Maryland State Trauma Registry Data Dictionary for Adult Patients April 21
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MGUH) / Lombardi Comprehensive Cancer Center (LCCC)
DISTRICT OF COLUMBIA DEPARTMENT OF HEALTH STATE HEALTH PLANNING AND DEVELOPMENT AGENCY 899 North Capitol Street, NE WASHINGTON, DC 20002 APPLICATION FOR CERTIFICATE OF NEED Registration No. 12-3-9 Establishment of a Proton Therapy Service at MedStar Georgetown University Hospital (MGUH) / Lombardi Comprehensive Cancer Center (LCCC) ~ kwiktag 090 761 842 EXHIBIT NOTEBOOK October 24, 2012 2012 Establishment of a Proton Therapy Service at MedStar Georqetown University Hospital (MGUH) / Lombardi Comprehensive Cancer Center (LCCC) APPLICATION FOR CERTIFICATE OF NEED Registration No.12-3-9 EXHIBIT LIST Exhibit 1: MGUH Incorporation documents Exhibit 2: Service Area Map Exhibit 3: MGUH Magnet Certification by the American Nurses Credentialing Center Exhibit 4: Mentoring Program Exhibit 5: Georgetown Excellence in Nursing Science and Practice Scholarship Exhibit 6:2013 Benefits Guide Exhibit 7: Mevion System Build Agreement Exhibit 8: Architectural Drawings of Proposed Facility Exhibit 9: Patient Rights and Responsibilities Exhibit 10: MGUH Policy on Patient Rights and Responsibilities Exhibit 11: MGUH Community Health Assessment Exhibit 12: Americans with Disabilities Act ("ADA") Policy Exhibit 13: MGUH Financial Statement on Charitable Care Exhibit 14: MGUH Certificate of Accreditation by The Joint Commission Exhibit 15: MGUH D.C. Department of Health License Exhibit 16: MGUH Rules and Regulations of the Professional Staff Exhibit 17: MGUH Policy on the Documentation of Licensure, Certification, and Registration of Professional Staff Exhibit -

Maryland Hospitals by County 2014
Maryland Hospital Association 2014 Member Hospitals by County 57 6 Allegany 43 Garrett 31 Cecil Washington Carroll 36 8 Harford Baltimore 54 46 12 Frederick 11 1340 34 53 23 Baltimore Kent Howard City 50 16 Montgomery 26 44 1 2 20 Queen 39 Anne Anne's 33 15 9 Arundel 3 42 56 32 24 37 Caroline 21 41 Prince George's Talbot 52 10 27 29 49 Calvert Baltimore City Charles 7 51 48 45 19 Dorchester 30 18 5 55 17 Wicomico 47 14 4 38 St. Mary's 28 35 25 Worcester Somerset Hospital Name Number Hospital Name Number Hospital Name Number 22 Adventist Behavioral Health 1 Levindale Hebrew Geriatric Center & Hospital 21 Sinai Hospital of Baltimore 41 Adventist Rehabilitation Hospital of Maryland 2 McCready Foundation 22 Suburban Hospital 42 Anne Arundel Medical Center 3 MedStar Franklin Square Medical Center 23 Union Hospital 43 Atlantic General Hospital 4 MedStar Good Samaritan Hospital 24 Univ of MD Baltimore Washington Medical Ctr 44 Bon Secours Baltimore Health System 5 MedStar Harbor Hospital 25 Univ of MD Charles Regional Medical Center 45 Univ of MD Harford Memorial Hospital 46 Brook Lane 6 MedStar Montgomery Medical Center 26 Calvert Memorial Hospital 7 MedStar Southern Maryland Hospital Center 27 University of Maryland Medical Center 47 Univ of MD Medical Center Midtown Campus 48 Carroll Hospital Center 8 MedStar St. Mary’s Hospital 28 Doctors Community Hospital 9 MedStar Union Memorial Hospital 29 Univ of MD Rehabilitation & Orthopaedic Inst 49 Fort Washington Center Medical Center 10 Mercy Medical Center 30 Univ of MD Shore Medical Ctr at Chestertown 5050 Frederick Regional Health System 11 Meritus Medical Center 31 Univ of MD Shore Medical Ctr at Dorchester 51 Garrett County Memorial Hospital 12 Mt. -

Medstar Harbor Hospital (Mhh) Conducted a Community Health Needs
Return of Organization Exempt From Income Tax OMBÀ¾µ¼ No. 1545-0047 Form 990 Under section 501(c), 527, or 4947(a)(1) of the Internal Revenue Code (except private foundations) IDo not enter Social Security numbers on this form as it may be made public. Open to Public Department of the Treasury I Internal Revenue Service Information about Form 990 and its instructions is at www.irs.gov/form990. Inspection A For the 2018 calendar year, or tax year beginning 07/01 , 2018, and ending 06/30 , 20 19 C Name of organization D Employer identification number B Check if applicable: HARBOR HOSPITAL, INC. Address change Doing Business As 52-0491660 Name change Number and street (or P.O. box if mail is not delivered to street address) Room/suite E Telephone number Initial return 3001 SOUTH HANOVER STREET (410) 772-6721 Terminated City or town, state or province, country, and ZIP or foreign postal code Amended BALTIMORE, MD 21225-1233 G Gross receipts $ 191,587,141. return Application F Name and address of principal officer: STUART LEVINE, M.D. H(a) Is this a group return for Yes X No pending subordinates? 3001 SOUTH HANOVER STREET,J BALTIMORE, MD 21225 H(b) Are all subordinates included? Yes No I Tax-exemptI status: X 501(c)(3) 501(c) ( ) (insert no.) 4947(a)(1) or 527 If "No," attach a list. (see instructions)I J Website: WWW.HARBORHOSPITAL.ORG I H(c) Group exemption number K Form of organization:X Corporation Trust Association Other L Year of formation: 1903 M State of legal domicile: MD Part I Summary 1 Briefly describe the organization's mission or most significant activities: HARBOR HOSPITAL IS COMMITTED TO QUALITY, CARING, AND SERVICE FOR OUR PATIENTS AND OUR COMMUNITIES. -
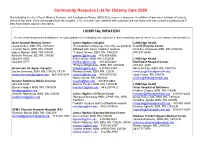
Community Resource List for Ostomy Care 2020
Community Resource List for Ostomy Care 2020 The following is a list of local Wound, Ostomy, and Continence Nurses (WOCN) to use as a resource. In addition, there are a number of ostomy clinics in the area. Once discharged from the hospital, LTC, or home care, patients with ostomies are not alone and can contact a professional if they have future ostomy care needs. HOSPITAL INPATIENT *Denotes that this particular facility/nurse accepts outpatient referrals/physician orders for treatment and your patient can be seen for ostomy related problems. Anne Arundel Medical Center Johns Hopkins Hospital LifeBridge Health Joyce Onken, BSN, RN, CWOCN (For outpatient follow-up, may only see patients Carroll Hospital Center Jennifer Davis, BSN, RN, CWON affiliated with Johns Hopkins Hospital) Christine Arrowood, BSN, RN, CWOCN Agnes Mpanja, BSN, RN, CWCN *Jessica Groom, BSN, RN, CWOCN 410-871-6839 Michelle Perkins, BS, RN, CWON [email protected] 410-955-6668 443-481-5508 Kelly Heffron, BSN, RN, CWOCN LifeBridge Health 443-481-5177 [email protected] 410-955-6647 Northwest Hospital Center *Frances Magliacane, BSN, RN, CWOCN 410-521-2200 Ascension St. Agnes Hospital [email protected] 410-955-5367 Missy McCoy, MSN, RN, CWOCN Sacha Simmons, BSN, RN, CWON, CFCN Rhonda Sewell, BSN, RN, COCN [email protected] [email protected] 667-234-3034 [email protected] 443-287-0392 Judy Coster, RN, CWCN Nancy Sujeta, RN, CWOCN [email protected] Greater Baltimore Medical Center [email protected] 410-955-6667 443-849-6992 Melissa Venker, BSN, -

Annotated List of Past Activities on Alcoholism in Maryland: 1935-1960
^. ~^ ANNOTATED LIST OF PAST ACTIVITIES ON ALCOHOLISM IN MARYLAND: 1935-1960 (Published and Unpublished) * * * * * * # * MARYLAND COMMISSION ON ALCOHOLISM February 17, 196l V 8U5'5&j MARYLAND COMMISSION ON ALCOHOLISM Lewis P, Gundry, M.D., Chairman Leo Bartemeier, M.D. William L. Clapp Mrs. Roland B. Duke John McGrath Alfred P. Quimby Rowland Posey, Secretary Staff Harrison M. Trice, Ph.D. Howard M. Bubert, Jr. Lillian M. Snyder * CONTENTS Page PREFACE •. i HOW TO USE THIS BOOK 1 LIST OF PAST ACTIVITIES ON ALCOHOLISM IN MARYLAND 2 APPENDIXES iS INDEX OF AUTHORS 65 PREFACE In the course of collecting data on alcoholism in Maryland from September 1 to December 1, i960, frequent references were made from time to time to previous studies, projects, and researches on alcoholism. Was the i960 Commission on Alcoholism duplicating what had been done before? What was the result of these past studies? If successful, had they been continued? If not, why not? This Annotated List and brief descriptions of some of the previous activities have been prepared for use by anyone interested in the problem of alcoholism in Maryland. We wish to acknowledge the assistance of the following libraries, organizations, and individuals: Enoch Pratt Free Library Medical & Chirurgical Faculty of Maryland Library Health Sciences Library, Uhiversity of Maryland Henry Phipps Library, Johns Hopkins University Homewood Library, Johns Hopkins University Welch Medical Library, Johns Hopkins University State Department of Health Library Old Age, Survivors', Disability Insurance Library Peabody Library Legislative Council, Reference Library Spring Grove State Hospital Library Springfield State Hospital Library Crownsville State Hospital Library State Department of Health, Bureau of Preventive Medicine, Division of Mental Health & Child Health State Department of Mental Hygiene, Central Office State Department of Mental Hygiene, Department of Research Health & Welfare Council of Baltimore Area, Inc. -

2016 Annual Report
Alvin & Lois Lapidus Cancer Institute 2016 ANNUAL REPORT Alvin & Lois Lapidus Cancer Institute TABLE OF LETTER FROM THE CANCER COMMITTEE CHAIRWOMAN, ABBIE FIELDS, M.D. 1 CONTENTS CANCER LIAISON PHYSICIAN SUMMARY, DONA HOBART, M.D. 2 LETTER FROM MARVIN JACK FELDMAN, M.D. MEDICAL DIRECTOR 3 SINAI HOSPITAL OF BALTIMORE AND NORTHWEST HOSPITAL 4-5 A LifeBridge Health Center Commission On Cancer Program CANCER SERVICES AVAILABLE AT SINAI HOSPITAL 6 OF BALTIMORE AND NORTHWEST HOSPITAL ALVIN & LOIS LAPIDUS CANCER INSTITUTE 7 THE HERMAN & WALTER SAMUELSON BREAST CARE CENTER SINAI HOSPITAL OF BALTIMORE AND NORTHWEST HOSPITAL THE QUALITY MEASURES FOR BREAST CANCER DIAGNOSTICS AND TREATMENT 8-9 LUNG CANCER FACTS – Lung Screening Program 10 THE ROLE OF OUR PATHOLOGY TEAM 11 THE ROLE OF OUR DIAGNOSTIC RADIOLOGISTS 12 PSYCHOSOCIAL HEALTH AND THE CANCER PATIENT 13 COMPLEMENTARY HEALTH SERVICES 14 2016 PATIENT NAVIGATION PROGRAM ACTIVITIES / INITIATIVES 15 2016 PREVENTION, EDUCATION, COMMUNITY OUTREACH 16 AND SCREENING ACTIVITIES / INITIATIVES THE CANCER REGISTRY 17 THE NATIONAL CANCER DATABASE 18 2015 CANCER REGISTRY STATISTICAL YEAR 19-20 2016 CANCER COMMITTEE MEMBERS 21 LETTER The cancer program at the Alvin & Lois Lapidus Cancer Institute, caring for patients at both FROM THE Sinai and Northwest hospital, in Baltimore City and County, proudly entered into collaboration with the William E. Kahlert Regional Cancer Center at Carroll Hospital in Westminster, Md. CANCER This collaboration contributed to the LifeBridge Health cancer program obtaining status of Integrated Network Cancer Program (INCP) through the American College of Surgeons COMMITTEE Commission on Cancer. Through this network, we are able to offer cutting-edge, evidence- CHAIRWOMAN based cancer care to patients within their own community-based institutions. -
User's Manual
MIEMSS Commercial Ambulance Licensing and Regulation COMMERCIAL—MAIS USER’S MANUAL July 2000 REV. 07/05/00 Table of Contents Page General Form Identification 1 Sample Commercial MAIS form. 2 Section 1 Location, Patient, and Provider Information 3 Section 2 Unit, Crew, Date, Origen and Destination Information 4 Section 3 Documentation of Response Times and Facility Codes 5 Section 4 Vital Signs, Transport Reason, Signs and Symptoms 6 Section 5 Airway/Ventilation, Circulation, and Other 7 Section 6 Care, Skills, Medications and Special Items 9 Section 7 Narrative 10 Appendix A Receiving Facility Codes 11 b GENERAL: FORM IDENTIFICATION MIEMSS RECORD—the TOP COPY is the SCANNABLE document to be submitted to MIEMSS. OFFICIAL COPY–is the legal copy of the record and should be retained at the company level. HOSPITAL COPY–is the copy to be left at the reciving facility. PLEASE DO NOT: Staple, tape, bend, or otherwise mutilate the top copy. This copy is fed through a scanner, stapling, taping, or attaching items such as ECG strips creates a significant problem. 1 2 SECTION 1: LOCATION, PATIENT, AND PROVIDER INFORMATION Response Location Record the location where you picked up the patient. Be as specific as possible. Ex. St. Joseph Hospital, Room 712B or 125 Smith Street, Bowie, MD Destination Record the location where you delivered the patient. Be as specific as possible. Ex. Garrett Memorial Hosp., Room 301 or 765 North Prospect Avenue, Cumberland, MD Patient Name Print the patient’s last name, first name, middle initial. Patient Address Print the patient’s residential address—include street address, city, and zip code. -

[email protected]
Number Refresher Training Names E-Mail Address Business Name County Zip Code Business Phone RPS0001 NEED REFRESHER David L. Barnes [email protected] MAPCB Baltimore 21022 (866)537-5340 RPS0002 NEED REFRESHER Lauretha Vargas [email protected] Phoenix Health Center Washington 21740 (240)420-0000 RPS0003 5/9/2019 LaToya Nkongolo [email protected] Nick's Place Prince George's 20705 (301)937-4356 RPS0004 NEED REFRESHER Almustaphael Al-Kahlil-Bey [email protected] Interdynamics Inc. Prince George's 20706 (301)306-4590 RPS0005 8/10/2018 Stacie Grogin [email protected] Phoenix Health Center Washington 21740 (240)420-0000 RPS0006 2/27/2019 Kheninh Daniels [email protected] Maryand Recovery Organizations Connecting Communities 21227 (410)522-2230 RPS0007 6/21/2019 Denise Marcell Camp [email protected] On our Own of Maryland, Inc. Baltimore 21227 (410)646-0262 x-26 RPS0008 RPS0009 RPS0010 RPS0011 2/27/2019 Monica A. Kirkpatrick [email protected] Mountain Manor Tx. Ctr. Frederick 21701 (301)662-1407 RPS0012 NEED REFRESHER Willie J. Wilson [email protected] Baltimore Crisis Response 21231 (410)433-5255 x-348 RPS0013 NEED REFRESHER Charles Williams [email protected] In & Out Program Prince George's 20748 (202)230-7992 RPS0014 NEED REFRESHER George Phillips [email protected] Anne Arundel County Dept. of Health Anne Arundel 21060 (410)222-0119 RPS0015 NEED REFRESHER Wayne Allen [email protected] State of Maryland 21501 (301)777-2346 RPS0016 NEED REFRESHER Debbie D. Andersen [email protected] On Our Own of Howard County Howard 21045 (410)772-7905 RPS0017 NEED REFRESHER Carolyn E. Miller [email protected] Baltimore County Bureau of Behavioral Health Baltimore 21212 (410)887-3828 RPS0018 2/27/2019 Lauren Elaine McCarthy [email protected] Mountain Manor Tx. -

The Maryland Board of Public Works
The Maryland Board of Public Works The Maryland Board of Public Works A History Alan M. Wilner Hall of Records Commission, Department of General Services, Annapolis, MD 21404 Contents FOREWORD Vll PREFACE ix CHAPTER 1. An Overview of Early Policies: To 1825 CHAPTER 2. The First Board of Public Works and the Mania 1 for Internal Improvements, 1825-1850 CHAPTER 3. The Constitutional Convention of 1850-1851 11 CHAPTER 4. The Reign of the Commissioners: 1851-1864 25 CHAPTER 5. The Constitutional Convention of 1864 35 CHAPTER 6. The New Board: 1864-1920 51 CHAPTER 7. The Modern Board: 1920-1960 59 CHAPTER 8. The Overburdened Board: 1960-1983 79 CHAPTER 9. Epilogue 99 APPENDIX A. Commissioners of Public Works and Members of 123 the Board of Public Works, 1851-1983 125 APPENDIX B. Guide to the Records of the Board of Public Works, 1851-1983 127 BIBLIOGRAPHY 185 INDEX 189 The Maryland Board of Public Works, A History, is available from the Maryland Hall of Records, P.O. Box 828, Annapolis, MD 21404. Copyright © 1984 by Alan M. Wilner. Foreword Alan M. Wilner's authorship of the history of the Board of Public Works continues a fine Maryland tradition of jurist-historians that includes Judge Carroll Bond's His- tory of the Court of Appeals and Judge Edward Delaplaine's biography of Governor Thomas Johnson. When I first read Judge Wilner's manuscript in the summer of 1981, it was im- mediately clear that it would provide an excellent introduction to the significant col- lection of archival materials at the Hall of Records relating to the history and work of the Board. -
Download WMTS User Guide
WMTS User Information Guide Powered by Table of Contents Introduction ....................................................................................... 3 Why use WMTS? .............................................................................. 4 Update on WMTS ............................................................................. 6 Register with ASHE .......................................................................... 7 WMTS Frequency Coordination Database ....................................... 9 Pricing Summary ............................................................................ 16 WMTS Deployment Form ............................................................... 17 Radio Astronomy ............................................................................ 21 Hospitals Affected by Carve-out Areas ........................................... 22 Contact Us ...................................................................................... 29 2 WMTS User Information Guide – V 10.1 December 2016 Powered by Introduction In response to growing concerns about interference resulting from new digital television transmitters, low power television transmitters, paging stations, and greater use of private land mobile radio equipment, the Federal Communications Commission (FCC) has done the following: Established the Wireless Medical Telemetry Service (WMTS), dedicating bands of frequencies to promote interference-free operation of medical telemetry systems, Appointed ASHE as the Frequency Coordinator for the -

Opkins Education
Volume X, Issue I Spring 2012 1. Remove scope-of- Discover Johns Hopkins practice barriers. Nursing’s Blueprint 2. Expand doctoral nursing education opportunities for for the nurses to lead and diffuse collaborative Future improvement efforts. 3. Implement nurse residency programs. 4. Increase the proportion of nurses with a baccalaureate degree to 80 percent by 2020. 5. Double the number of nurses with a doctorate by 2020. The Doctor of Philosophy (PhD) for research leaders. 6. Ensure that nurses engage in lifelong learning. Advance the science of nursing and healthcare. 7. Prepare and enable nurses to lead The Doctor of Nursing Practice (DNP) for clinical leaders. change to advance health. Advance the practice of nursing and improve health outcomes. 8. Build an infrastructure for the collection and analysis of interprofessional healthcare workforce data. Choose your path at the Johns Hopkins University School of Nursing—a place where exceptional people discover possibilities that forever change their lives www.nursing.jhu.edu/doctoral and the world. Inside: 26 Doubling the Number of 32 Interprofessional Education Nurses with Doctorates Initiatives at Hopkins JOHNS HOPKINSVolume X, Issue I Spring 2012 A publication of the Johns Hopkins University School of Nursing, the Johns Hopkins Nurses’ Alumni Association, and the nursing departments of the Johns Hopkins-affiliated hospitals Features 26 Higher Education by Jennifer Walker The data is compelling. The American Association of Colleges of Nursing predicts the country will lose 260,000 nurses by 2025, including thousands of nursing faculty needed to educate new nurses. In response, the Institute of Medicine recommends universities double the number of doctoral-prepared nurses. -

Carroll Hospital's Clinical Decision Unit
JANUARY 2017 NONPROFIT ORG U.S. POSTAGE PAID WESTMINSTER, MD PERMIT NO. 348 SCOPE 200 Memorial Avenue Westminster, MD 21157 A PUBLICATION FOR THE MEDICAL STAFF OF CARROLL HOSPITAL CarrollHospitalCenter.org Physicians Message from President Leslie Simmons, R.N., F.A.C.H.E. of the Month As we near the halfway mark of fiscal year 2017, I wanted to remind everyone of our organization’s corporate goals and the essential role that you, as a member of our medical staff, play in helping us achieve them. Every year, we set goals for the organization to challenge ourselves to raise the bar and continue our focus on providing high quality care and the best patient experience. For FY17, the LifeBridge Health corporate goals for each hospital fall under the following categories: August 2016 • Appropriate Utilization — ensuring patients are receiving the right care in the right Melvin Yeshnik, M.D., setting and that they have the resources they need when they go home to prevent a OB/GYN readmission. • Patient Experience — improving customer service scores (Hospital Consumer Assessment of Healthcare Providers and Systems [HCAHPS] — or patients’ perceptions of their care). • Employee and Physician Engagement — finding ways to enhance our employees’ and physicians’ involvement in their departments, increase their satisfaction and make LifeBridge Health the best place to work and practice medicine. • Financial — accomplishing all of the above while meeting our financial targets. Based on our reimbursement model, the quality of care we provide can have a big impact on our finances. September 2016 Medical and Carroll Health Group Staff – Additions Douglas Weber, M.D., Our success in achieving these goals depends on every medical staff member and employee understanding his or emergency medicine Department of Diagnostic Wendy Miller, M.D.