Letters to the Editor
Total Page:16
File Type:pdf, Size:1020Kb
Load more
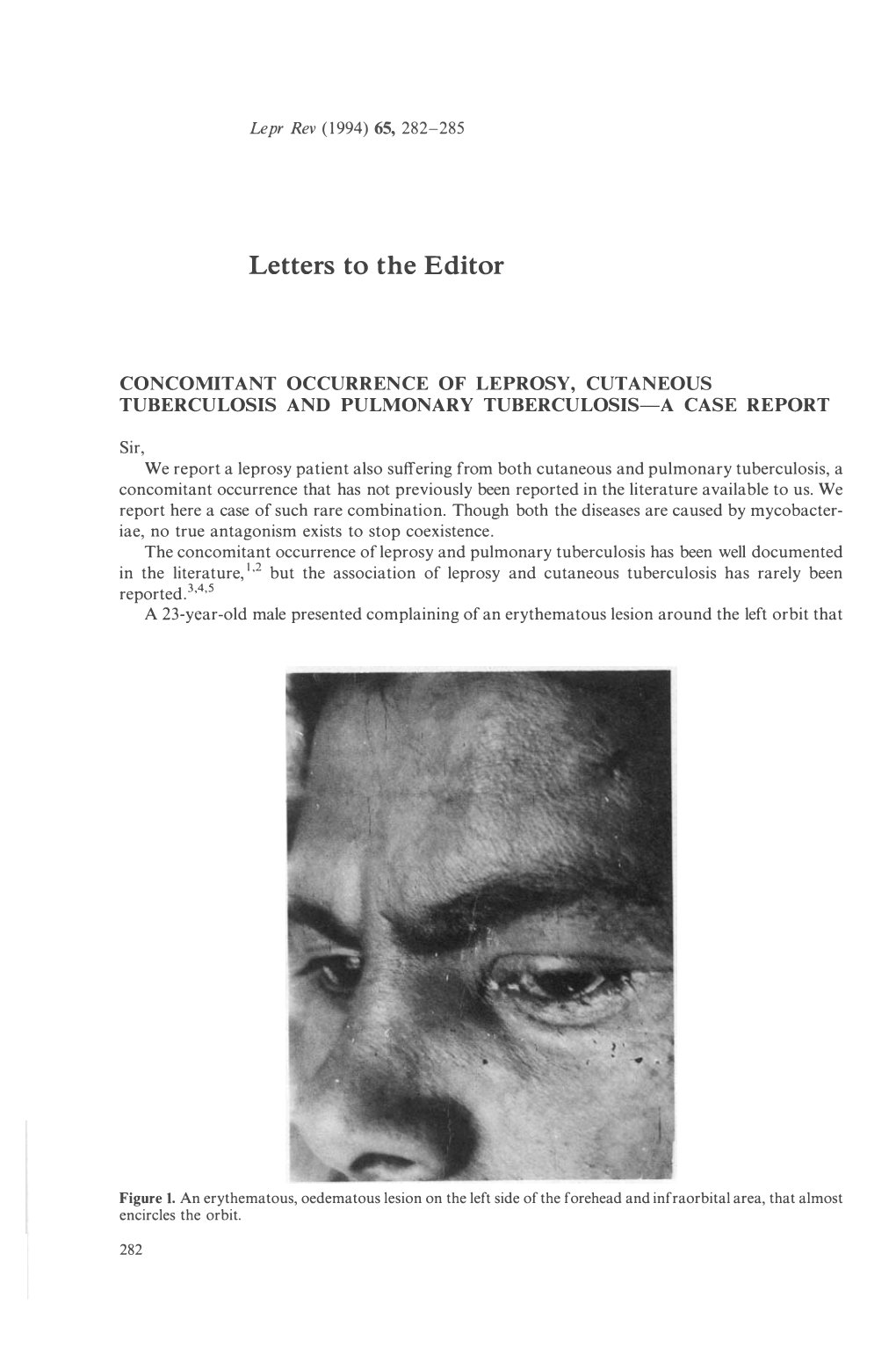
Recommended publications
-

Chapter 3 Bacterial and Viral Infections
GBB03 10/4/06 12:20 PM Page 19 Chapter 3 Bacterial and viral infections A mighty creature is the germ gain entry into the skin via minor abrasions, or fis- Though smaller than the pachyderm sures between the toes associated with tinea pedis, His customary dwelling place and leg ulcers provide a portal of entry in many Is deep within the human race cases. A frequent predisposing factor is oedema of His childish pride he often pleases the legs, and cellulitis is a common condition in By giving people strange diseases elderly people, who often suffer from leg oedema Do you, my poppet, feel infirm? of cardiac, venous or lymphatic origin. You probably contain a germ The affected area becomes red, hot and swollen (Ogden Nash, The Germ) (Fig. 3.1), and blister formation and areas of skin necrosis may occur. The patient is pyrexial and feels unwell. Rigors may occur and, in elderly Bacterial infections people, a toxic confusional state. In presumed streptococcal cellulitis, penicillin is Streptococcal infection the treatment of choice, initially given as ben- zylpenicillin intravenously. If the leg is affected, Cellulitis bed rest is an important aspect of treatment. Where Cellulitis is a bacterial infection of subcutaneous there is extensive tissue necrosis, surgical debride- tissues that, in immunologically normal individu- ment may be necessary. als, is usually caused by Streptococcus pyogenes. A particularly severe, deep form of cellulitis, in- ‘Erysipelas’ is a term applied to superficial volving fascia and muscles, is known as ‘necrotiz- streptococcal cellulitis that has a well-demarcated ing fasciitis’. This disorder achieved notoriety a few edge. -

Pattern of Cutaneous Tuberculosis Among Children and Adolescent
Bangladesh Med Res Counc Bull 2012; 38: 94-97 Pattern of cutaneous tuberculosis among children and adolescent Sultana A1, Bhuiyan MSI1, Haque A2, Bashar A3, Islam MT4, Rahman MM5 1Dept. of Dermatology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, 2Dept. of Public health and informatics, BSMMU, Dhaka, 3SK Hospital, Mymensingh Medical College, Mymensingh, 4Dept. of Physical Medicine and Rehabilitation, BSMMU, Dhaka, 5Dept. of Dermatology, National Medical College, Dhaka. Email: [email protected] Abstract Cutaneous tuberculosis is one of the most subtle and difficult diagnoses for dermatologists practicing in developing countries. It has widely varied manifestations and it is important to know the spectrum of manifestations in children and adolescent. Sixty cases (age<19 years) of cutaneous tuberculosis were included in this one period study. The diagnosis was based on clinical examination, tuberculin reaction, histopathology, and response to antitubercular therapy. Histopahology revealed 38.3% had skin tuberculosis and 61.7% had diseases other than tuberculosis. Among 23 histopathologically proved cutaneous tuberculosis, 47.8% had scrofuloderma, 34.8% had lupus vulgaris and 17.4% had tuberculosis verrucosa cutis (TVC). Most common site for scrofuloderma lesions was neck and that for lupus vulgaris and TVC was lower limb. Cutaneous tuberculosis in children continues to be an important cause of morbidity, there is a high likelihood of internal involvement, especially in patients with scrofuloderma. A search is required for more sensitive, economic diagnostic tools. Introduction of Child Health (BICH) and Institute of Diseases of Tuberculosis (TB), an ancient disease has affected Chest and Hospital (IDCH) from January to humankind for more than 4,000 years1 and its December 2010. -

A Rare Case of Tuberculosis Cutis Colliquative
Jemds.com Case Report A Rare Case of Tuberculosis Cutis Colliquative 1 2 3 4 5 Shravya Rimmalapudi , Amruta D. Morey , Bhushan Madke , Adarsh Lata Singh , Sugat Jawade 1, 2, 3, 4, 5 Department of Dermatology, Venereology and Leprosy, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, Maharashtra, India. INTRODUCTION Tuberculosis is one of the oldest documented diseases known to mankind and has Corresponding Author: evolved along with humans for several million years. It is still a major burden globally Dr. Bhushan Madke, despite the advancement in control measures and reduction in new cases1 Professor and Head, Tuberculosis is a chronic granulomatous infectious disease. It is caused by Department of Dermatology, Venereology & Leprosy, Mycobacterium tuberculosis, an acid-fast bacillus with inhalation of airborne droplets Jawaharlal Nehru Medical College, 2,3 being the route of spread. The organs most commonly affected include lungs, Datta Meghe Institute of Medical intestines, lymph nodes, skin, meninges, liver, oral cavity, kidneys and bones.1 About Sciences, Wardha, Maharashtra, India. 1.5 % of tuberculous manifestations are cutaneous and accounts for 0.1 – 0.9 % of E-mail: [email protected] total dermatological out patients in India.2 Scrofuloderma is a type of cutaneous tuberculosis (TB) which is a rare presentation in dermatological setting and is DOI: 10.14260/jemds/2021/67 difficult to diagnose. It was earlier known as tuberculosis cutis colliquative develops as an extension of infection into the skin from an underlying focus, usually the lymph How to Cite This Article: Rimmalapudi S, Morey AD, Madke B, et al. A nodes and sometimes bone. -

Tuberculosis Verrucosa Cutis Presenting As an Annular Hyperkeratotic Plaque
CONTINUING MEDICAL EDUCATION Tuberculosis Verrucosa Cutis Presenting as an Annular Hyperkeratotic Plaque Shahbaz A. Janjua, MD; Amor Khachemoune, MD, CWS; Sabrina Guillen, MD GOAL To understand cutaneous tuberculosis to better manage patients with the condition OBJECTIVES Upon completion of this activity, dermatologists and general practitioners should be able to: 1. Recognize the morphologic features of cutaneous tuberculosis. 2. Describe the histopathologic characteristics of cutaneous tuberculosis. 3. Explain the treatment options for cutaneous tuberculosis. CME Test on page 320. This article has been peer reviewed and approved Einstein College of Medicine is accredited by by Michael Fisher, MD, Professor of Medicine, the ACCME to provide continuing medical edu- Albert Einstein College of Medicine. Review date: cation for physicians. October 2006. Albert Einstein College of Medicine designates This activity has been planned and imple- this educational activity for a maximum of 1 AMA mented in accordance with the Essential Areas PRA Category 1 CreditTM. Physicians should only and Policies of the Accreditation Council for claim credit commensurate with the extent of their Continuing Medical Education through the participation in the activity. joint sponsorship of Albert Einstein College of This activity has been planned and produced in Medicine and Quadrant HealthCom, Inc. Albert accordance with ACCME Essentials. Drs. Janjua, Khachemoune, and Guillen report no conflict of interest. The authors discuss off-label use of ethambutol, isoniazid, pyrazinamide, and rifampicin. Dr. Fisher reports no conflict of interest. Tuberculosis verrucosa cutis (TVC) is a form evolving cell-mediated immunity. TVC usually of cutaneous tuberculosis that results from acci- begins as a solitary papulonodule following a dental inoculation of Mycobacterium tuberculosis trivial injury or trauma on one of the extremi- in a previously infected or sensitized individ- ties that soon acquires a scaly and verrucous ual with a moderate to high degree of slowly surface. -

Lupus Vulgaris Developing at the Site of Scrofuloderma Misdiagnosed As Leishmania
INFECTIOUS DISEASES (BACTERIAL, FUNGAL, VIRAL, PARASITIC, INFESTATIONS) LUPUS VULGARIS DEVELOPING AT THE SITE OF SCROFULODERMA MISDIAGNOSED AS LEISHMANIA R Sanchez-perales (1) - E Saenz-anduaga (1) - G Chanco-ramirez (1) - M Sialer-vildozola (1) - L Cevallos-riva (1) Hospital Militar Central, Dermatology, Lima, Peru (1) Background: Tuberculosis is a chronic infectious disease caused by Mycobacterium tuberculosis, that mostly affects the lungs. In 2017, about 10 million people worldwide developed some form of tuberculosis. Extrapulmonary tuberculosis represents 10-20% of all types of tuberculosis, and 1.5% of these cases are cutaneous tuberculosis. The most frequent clinical manifestations of cutaneous tuberculosis are scrofuloderma and lupus vulgaris. The clinical and histopathological forms of cutaneous tuberculosis may resemble other infectious diseases. Observation: A 19-year-old Peruvian man presented with an erythematous plaque in the left inguinal area with no other constitutional symptoms. Initially, the lesion was an erythematous, suppurative nodule which over the course of six months grew into a 6 by 7 cm plaque with defined edges, irregular shape, shiny surface, and light desquamation. This lesion was overlying a 1 cm mobile, painful adenopathy. The histopathological study of the skin lesion showed a severe lymphocytic inflammatory infiltrate, with the presence of granulomas and giant multinucleated Langhans cells. The PAS, Giemsa, Grocott and Ziehl- Neelsen stains were negative for microorganisms. Patient´s chest X-ray and acid-fast bacilli stain in sputum were negative. It was not possible to perform PPD testing. Skin biopsy PCR tested positive for Leishmania, which lead the physicians to treat the patient with sodium stibogluconate. The lesion partially improved, but subsequently got worse. -

Scrofuloderma: a Rare Case Report on Cutaneous Tuberculosis Taksande Amar, MD, FIAE1*, Zeeshan Patel, MBBS2 and Meshram Rewat, MD3
ISSN: 2378-3656 Amar et al. Clin Med Rev Case Rep 2020, 7:330 DOI: 10.23937/2378-3656/1410330 Volume 7 | Issue 12 Clinical Medical Reviews Open Access and Case Reports CASE REPORT Scrofuloderma: A Rare Case Report on Cutaneous Tuberculosis Taksande Amar, MD, FIAE1*, Zeeshan Patel, MBBS2 and Meshram Rewat, MD3 1Professor, Department of Paediatrics, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, India 2 Resident, Department of Paediatrics, Jawaharlal Nehru Medical College, Datta Meghe Institute of Check for Medical Sciences, India updates 3Associate Professor, Department of Paediatrics, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, India *Corresponding author: Dr. Amar Taksande, Department of Paediatrics, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi Meghe, Wardha, Maharashtra State 442004, India nodes are most often involved followed by axillary, in- Abstract guinal group of lymph nodes [2]. Scrofuloderma begins Globally, India has one of the highest burdens of tuber- as firm, deep seated nodule adherent to skin followed culosis (TB). The diagnosis of tuberculosis is challenging, particularly in young children due to a high rate of extra-pul- by softening, suppuration, perforation and then, lastly monary and meningeal disease. Scrofuloderma is cuta- formsan ulcer or sinus. Later on, a scarred tract devel- neous tuberculosis, accounting for approximately 1.5% of ops and bridges the ulcerative areas [2,3]. Here we re- extra-pulmonary cases. Mycobacterium tuberculosis is the port a rare case of scrofuloderma in pediatric patient. main etiological agent and, rarely, by Mycobacterium bo- vis. The cutaneous variants of tuberculosis have a variable Case Report clinical appearance, significance and prognosis. -

A Rare Case of Coexistence of Borderline Lepromatous Leprosy with Tuberculosis Verrucosa Cutis
Hindawi Publishing Corporation Case Reports in Infectious Diseases Volume 2016, Article ID 1746896, 4 pages http://dx.doi.org/10.1155/2016/1746896 Case Report A Rare Case of Coexistence of Borderline Lepromatous Leprosy with Tuberculosis Verrucosa Cutis Biswajit Dey,1 Debasis Gochhait,1 Nagendran Prabhakaran,2 Laxmisha Chandrashekar,2 and Biswanath Behera2 1 Department of Pathology, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry, India 2Department of Dermatology, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Pondicherry, India Correspondence should be addressed to Debasis Gochhait; [email protected] Received 13 July 2016; Revised 23 October 2016; Accepted 31 October 2016 Academic Editor: Sinesio´ Talhari Copyright © 2016 Biswajit Dey et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Occurrence of pulmonary tuberculosis with leprosy is known but association of cutaneous tuberculosis with leprosy is rare. We report a case of borderline lepromatous leprosy coexistent with tuberculosis verrucosa cutis in a 29-year-old male, who presented with multiple skin coloured nodules and hyperkeratotic scaly lesions of 3-month duration. Dual infections are associated with high mortality and morbidity. Therefore early diagnosis and management helps to reduce mortality and to mitigate the effects of morbidity. 1. Introduction or motor weakness. The patient denied any drug intake, fever, myalgia, spontaneous blistering or ulceration, neuritic Mycobacterium leprae is the causative agent of leprosy that pain, and testicular pain. None of the family members or affects the skin and peripheral nerves. -

Unusual Presentation of Scrofuloderma in an Immunocompetent Patient
LETTER TO THE EDITOR Unusual Presentation of Scrofuloderma in an Immunocompetent Patient Sir, Figure 1a: Left cheek; showing Figure 1b: Complete regression of Cutaneous tuberculosis has many faces; from papules and nodules coalescing to lesions after treatment. form a plaque. paucibacillary tuberculosis verrucosa cutis to multibacillary acute miliary tuberculosis.1 Scrofuloderma also called as tuberculosis colliquativa cutis is the second most common type of cutaneous tuberculosis following lupus vulgaris.2 It is characterized by a bluish- red nodule overlying an infected lymph gland, bone or joint that breaks down to form an undermined ulcer with a granulating tissue at the base.3 Unusual site and atypical morphological appearance can confuse this Figure 2a: Showing epithelioid Figure 2b: Showing atrophied entity with other clinically mimicking conditions. granuloma containing langerhans epidermis, epithelioid granuloma giant cells surrounded by lympho- containing langerhans giant cells A twenty eight-years old, otherwise, healthy male, cytes (H and E; x10). (H and E; x40). presented with multiple erythematous papules and nodules on his left cheek persisting for the last 8 months. In the present case, morphology of plaque and site There was history of on and off seropurulent discharge. involved suggested cervico facial actinomycoses as first There was no history of similar complaints in the clinical possibility. The absence of sulphur granules and family or contact with tubercular patient. There was negative culture report for actinomycetes helped us to no history of past treatment for these complaints. delineate this condition. Nocardiosis was also ruled out Cutaneous examination revealed seven ill to well on the basis of absence of gram-positive branched- defined papules and nodules coalesced to form a plaque filaments. -

Picture of the Month—Diagnosis
Denouement and Discussion Scrofuloderma With Lupus Vulgaris he result of tuberculin skin testing was positive, with vised National Tuberculosis Control Programme, the di- a20ϫ25-mmindurationassociatedwithvesiculation. rectly observed short-course chemotherapy strategy (DOTS), Thesputumexaminationresultforacid-fastbacilliwas a globally accepted standard for treatment of all forms of tu- T 13 negative. Pus aspirated from the cold abscess, and a smear from berculosis, is followed. In the initial intensive phase of treat- the ulcers did not reveal any mycobacteria on Ziehl-Neelsen ment, isoniazid, 10 to 15 mg/kg; rifampicin, 10 mg/kg; pyra- acid-fast stain; however, a biopsy specimen from the skin le- zinamide, 15 to 30 mg/kg; and ethambutol, 15 to 25 mg/kg, sion and sinuses revealed tuberculous granulomatous infec- are given 3 times a week on alternate days for 2 months, while tion. Routine culture eventually grew Mycobacterium tubercu- in the immediate continuation phase, isoniazid and rifam- losis, and the patient was diagnosed as having scrofuloderma picin are given in the same doses 3 times a week for 4 months. (SCD) and lupus vulgaris (cutaneous tuberculosis). He re- DOTS has the advantage of directly supervised treatment that sponded well to drainage of cold abscesses and standard an- increases the cure rate, decreases transmission of disease, and tituberculous drug therapy, composed of isoniazid, rifampi- prevents emergence of multidrug-resistant tuberculosis while cin sodium, pyrazinamide, and ethambutol hydrochloride. minimizing adverse effects due to drugs. In SCD resulting The incidence of cutaneous tuberculosis, which forms a from tuberculous lymphadenitis, arthritis, or osteomyelitis, minute proportion of extrapulmonary tuberculosis, has de- surgery in the form of aspiration, incision and drainage, de- creased from 2% to 0.15% in India.1 In the West, it is rarely en- bridement, curettage, and partial or total excision of the cold countered. -

Recurrent Abscesses of the Neck: Scrofuloderma Tuberculosis of the Skin Has Become a Rare Disease in Indus- Trialized Countries
Letters 1. McKenzie WS, Rosenberg M. Iatrogenic subcutaneous emphysema of dental and surgical origin: a literature review. J Oral Maxillofac Surg. 2009;67(6): Figure 1. Clinical Images of the Patient 1265-1268. A 2. Romeo U, Galanakis A, Lerario F, Daniele GM, Tenore G, Palaia G. Subcutaneous emphysema during third molar surgery: a case report. Braz Dent J. 2011;22(1):83-86. 3. Arai I, Aoki T, Yamazaki H, Ota Y, Kaneko A. Pneumomediastinum and subcutaneous emphysema after dental extraction detected incidentally by regular medical checkup: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(4):e33-e38. 4. Sujeet K, Shankar S. Images in clinical medicine: prevertebral emphysema after a dental procedure. N Engl J Med. 2007;356(2):173. 5. Hsu HL, Chang CC, Liu KL. Subcutaneous emphysema after dental procedure. QJM. 2011;104(6):545. Recurrent Abscesses of the Neck: Scrofuloderma Tuberculosis of the skin has become a rare disease in indus- trialized countries. Polymerase chain reaction (PCR) is a pow- erful diagnostic tool for mycobacterial infections of the skin, but it can fail, as demonstrated in this case. Report of a Case | A woman in her 80s was referred for surgical B treatment of a cervical abscess. Similar abscesses erupted in the cervical region over the course of 2 years (Figure 1A). A needle aspiration biopsy was performed on a node at the left side of the neck, which measured 2 cm. The histopatho- logic report described a minor nonspecific inflammatory reaction, not suggestive of infection. Findings of the Myco- bacterium tuberculosis PCR were negative. -

Original Article Cutaneous Manifestations of Extra Pulmonary
Original Article Cutaneous Manifestations of Extra pulmonary Tuberculosis Ahmad S1, Ahmed N2, Singha JL3, Mamun MAA4, Hassan ASMFU5, Aziz NMSB6, Alam SI7 Conflict of Interest: None Abstract: Received: 12-08-2018 Background: Ulcers and surgical wounds not healing well and expectedly are common problems Accepted: 06-11-2018 www.banglajol.info/index.php/JSSMC among patients in countries like us. Ulcers may develop spontaneously or following a penetrating injury. wounds not healing well are common among poor, lower middle class and middle class people. Postsurgical non-healing wound or chronic discharging sinuses at the scar site are also common in that class of people. Suspecting malignancy or tuberculosis in these types of wounds we have sent wedge or excision biopsy for these ulcers in about 500 cases and found tuberculosis in 65 cases. In rest of the cases histopathology reports found as non- specific ulcers, Malignant melanoma, squamous or basal cell carcinoma, Verruca vulgaris. Objectives: To find out the relationship of tuberculosis with chronic or nonhealing ulcers. Methods: This is a prospective observational study conducted for patients coming to our chambers, OPD of a district general hospital and Shaheed Suhrawardy Medical College Hospital, Dhaka from July 2012 to June 2018. Results: Mean age of the study subjects were 28±2. Among the study subjects nonspecific ulcer or sinus tracts were found in 418 (83.6%), tuberculosis in 65 (13%), Malignant melanoma 7 (1.4%), Verruca vulgaris 5(1%), squamous cell carcinoma 3(0.6), basal cell carcinoma 2 (0.4%). Biopsy done only for very suspicious ulcers or wounds. Key Words: Cutaneous Conclusion: With this very small sample size it is difficult to conclude regarding incidence of manifestation, Extrapulmonary cutaneous involvement of extra pulmonary tuberculosis , but every clinician should think of it in case involvement, Tuberculosis. -
![Culture Negative Cutaneous Tuberculosis[Version 1; Peer Review: 1 Approved with Reservations, 1 Not Approved]](https://docslib.b-cdn.net/cover/0061/culture-negative-cutaneous-tuberculosis-version-1-peer-review-1-approved-with-reservations-1-not-approved-3790061.webp)
Culture Negative Cutaneous Tuberculosis[Version 1; Peer Review: 1 Approved with Reservations, 1 Not Approved]
F1000Research 2019, 8:509 Last updated: 05 AUG 2021 CASE REPORT Case Report: Culture negative cutaneous tuberculosis [version 1; peer review: 1 approved with reservations, 1 not approved] Maria Qadri, Qurban Hussain Sheikh, Mir Tahir Hussain Talpur, Uzair Yaqoob , Khalil Ullah Shabbir Department of Medicine, Jinnah Postgraduate Medical Centre, Karachi, Sindh, Pakistan v1 First published: 17 Apr 2019, 8:509 Open Peer Review https://doi.org/10.12688/f1000research.18850.1 Latest published: 17 Apr 2019, 8:509 https://doi.org/10.12688/f1000research.18850.1 Reviewer Status Invited Reviewers Abstract Cutaneous tuberculosis (TB) can present in a number of ways, making 1 2 it difficult to diagnose. It most commonly presents as scrofuloderma, which commonly affects the supra-clavicular region, axilla and the version 1 cervical region. All the different presentations of cutaneous TB should 17 Apr 2019 report report be known to clinicians, in order to diagnose it early. The objective of this article is to describe a case of scrofuloderma presenting with 1. Vanessa Lucília Silveira de Medeiros , different cutaneous lesions at the same time, which were culture negative. We present a 23-year-old male with no known co- Federal University of Pernambuco (UFPE), morbidities, presenting to us with fever and multiple swellings on the Recife, Brazil body. Cultures of pus and blood were negative for TB; GeneXpert detected the microorganism. Cutaneous TB, although a rare disease 2. Rita V. Vora, Shree Krishna Hospital, with wide spectrum of cutaneous lesions, should be considered in Karamsad, India differential diagnosis of cold abscesses and nodules, especially of the head and neck region.