Formulary April
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Summary of Product Characteristics
Health Products Regulatory Authority Summary of Product Characteristics 1 NAME OF THE VETERINARY MEDICINAL PRODUCT Cardisure 3.5 mg/ml Oral Solution for Dogs 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Each ml contains Active substance: Pimobendan 3.5 mg Excipients: Benzyl alcohol (E1519) 1.0 mg For the full list of excipients, see section 6.1. 3 PHARMACEUTICAL FORM Oral Solution. Clear, colourless, semi-viscous liquid. 4 CLINICAL PARTICULARS 4.1 Target Species Dogs. 4.2 Indications for use, specifying the target species For the treatment of canine congestive heart failure originating from valvular insufficiency (mitral and/or tricuspid regurgitation) or dilated cardiomyopathy. 4.3 Contraindications Do not use in cases of hypertrophic cardiomyopathies or clinical conditions where an augmentation of cardiac output is not possible for functional or anatomical reasons (e.g. aortic stenosis). Do not use in dogs with severe impairment of liver function, as pimobendan is metabolised mainly via the liver. Do not use in cases of known hypersensitivity to the active substance or to any of the excipients. 4.4 Special warnings for each target species None known. 4.5 Special precautions for use Special precautions for use in animals The blood glucose should be tested regularly during treatment in dogs with existing diabetes mellitus. Monitoring of cardiac function and morphology is recommended in animals treated with pimobendan (See also section 4.6). Special precautions to be taken by the person administering the veterinary medicinal product to animals Accidental ingestion, especially by a child, may lead to the occurrence of tachycardia, orthostatic hypotension, flushing of the face and headaches. -

Dynamic Analysis of Cardiovascular Drugs Data
Available online www.jocpr.com Journal of Chemical and Pharmaceutical Research, 2014, 6(5):1517-1520 ISSN : 0975-7384 Research Article CODEN(USA) : JCPRC5 Dynamic analysis of cardiovascular drugs data Humei Yang and SunShi The Affiliated Hospital of Qingdao University Medical College , China _____________________________________________________________________________________________ ABSTRACT Cardiovascular disease is an important disease which is a serious hazard to human health, not only that, but the cause is still quite complicated. Therefore, it is very important to carry out research work of cardiovascular drugs in the medical profession. In this article, the money amount sequence method and DDD number sequence method were used to statistically analyze the data of cardiovascular drugs which were purchased by patients in a hospital in Shanghai in 2010-2013 year. The data of cardiovascular drugs second-class hospitals and upper-class hospitals in Shanghai included the drug varieties, prescription medication, the amount of money, which were statistically analyzed in order to provide recommendations for future cardiovascular medication guide. Through this research, we have come to the result that the money of cardiovascular drugs accounts greater of the amount of all of the drugs in the second-class hospitals than that in the upper-class hospitals, and cardiovascular medication amounts, prescriptions, etc of the second-class hospitals and upper-class hospitals had increased than before. Calcium antagonists and angiotensin ⅱ receptor antagonist drugs led occupation, as well as a small amount of varieties of drugs had gone into the top 10 amounts .As for cardiovascular drugs, foreign markets occupy a major market. That is to say that between different levels of hospitals there is some difference in cardiovascular drug use, but the drugs with good effects are already the first choice. -

WO 2016/133483 Al 25 August 2016 (25.08.2016) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization I International Bureau (10) International Publication Number (43) International Publication Date WO 2016/133483 Al 25 August 2016 (25.08.2016) P O P C T (51) International Patent Classification: SHENIA, Iaroslav Viktorovych [UA/UA]; Feodosiyskyy A61L 15/44 (2006.01) A61L 26/00 (2006.01) lane, 14-a, kv. 65, Kyiv, 03028 (UA). A61L 15/54 (2006.01) (74) Agent: BRAGARNYK, Oleksandr Mykolayovych; str. (21) International Application Number: Lomonosova, 60/5-43, Kyiv, 03189 (UA). PCT/UA20 16/0000 19 (81) Designated States (unless otherwise indicated, for every (22) International Filing Date: kind of national protection available): AE, AG, AL, AM, 15 February 2016 (15.02.2016) AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, (25) Filing Language: English DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (26) Publication Language: English HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, (30) Priority Data: MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, a 2015 01285 16 February 2015 (16.02.2015) UA PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, u 2015 01288 16 February 2015 (16.02.2015) UA SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, (72) Inventors; and TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, ZW. -

SNF Mobility Model: ICD-10 HCC Crosswalk, V. 3.0.1
The mapping below corresponds to NQF #2634 and NQF #2636. HCC # ICD-10 Code ICD-10 Code Category This is a filter ceThis is a filter cellThis is a filter cell 3 A0101 Typhoid meningitis 3 A0221 Salmonella meningitis 3 A066 Amebic brain abscess 3 A170 Tuberculous meningitis 3 A171 Meningeal tuberculoma 3 A1781 Tuberculoma of brain and spinal cord 3 A1782 Tuberculous meningoencephalitis 3 A1783 Tuberculous neuritis 3 A1789 Other tuberculosis of nervous system 3 A179 Tuberculosis of nervous system, unspecified 3 A203 Plague meningitis 3 A2781 Aseptic meningitis in leptospirosis 3 A3211 Listerial meningitis 3 A3212 Listerial meningoencephalitis 3 A34 Obstetrical tetanus 3 A35 Other tetanus 3 A390 Meningococcal meningitis 3 A3981 Meningococcal encephalitis 3 A4281 Actinomycotic meningitis 3 A4282 Actinomycotic encephalitis 3 A5040 Late congenital neurosyphilis, unspecified 3 A5041 Late congenital syphilitic meningitis 3 A5042 Late congenital syphilitic encephalitis 3 A5043 Late congenital syphilitic polyneuropathy 3 A5044 Late congenital syphilitic optic nerve atrophy 3 A5045 Juvenile general paresis 3 A5049 Other late congenital neurosyphilis 3 A5141 Secondary syphilitic meningitis 3 A5210 Symptomatic neurosyphilis, unspecified 3 A5211 Tabes dorsalis 3 A5212 Other cerebrospinal syphilis 3 A5213 Late syphilitic meningitis 3 A5214 Late syphilitic encephalitis 3 A5215 Late syphilitic neuropathy 3 A5216 Charcot's arthropathy (tabetic) 3 A5217 General paresis 3 A5219 Other symptomatic neurosyphilis 3 A522 Asymptomatic neurosyphilis 3 A523 Neurosyphilis, -

Receptores Β-Adrenérgicos No Sistema Cardiovascular
Medicina, Ribeirão Preto, X SIMPÓSIO BRASILEIRO DE FISIOLOGIA CARDIOVASCULAR 39 (1): 3-12, jan./mar. 2006 Capítulo I RECEPTORES β-ADRENÉRGICOS NO SISTEMA CARDIOVASCULAR β-ADRENOCEPTORS FUNCTION IN THE CARDIOVASCULAR SYSTEM Mário A Neto1, Ricardo R Rascado1, Lusiane M Bendhack2 1Pós-Graduandos (Doutorado). Faculdade de Medicina de Ribeirão Preto - USP. 2Docente. Departamento de Física e Química. Faculdade de Ciências Farmacêuticas de Ribeirão Preto - USP. CORRESPONDÊNCIA: Profa. Dra. Lusiane M. Bendhack. Laboratório de Farmacologia. Faculdade de Ciências Farmacêuticas de Ribeirão Preto - USP Av. do Café s/nº - 14040-903 Ribeirão Preto - SP Fax: 16-36024880 . e-mail: [email protected] Neto MA, Rascado RR, Bendhack LM. Receptores β−adrenérgicos no sistema cardiovascular. Medicina (Ribeirão Preto) 2006; 39 (1): 3-12. Resumo: Os receptores β-adrenérgicos (β-AR) integram um sistema proteico ternário: β-AR, proteína G de acoplamento e enzimas como a adenilato-ciclase (AC) que produz o 3´-5´ monofosfato de adenosina (AMPc). O principal mecanismo de ação do AMPc é a ativação da proteína quinase A (PKA), capaz de fosforilar inúmeros substratos. Em células endoteliais, a ativação dos β-AR promove o aumento dos níveis citoplasmáticos de Ca+2 favorecendo a ligação do Ca+2 com a calmodulina e deste complexo com a enzima óxido nítrico sintase endotelial (eNOS), resultando na produção de NO. A ativação β-AR no músculo liso vascular e conseqüente ativação da PKA reduz a concentração citoplasmática de Ca+2 e a sua afinidade pela calmodulina, resultando no relaxamento vascular. Os receptores β-AR podem ser agrupados em β-AR clássi- cos (β e β ) e β-AR atípicos (β e β ). -

Controlled Substance Monitoring and Drugs of Abuse Testing Local Coverage Determination
Controlled Substance Monitoring and Drugs of Abuse Testing Local Coverage Determination CPT Codes: Code Description 80305 Drug test(s), presumptive, any number of drug classes, any number of devices or procedures (eg, immunoassay); capable of being read by direct optical observation only (eg, dipsticks, cups, cards, cartridges) includes sample validation when performed, per date of service 80306 Drug test(s), presumptive, any number of drug classes, any number of devices or procedures (eg, immunoassay); read by instrument assisted direct optical observation (eg, dipsticks, cups, cards, cartridges), includes sample validation when performed, per date of service 80307 Drug test(s), presumptive, any number of drug classes, any number of devices or procedures, by instrument chemistry analyzers (eg, utilizing immunoassay [eg, eia, elisa, emit, fpia, ia, kims, ria]), chromatography (eg, gc, hplc), and mass spectrometry either with or without chromatography, (eg, dart, desi, gc-ms, gc-ms/ms, lc-ms, lc-ms/ms, ldtd, maldi, tof) includes sample validation when performed, per date of service G0480 Drug test(s), definitive, utilizing drug identification methods able to identify individual drugs and distinguish between structural isomers (but not necessarily stereoisomers), including, but not limited to gc/ms (any type, single or tandem) and lc/ms (any type, single or tandem and excluding immunoassays (e.g., ia, eia, elisa, emit, fpia) and enzymatic methods (e.g., alcohol dehydrogenase)); qualitative or quantitative, all sources(s), includes specimen -

Malta Medicines List April 08
Defined Daily Doses Pharmacological Dispensing Active Ingredients Trade Name Dosage strength Dosage form ATC Code Comments (WHO) Classification Class Glucobay 50 50mg Alpha Glucosidase Inhibitor - Blood Acarbose Tablet 300mg A10BF01 PoM Glucose Lowering Glucobay 100 100mg Medicine Rantudil® Forte 60mg Capsule hard Anti-inflammatory and Acemetacine 0.12g anti rheumatic, non M01AB11 PoM steroidal Rantudil® Retard 90mg Slow release capsule Carbonic Anhydrase Inhibitor - Acetazolamide Diamox 250mg Tablet 750mg S01EC01 PoM Antiglaucoma Preparation Parasympatho- Powder and solvent for solution for mimetic - Acetylcholine Chloride Miovisin® 10mg/ml Refer to PIL S01EB09 PoM eye irrigation Antiglaucoma Preparation Acetylcysteine 200mg/ml Concentrate for solution for Acetylcysteine 200mg/ml Refer to PIL Antidote PoM Injection injection V03AB23 Zovirax™ Suspension 200mg/5ml Oral suspension Aciclovir Medovir 200 200mg Tablet Virucid 200 Zovirax® 200mg Dispersible film-coated tablets 4g Antiviral J05AB01 PoM Zovirax® 800mg Aciclovir Medovir 800 800mg Tablet Aciclovir Virucid 800 Virucid 400 400mg Tablet Aciclovir Merck 250mg Powder for solution for inj Immunovir® Zovirax® Cream PoM PoM Numark Cold Sore Cream 5% w/w (5g/100g)Cream Refer to PIL Antiviral D06BB03 Vitasorb Cold Sore OTC Cream Medovir PoM Neotigason® 10mg Acitretin Capsule 35mg Retinoid - Antipsoriatic D05BB02 PoM Neotigason® 25mg Acrivastine Benadryl® Allergy Relief 8mg Capsule 24mg Antihistamine R06AX18 OTC Carbomix 81.3%w/w Granules for oral suspension Antidiarrhoeal and Activated Charcoal -
![Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set](https://docslib.b-cdn.net/cover/8870/ehealth-dsi-ehdsi-v2-2-2-or-ehealth-dsi-master-value-set-1028870.webp)
Ehealth DSI [Ehdsi V2.2.2-OR] Ehealth DSI – Master Value Set
MTC eHealth DSI [eHDSI v2.2.2-OR] eHealth DSI – Master Value Set Catalogue Responsible : eHDSI Solution Provider PublishDate : Wed Nov 08 16:16:10 CET 2017 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 1 of 490 MTC Table of Contents epSOSActiveIngredient 4 epSOSAdministrativeGender 148 epSOSAdverseEventType 149 epSOSAllergenNoDrugs 150 epSOSBloodGroup 155 epSOSBloodPressure 156 epSOSCodeNoMedication 157 epSOSCodeProb 158 epSOSConfidentiality 159 epSOSCountry 160 epSOSDisplayLabel 167 epSOSDocumentCode 170 epSOSDoseForm 171 epSOSHealthcareProfessionalRoles 184 epSOSIllnessesandDisorders 186 epSOSLanguage 448 epSOSMedicalDevices 458 epSOSNullFavor 461 epSOSPackage 462 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 2 of 490 MTC epSOSPersonalRelationship 464 epSOSPregnancyInformation 466 epSOSProcedures 467 epSOSReactionAllergy 470 epSOSResolutionOutcome 472 epSOSRoleClass 473 epSOSRouteofAdministration 474 epSOSSections 477 epSOSSeverity 478 epSOSSocialHistory 479 epSOSStatusCode 480 epSOSSubstitutionCode 481 epSOSTelecomAddress 482 epSOSTimingEvent 483 epSOSUnits 484 epSOSUnknownInformation 487 epSOSVaccine 488 © eHealth DSI eHDSI Solution Provider v2.2.2-OR Wed Nov 08 16:16:10 CET 2017 Page 3 of 490 MTC epSOSActiveIngredient epSOSActiveIngredient Value Set ID 1.3.6.1.4.1.12559.11.10.1.3.1.42.24 TRANSLATIONS Code System ID Code System Version Concept Code Description (FSN) 2.16.840.1.113883.6.73 2017-01 A ALIMENTARY TRACT AND METABOLISM 2.16.840.1.113883.6.73 2017-01 -
Dietary Supplements Compendium Volume 1
2015 Dietary Supplements Compendium DSC Volume 1 General Notices and Requirements USP–NF General Chapters USP–NF Dietary Supplement Monographs USP–NF Excipient Monographs FCC General Provisions FCC Monographs FCC Identity Standards FCC Appendices Reagents, Indicators, and Solutions Reference Tables DSC217M_DSCVol1_Title_2015-01_V3.indd 1 2/2/15 12:18 PM 2 Notice and Warning Concerning U.S. Patent or Trademark Rights The inclusion in the USP Dietary Supplements Compendium of a monograph on any dietary supplement in respect to which patent or trademark rights may exist shall not be deemed, and is not intended as, a grant of, or authority to exercise, any right or privilege protected by such patent or trademark. All such rights and privileges are vested in the patent or trademark owner, and no other person may exercise the same without express permission, authority, or license secured from such patent or trademark owner. Concerning Use of the USP Dietary Supplements Compendium Attention is called to the fact that USP Dietary Supplements Compendium text is fully copyrighted. Authors and others wishing to use portions of the text should request permission to do so from the Legal Department of the United States Pharmacopeial Convention. Copyright © 2015 The United States Pharmacopeial Convention ISBN: 978-1-936424-41-2 12601 Twinbrook Parkway, Rockville, MD 20852 All rights reserved. DSC Contents iii Contents USP Dietary Supplements Compendium Volume 1 Volume 2 Members . v. Preface . v Mission and Preface . 1 Dietary Supplements Admission Evaluations . 1. General Notices and Requirements . 9 USP Dietary Supplement Verification Program . .205 USP–NF General Chapters . 25 Dietary Supplements Regulatory USP–NF Dietary Supplement Monographs . -
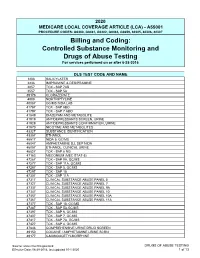
Controlled Substance Monitoring and Drugs of Abuse Testing for Services Performed on Or After 6-28-2016
2020 MEDICARE LOCAL COVERAGE ARTICLE (LCA) - A55001 PROCEDURE CODES: G0480, G0481, G0482, G0483, G0659, 80305, 80306, 80307 Billing and Coding: Controlled Substance Monitoring and Drugs of Abuse Testing For services performed on or after 6-28-2016 DLS TEST CODE AND NAME 1203 SALICYLATES 2236 IMIPRAMINE & DESIPRAMINE 2857 TOX - SAP 7AB 3557 TOX - SAP 5A 39176 CLORAZEPATE 4008 NORTRIPTYLINE 40087 GC/MS NIDA LAB 41787 TOX - SAP 6BO 41797 TOX - SAP 7 ABO 41849 DIAZEPAM AND METABOLITE 41919 ANTIDEPRESSANTS SCREEN, URINE 41929 ANTIDEPRESSANTS CONFIRMATION, URINE 41970 NICOTINE AND METABOLITES 43327 SUBSTANCE IDENTIFICATION 43357 ETHANOL 45517 NIDA 5, GC/MS 46047 AMPHETAMINE D,L SEP NIDA 46057 ETHANOL, CLINICAL URINE 46827 TOX - SAP 6 NG 47163 MECONIUM (MEC STAT-5) 47267 TOX - SAP 9A, GC/MS 47277 TOX - SAP 11A, GC/MS 47287 TOX - SAP 5, GC/MS 47297 TOX - SAP 10 47307 TOX - SAP 11A 47317 CLINICAL SUBSTANCE ABUSE PANEL 5 47327 CLINICAL SUBSTANCE ABUSE PANEL 7 47337 CLINICAL SUBSTANCE ABUSE PANEL 9A 47347 CLINICAL SUBSTANCE ABUSE PANEL 10 47357 CLINICAL SUBSTANCE ABUSE PANEL 10A 47367 CLINICAL SUBSTANCE ABUSE PANEL 11A 47377 TOX - SAP 10, GC/MS 47387 TOX - SAP 5A,GC/MS 47397 TOX - SAP 6, GC/MS 47407 TOX - SAP 7, GC/MS 47417 TOX - SAP 7A, GC/MS 47427 TOX - SAP 4, GC/MS 47846 COMPREHENSIVE URINE DRUG SCREEN 49150 COCAINE / AMPHETAMINE URINE SCRN 49177 6-MONOACETYLMORPHINE Source: www.cms.hhs.gov/mcd DRUGS OF ABUSE TESTING Effective Date: 06-28-2016, last updated 10-1-2020 1 of 13 49237 AMPHETAMINES, CLINICAL UR 49247 BARBITURATES, CLINICAL URINE 49257 -

Therapeutic Options to Minimize Allogeneic Blood
Santos AA, etREVIEW al. - Therapeutic ARTICLE options to minimize allogeneic blood Rev Bras Cir Cardiovasc 2014;29(4):606-21 transfusions and their adverse effects in cardiac surgery: A systematic review Therapeutic options to minimize allogeneic blood transfusions and their adverse effects in cardiac surgery: A systematic review Opções terapêuticas para minimizar transfusões de sangue alogênico e seus efeitos adversos em cirurgia cardíaca: Revisão sistemática Antônio Alceu dos Santos1, MD; José Pedro da Silva1, MD, PhD; Luciana da Fonseca da Silva1, MD, PhD; Alexandre Gonçalves de Sousa1, MD; Raquel Ferrari Piotto1, MD, PhD; José Francisco Baumgratz1, MD DOI: 10.5935/1678-9741.20140114 RBCCV 44205-1596 Abstract Results: Treating anemia and thrombocytopenia, suspending Introduction: Allogeneic blood is an exhaustible therapeutic anticoagulants and antiplatelet agents, reducing routine phle- resource. New evidence indicates that blood consumption is ex- botomies, utilizing less traumatic surgical techniques with moderate cessive and that donations have decreased, resulting in reduced hypothermia and hypotension, meticulous hemostasis, use of topical blood supplies worldwide. Blood transfusions are associated and systemic hemostatic agents, acute normovolemic hemodilu- with increased morbidity and mortality, as well as higher hos- tion, cell salvage, anemia tolerance (supplementary oxygen and pital costs. This makes it necessary to seek out new treatment normothermia), as well as various other therapeutic options have options. Such options -

UWA Research Publication
UWA Research Publication Price, S., Holman, D. A., Sanfilippo, F., & Emery, J. (2013). Use of case–time–control design in pharmacovigilance applications: exploration with high-risk medications and unplanned hospital admissions in the Western Australian elderly. Pharmacoepidemiology and Drug Safety, 22(11), 1159-1170. Copyright © 2013 John Wiley & Sons, Ltd. This is the peer reviewed version of the following article: Price, S., Holman, D. A., Sanfilippo, F., & Emery, J. (2013). Use of case–time–control design in pharmacovigilance applications: exploration with high-risk medications and unplanned hospital admissions in the Western Australian elderly. Pharmacoepidemiology and Drug Safety, 22(11), 1159-1170., which has been published in final form at http://dx.doi.org/10.1002/pds.3469. This article may be used for non-commercial purposes in accordance With Wiley Terms and Conditions for self-archiving' This version was made available in the UWA Research Repository on 23 April 2015 in compliance with the publisher’s policies on archiving in institutional repositories. Use of the article is subject to copyright law. Use of case-time-control design in pharmacovigilance applications: exploration with high risk medications and unplanned hospital admissions in the Western Australian elderly Running head: High risk drugs and hospital admissions in elderly Sylvie D Price1, C D’Arcy J Holman1, Frank M Sanfilippo1 and Jon D Emery2 1 School of Population Health, The University of Western Australia, Perth, Australia 2 School of Primary, Aboriginal and Rural Health Care, The University of Western Australia, Perth, Australia Corresponding author: Sylvie Price, School of Population Health (M431), The University of Western Australia, 35 Stirling Highway, CRAWLEY WA 6009, Australia; Tel.