythemia (ET), poly- effects on mutant allele burden. In this review, we discuss the cythemia vera (PV), and myelofibrosis (MF). Although these genetic heterogeneity contributing to the pathogenesis of clonal disorders share certain clinical and genetic features, MF MPNs, focusing on novel driver and epigenetic mutations and in particular is distinct for its complex mutational landscape, how they relate to combination therapeutic strategies. We severe disease phenotype, and poor prognosis. The genetic discuss results from ongoing studies of new JAK inhibitors and complexity inherent to MF has made this disease extremely report on new drugs and drug combinations that have dem- challenging to treat. Pharmacologic JAK inhibition has proven onstrated success in early preclinical and clinical trials, includ- to be a transformative therapy in MPNs, alleviating symptom ing type II JAK inhibitors, antifibrotic agents, and telomerase burden and improving survival, but has been hampered by inhibitors. Clin Cancer Res; 22(5); 1037–47. Ó2016 AACR. Disclosure of Potential Conflicts of Interest M.W. Deininger reports receiving commercial research grants from Bristol-Myers Squibb, Celgene, Gilead, and Novartis, and is a consultant/ advisory board member for ARIAD Pharmaceuticals, Bristol-Myers Squibb, Incyte, Novartis, and Pfizer. No potential conflicts of interest were disclosed by the other authors. Editor's Disclosures The following editor(s) reported relevant financial relationships: J.L. -
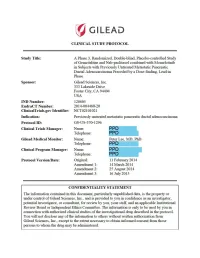
Study Protocol: Amendment 3
(!') GILEAU CLINICAL STUDY PROTOCOL Study Title: A Phase 3, Randomized, Double-blind, Placebo-controlled Study of Gemcitabine and Nab-paclitaxel combined with Momelotinib in Subjects with Previously Unu·eated Metastatic Pancreatic Ductal Adenocarcinoma Preceded by a Dose-fmding, Lead-in Phase Sponsor: Gilead Sciences, Inc. 333 Lakeside Drive Foster City, CA 94404 USA IND Number: 120605 EudraCT Number: 2014-004480-20 ClinicalTrials.gov Identifier: NCT021 01021 Indication: Previously unu·eated metastatic pancreatic ductal adenocarcinoma Protocol ID: GS-US-370-1296 Clinical Trials Manager: Name: PPD Telephone: PPD Gilead Medical Monitor: Name: Peter Lee, MD, PhD Telephone: PPD Clinical Program Manager: Name: PPD Telephone: PPD Protocol Version/Date: Original: 11 Febmary 2014 Amendment 1: 14 March 2014 Amendment 2: 25 August 2014 Amendment 3: 16 July 2015 CONFIDENTIALITY STATEMENT The inf01mation contained in this document, pruiicularly unpublished data, is the prope1iy or under conu·ol of Gilead Sciences, Inc., and is provided to you in confidence as an investigator, potential investigator, or consultant, for review by you, your staff, and an applicable Institutional Review Board or Independent Ethics Committee. The infonnation is only to be used by you in connection with authorized clinical studies of the investigational dmg described in the protocol. You will not disclose any of the infonnation to others without written authorization from Gilead Sciences, Inc., except to the extent necessa1y to obtain infonned consent from those persons