ASN Program Have Assumed Important Roles in Nursing and Health Care in a Variety of Care Settings
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nursing's Future Comes to Life in Driscoll Hall
SPRING/ SUMMER 2 0 0 9 A PUBLICATION OF THE VILLANOVA UNIVERSITY COLLEGE OF NURSING Nursing’s Future Comes to Life in Driscoll Hall College of Nursing Board of Consultors gueras NO la O • H.E. Dr. Ali Al-Moosa A P • Mr. Thomas E. Beeman • Rear Adm. Christine M. Bruzek-Kohler • Dr. Helen R. Connors • Mrs. Tara M. Easter • Rear Adm. (Ret.) James W. Eastwood • Mr. Stephen P. Fera • Mr. Daniel Finnegan • Dr. M. Louise Fitzpatrick, Ex officio • Ms. Margaret M. Hannan • Veronica Hill-Milbourne, Esq. • Mr. Richard J. Kreider • Mr. J. Patrick Lupton • Dr. Thomas F. Monahan • Dr. Mary D. Naylor • Mr. James V. O’Donnell Mrs. Sue Stein, staff Mark your calendar! October 4 Undergraduate Open House November 16 Annual Distinguished Lecture Dr. Mary D. Naylor ’71 B.S.N., Ph.D., R.N., FAAN, the Marian S. Ware In the lobby of Driscoll Hall, the Crucifix, designed and painted in the Byzantine style by Professor in Gerontology and director Edward Ruscil, includes depictions of the Visita- of the Center for Health Transitions, tion and the parable of the Good Samaritan. School of Nursing, University of Pennsylvania Villanova Nursing Vol. 28 No. 1 Spring/Summer 2009 Features On the Cover: In May, the Class of 2009 became the first B.S.N. class Driscoll Hall Advances Nursing’s Future ........................2 to graduate from the College of Nursing following the opening of Driscoll Hall last fall. Thank You to the Donors .........................................11 Editorial Board College Launches Campaign Ann Barrow McKenzie ’86 B.S.N., ’91 M.S.N., R.N., Editor Promoting Nursing ....................... -

Who We Are Dean’S Welcome
WHO WE ARE DEAN’S WELCOME Dear friends, This month I took part in my fifth year of graduation and commencement ceremonies at NYU as dean. What an excit- ing time! To see students work so hard and then finally walk across the stage to receive their diplomas, and, for many, enter a new stage in their lives, is the highlight of my year. We have prepared our recent graduates to become leaders at a critical moment in healthcare—a time to reimagine how best to deliver high-quality, affordable care. As nurses, we are uniquely positioned to develop and implement the inno- vation required to tackle this challenge, and more broadly, the world’s most pressing issues like poverty, mental health, climate change, chronic illness, substance abuse, and the effects of an aging population. We know our new graduates—the extraordinary class of 2017—will rise to the challenge. I hope you will join me in saluting them. In the spring issue of NYU Nursing, we are proud to STATEMENT ON DIVERSITY showcase who we are and you will: AND INCLUSION • Explore the US-China relationship and the two countries’ WELCOME. shared healthcare challenges; NEW YORK UNIVERSITY RORY MEYERS COLLEGE • OF NURSING is committed to the inclusion and Meet Assistant Professor Yzette Lanier, a developmental support of individuals and ideas from all who psychologist studying HIV behavioral intervention; comprise our multicultural community. The College embraces the richness of diversity in its • Discover how first-generation college students integrate multiple dimensions that exist within and around into the classroom and campus life; us, including: race, ethnicity, nationality, class, sex, gender identity/expression, ability, faith/belief, • Experience what it’s like for a male nurse midwife, sexual orientation, and age. -

The Nursing Alumni Association at 20 Years Page 2
learning the hbrighamealer’s young university college of nursin artg Fall 2019 The Nursing Alumni Association at 20 Years Page 2 Night of Nursing Expansion Page 8 New Faculty Page 20 Dean’s Message learning the Fall 2019 The Family Connection: It’s All Relative healer’s art I recently read an entry from urban- the college alumni association supports Just as your own family dictionary.com that defined family as activities to enhance student learning, a group of people “who genuinely love, foster employment for graduates, and can provide strength trust, care about, and look out for each create collegial relationships that build other. Real family is a bondage that the individual, the profession, and the . the college alumni cannot be broken by any means.” reputation of Brigham Young University. That got me thinking about the “fami- A sense of belonging supports the mis- association supports lies” we have here at the College of Nursing. sion and goals of the college by rekindling activities to enhance In each of the six nursing semesters, the spirit of the BYU nursing experience, individuals sustain one another as they encouraging financial contributions, pro- student learning, advanced together through the program moting a sense of community, and har- for three years. They learn to value mem- monizing nursing with gospel principles foster employment for 2 8 20 bers for their unique abilities and assets, through knowledge, faith, and healing. rather than as competition; spending This issue features stories of ways to graduates, and create hours as one group establishes our car- connect with the college alumni asso- collegial relationships ing heritage. -

Search Titles and Presenters at Past AAHN Conferences from 1984
American Association for the History of Nursing, Inc. 10200 W. 44th Avenue, Suite 304 Wheat Ridge, CO 80033 Phone: (303) 422-2685 Fax: (303) 422-8894 [email protected] www.aahn.org Titles and Presenters at Past AAHN Conferences 1984 – 2010 Papers remain the intellectual property of the researchers and are not available through the AAHN. 2010 Co-sponsor: Royal Holloway, University of London, England September 14 - 16, 2010 London, England Photo Album Conference Podcasts The following podcasts are available for download by right-clicking on the talk required and selecting "Save target/link as ..." Fiona Ross: Conference Welcome [28Mb-28m31s] Mark Bostridge: A Florence Nightingale for the 21st Century [51Mb-53m29s] Lynn McDonald: The Nightingale system of training and its influence worldwide [13Mb-13m34s] Carol Helmstadter: Nightingale Training in Context [15Mb-16m42s] Judith Godden: The Power of the Ideal: How the Nightingale System shaped modern nursing [17Mb-18m14s] Barbra Mann-Wall: Nuns, Nightingale and Nursing [15Mb-15m36s] Dr Afaf Meleis: Nursing Connections Past and Present: A Global Perspective [58Mb-61m00s] 2009 Co-sponsor: School of Nursing, University of Minnesota September 24 - 27, 2009 Minneapolis, Minnesota Paper Presentations Protecting and Healing the Physical Wound: Control of Wound Infection in the First World War Christine Hallett ―A Silent but Serious Struggle Against the Sisters‖: Working-Class German Men in Nursing, 1903- 1934 Aeleah Soine, PhDc The Ties that Bind: Tale of Urban Health Work in Philadelphia‘s Black Belt, 1912-1922 J. Margo Brooks Carthon, PhD, RN, APN-BC The Cow Question: Solving the TB Problem in Chicago, 1903-1920 Wendy Burgess, PhD, RN ―Pioneers In Preventative Health‖: The Work of The Chicago Mts. -
Practical Nursing Clinical Uniform Check List
PRACTICAL NURSING PROGRAM STUDENT HANDBOOK 2017-2018 Department of Nursing Division of Nursing and Allied Health Revised 7/24/2017 Page 1 Contents Equal Opportunity Statement ......................................................................................................... 4 Introduction .................................................................................................................................... 4 Mission ............................................................................................................................................ 4 Vision ............................................................................................................................................... 4 Value Statement ............................................................................................................................. 4 Shared Values.................................................................................................................................. 5 Curriculum Organizing Framework ................................................................................................. 6 Department of Nursing Curriculum Organizing Framework Model ....................................................... 6 Program Outcomes ......................................................................................................................... 7 Student Learning Outcomes ........................................................................................................... 7 Program -
Nursing Student Handbook Spring 2021
Nursing Student Handbook Spring 2021 TABLE OF CONTENTS INTRODUCTION / WELCOME ...................................................................................................................................... 6 CONTACT INFORMATION ............................................................................................................................................. 7 TJC NURSING PHILOSOPHY .......................................................................................................................................... 8 Vision ................................................................................................................................................................................ 8 Program Mission ............................................................................................................................................................ 8 Program Values .............................................................................................................................................................. 8 TJC Nursing Conceptual Framework ......................................................................................................................... 9 CONDITIONAL ACCEPTANCE POLICIES .................................................................................................................. 14 Cardiopulmonary Resuscitation (CPR) ..................................................................................................................... 14 Criminal Background -

Exploring Gendered and Sexed Relations in Nursing
MEN NURSES AND MASCULINITIES: EXPLORING GENDERED AND SEXED RELATIONS IN NURSING SY Joan Alice Evans Submitted in partial fulfillrnent of the requirernents for the degree of Doctor of Philosophy Dalhousie University Halifax, Nova Scotia August, 2001 O Copyright by Joan Alice Evans, 2001 National Library Bibliothèque nationale du Canada Acquisitions and Acquisitions et Bibliographie Services services bibliographiques 395 Wellington Street 395, rue Wellington Ottawa ON KIA ON4 Otbwa ON KlAûN4 Canada Canada The author has granted a non- L'auteur a accordé une licence non exclusive licence allowing the exclusive permettant à la National Library of Canada to Bibliothèque nationale du Canada de reproduce, loan, distnbute or sell reproduire' prêter, distribuer ou copies of this thesis in microform, vendre des copies de cette thèse sous paper or electronic formats. la fome de microfiche/film, de reproduction sur papier ou sur format électronique. The author retains ownership of the L'auteur conserve la propriété du copyright in this thesis. Neither the droit d'auteur qui protège cette thèse. thesis nor substantial extracts from it Ni la thèse ni des extraits substantiels may be printed or otherwise de celle-ci ne doivent être imprimés reproduced without the author's ou autrement reproduits sans son permission. autorisation. This research is dedicated to my father Maxwell James Evans who instilled in his three daughters the value of education the importance of independence and the rewards of hard work TABLE OF CONTENTS Abstract ....................................................... ix Acknowledgments ............................................... x Prologue ....................................................... 1 Thepurpose .............................................. 3 The Structure of the Thesis ................................... 4 Chapter 1: Men Nurses and the Gendered Nature of Nuning ........... -
BSN Completion Program Handbook for Students
BSN COMPLETION PROGRAM HANDBOOK FOR STUDENTS University of Wisconsin-Eau Claire COLLEGE OF NURSING AND HEALTH SCIENCES July 2021 Handbook for BSN Completion Program Students PREFACE All students will find it helpful to study this handbook. It is updated every six months to reflect new or changed policies. It is important for you to be aware of the information contained herein to facilitate your program and to protect you and your clients. We wish to create an inclusive and supportive environment that motivates everyone to do their best work and learn and grow as individuals. Table of Contents I. Introduction .................................................................................................................................................................. 1 II. History of the BSN Completion Program ...................................................................................................................... 3 History of Nursing Attire ............................................................................................................................................................... 15 III. Nursing Building Educational Facilities ...................................................................................................................... 17 Eau Claire Site - College of Nursing and Health Sciences Building .................................................................................................. 17 Nursing Department Educational Facilities - Marshfield Site at UW-Stevens Point at Marshfield -

School of Nursing Student Handbook
Please click on the program link to navigate to that section. Clemson University SCHOOL OF NURSING College of Behavioral, Social, and Health Sciences UNDERGRADUATE BS-T AND BS-A HANDBOOK 2019- 2020 ii CLEMSON UNIVERSITY School of Nursing College of Behavioral, Social and Health Sciences TABLE OF CONTENTS SECTION I: THE SCHOOL OF NURSING .................................................................................4 Welcome to the School of Nursing .....................................................................................4 The School of Nursing Overview ..........................................................................................4 Accreditation: Commission on Collegiate Nursing Education (CCNE)................................. 5 Statement of Equal Opportunity .........................................................................................5 School of Nursing Organizational Chart...............................................................................6 School of Nursing Mission, Vision, and Goals...................................................................... 7 SECTION II: OBJECTIVES & CURRICULUM INFORMATION .................................................. 8 Baccalaureate Program Overview & Objectives ................................................................8 2019-2020 Bachelor of Science in Nursing Curriculum Plan ................................................9 Bachelor of Science in Nursing Course Descriptions .................................................... 10-12 Honors Program -

Alverno's Nursing Tradition
Alverno’s Nursing Tradition: From Sacred Heart School of Nursing to the JoAnn McGrath School of Nursing September 22, 1930 - Today Alverno’s Nursing Tradition - The Sacred Heart Years To tell the story of the Alverno College School of Nursing, one has to step back in time and look at the nursing roots laid down by the School Sisters of Saint Francis. The School Sisters of Saint Francis established the Sacred Heart Sanitarium under the guidance of their foundress, Venerable Mother M. Alexia Hoell. Built on land adjacent to the School Sisters of Saint Francis St Joseph Convent, the sanitarium was located at 1545 South Layton Boulevard and opened December 1893. It would provide a vehicle to further the Sisters’ philosophy of ministering to the health needs of others. Alverno’s Nursing Tradition - The Sacred Heart Years Sisters, trained in the methods of nursing and ministering to the sick, would serve as the sanitarium’s nursing instructors. They would teach the young women entering the religious life and prepare them for the field of nursing. Mother M. Alexia was instrumental in bringing hydrotherapy techniques used in Europe to the sanitarium. Doctors were appointed to assist the Sisters in the nurses’ training process. Expansion and reorganization of the sanitarium’s medical therapy regime took place in 1902. Additional doctors, specializing in specific diseases and disorders, were appointed to the staff to help with the increased patient load. Patients with various types of ailments, ranging from physical to mental diseases, were coming to the sanitarium for treatments. Alverno’s Nursing Tradition - The Sacred Heart Years Mother M. -

Nursing Practicum in Kenya 3
THE COLLEGE OF PHARMACY, NURSING, & ALLIED SCIENCES SUMMER ‘12 Nursing practicum in Kenya 3 Student-athletes shine 4 Distinguished alumna offers advice 6 Workforce shortage addressed 8 1 Carla Gross, chair and associate professor Phone: 701-231-7772 E-mail: [email protected] a message from Carla Gross Th is is an exciting time for the nursing profession and nursing education. Since its inclusion in Gallop Poll’s survey of the trustworthiest professions 13 years ago, nursing topped the list for the 12th consecutive year. Other national movements reinforce the public’s trust in nurses. Our country is challenged to balance providing broader access to health care while controlling costs. Nurses will play a key role in addressing these challenges. Th e country relies on advanced practice nurses to meet the growing need for primary care providers. Recommendations in the Aff ordable Care Act (2010) and the Institute of Medicine’s report, “Th e Future of Nursing: Leading Change, Advancing Health” (2010), call for nurses to assume greater leadership roles, collaborate fully with other disciplines and practice to the full extent of their education, training and scope of practice. NDSU is committed to preparing graduates who are up to the challenge. Faculty maintain a rigorous curriculum that meets educational regulations and needs of the practice arena. Both undergraduate and graduate curricula have been revised to meet standards outlined by our accrediting body, the Commission on Collegiate Nursing Education (CCNE) and the N.D. Board of Nursing. Th e department has been preparing for site visits from both entities this past year and a half. -
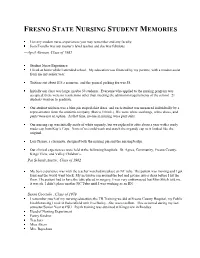
CSU Fresno Student Memories
FRESNO STATE NURSING STUDENT MEMORIES List any student nurse experiences you may remember and any faculty: Joan Fiorello was my master‘s level teacher and she was fabulous —April Aleman, Class of 1985 Student Nurse Experience I lived at home while I attended school. My education was financed by my parents, with a modest assist from me my senior year. Tuition cost about $35 a semester, and the general parking fee was $8. Initially our class was large, maybe 50 students. Everyone who applied to the nursing program was accepted; there were no restrictions other than meeting the admission requirements of the school. 21 students went on to graduate. Our student uniform was a blue pin striped shirt dress, and each student was measured individually by a representative from the uniform company (Barco, I think.) We wore white stockings, white shoes, and pants were not an option. At that time, no one in nursing wore pant suits. Our nursing cap was initially made of white organdy, but we replaced it after about a year with a ready made cap from Kay‘s Caps. None of us could wash and starch the organdy cap so it looked like the original. Lois Pisano, a classmate, designed both the nursing pin and the nursing badge. Our clinical experiences were held at the following hospitals: St. Agnes, Community, Fresno County, Kings View, and Valley Children‘s. —Pat Scheidt Austin , Class of 1962 My best experience was with the teacher watched me place an NC tube. The patient was moving and I got faint and the world went black.