Clobetasone Butyrate Eye Drops Effect on Ocular Inflammation and Intraocular Pressure
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

This Fact Sheet Provides Information to Patients with Eczema and Their Carers. About Topical Corticosteroids How to Apply Topic
This fact sheet provides information to patients with eczema and their carers. About topical corticosteroids You or your child’s doctor has prescribed a topical corticosteroid for the treatment of eczema. For treating eczema, corticosteroids are usually prepared in a cream or ointment and are applied topically (directly onto the skin). Topical corticosteroids work by reducing inflammation and helping to control an over-reactive response of the immune system at the site of eczema. They also tighten blood vessels, making less blood flow to the surface of the skin. Together, these effects help to manage the symptoms of eczema. There is a range of steroids that can be used to treat eczema, each with different strengths (potencies). On the next page, the potencies of some common steroids are shown, as well as the concentration that they are usually used in cream or ointment preparations. Using a moisturiser along with a steroid cream does not reduce the effect of the steroid. There are many misconceptions about the side effects of topical corticosteroids. However these treatments are very safe and patients are encouraged to follow the treatment regimen as advised by their doctor. How to apply topical corticosteroids How often should I apply? How much should I apply? Apply 1–2 times each day to the affected area Enough cream should be used so that the of skin according to your doctor’s instructions. entire affected area is covered. The cream can then be rubbed or massaged into the Once the steroid cream has been applied, inflamed skin. moisturisers can be used straight away if needed. -

(12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 De Juan Et Al
US 200601 10428A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 de Juan et al. (43) Pub. Date: May 25, 2006 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA (US); A6F 2/00 (2006.01) Signe E. Varner, Los Angeles, CA (52) U.S. Cl. .............................................................. 424/427 (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Correspondence Address: Featured is a method for instilling one or more bioactive SCOTT PRIBNOW agents into ocular tissue within an eye of a patient for the Kagan Binder, PLLC treatment of an ocular condition, the method comprising Suite 200 concurrently using at least two of the following bioactive 221 Main Street North agent delivery methods (A)-(C): Stillwater, MN 55082 (US) (A) implanting a Sustained release delivery device com (21) Appl. No.: 11/175,850 prising one or more bioactive agents in a posterior region of the eye so that it delivers the one or more (22) Filed: Jul. 5, 2005 bioactive agents into the vitreous humor of the eye; (B) instilling (e.g., injecting or implanting) one or more Related U.S. Application Data bioactive agents Subretinally; and (60) Provisional application No. 60/585,236, filed on Jul. (C) instilling (e.g., injecting or delivering by ocular ion 2, 2004. Provisional application No. 60/669,701, filed tophoresis) one or more bioactive agents into the Vit on Apr. 8, 2005. reous humor of the eye. Patent Application Publication May 25, 2006 Sheet 1 of 22 US 2006/0110428A1 R 2 2 C.6 Fig. -

A New Robust Technique for Testing of Glucocorticosteroids in Dogs and Horses Terry E
Iowa State University Capstones, Theses and Retrospective Theses and Dissertations Dissertations 2007 A new robust technique for testing of glucocorticosteroids in dogs and horses Terry E. Webster Iowa State University Follow this and additional works at: https://lib.dr.iastate.edu/rtd Part of the Veterinary Toxicology and Pharmacology Commons Recommended Citation Webster, Terry E., "A new robust technique for testing of glucocorticosteroids in dogs and horses" (2007). Retrospective Theses and Dissertations. 15029. https://lib.dr.iastate.edu/rtd/15029 This Thesis is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Retrospective Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. A new robust technique for testing of glucocorticosteroids in dogs and horses by Terry E. Webster A thesis submitted to the graduate faculty in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE Major: Toxicology Program o f Study Committee: Walter G. Hyde, Major Professor Steve Ensley Thomas Isenhart Iowa State University Ames, Iowa 2007 Copyright © Terry Edward Webster, 2007. All rights reserved UMI Number: 1446027 Copyright 2007 by Webster, Terry E. All rights reserved. UMI Microform 1446027 Copyright 2007 by ProQuest Information and Learning Company. All rights reserved. This microform edition is protected against unauthorized copying under Title 17, United States Code. ProQuest Information and Learning Company 300 North Zeeb Road P.O. Box 1346 Ann Arbor, MI 48106-1346 ii DEDICATION I want to dedicate this project to my wife, Jackie, and my children, Shauna, Luke and Jake for their patience and understanding without which this project would not have been possible. -

(12) United States Patent (10) Patent No.: US 6,264,917 B1 Klaveness Et Al
USOO6264,917B1 (12) United States Patent (10) Patent No.: US 6,264,917 B1 Klaveness et al. (45) Date of Patent: Jul. 24, 2001 (54) TARGETED ULTRASOUND CONTRAST 5,733,572 3/1998 Unger et al.. AGENTS 5,780,010 7/1998 Lanza et al. 5,846,517 12/1998 Unger .................................. 424/9.52 (75) Inventors: Jo Klaveness; Pál Rongved; Dagfinn 5,849,727 12/1998 Porter et al. ......................... 514/156 Lovhaug, all of Oslo (NO) 5,910,300 6/1999 Tournier et al. .................... 424/9.34 FOREIGN PATENT DOCUMENTS (73) Assignee: Nycomed Imaging AS, Oslo (NO) 2 145 SOS 4/1994 (CA). (*) Notice: Subject to any disclaimer, the term of this 19 626 530 1/1998 (DE). patent is extended or adjusted under 35 O 727 225 8/1996 (EP). U.S.C. 154(b) by 0 days. WO91/15244 10/1991 (WO). WO 93/20802 10/1993 (WO). WO 94/07539 4/1994 (WO). (21) Appl. No.: 08/958,993 WO 94/28873 12/1994 (WO). WO 94/28874 12/1994 (WO). (22) Filed: Oct. 28, 1997 WO95/03356 2/1995 (WO). WO95/03357 2/1995 (WO). Related U.S. Application Data WO95/07072 3/1995 (WO). (60) Provisional application No. 60/049.264, filed on Jun. 7, WO95/15118 6/1995 (WO). 1997, provisional application No. 60/049,265, filed on Jun. WO 96/39149 12/1996 (WO). 7, 1997, and provisional application No. 60/049.268, filed WO 96/40277 12/1996 (WO). on Jun. 7, 1997. WO 96/40285 12/1996 (WO). (30) Foreign Application Priority Data WO 96/41647 12/1996 (WO). -

St John's Institute of Dermatology
St John’s Institute of Dermatology Topical steroids This leaflet explains more about topical steroids and how they are used to treat a variety of skin conditions. If you have any questions or concerns, please speak to a doctor or nurse caring for you. What are topical corticosteroids and how do they work? Topical corticosteroids are steroids that are applied onto the skin and are used to treat a variety of skin conditions. The type of steroid found in these medicines is similar to those produced naturally in the body and they work by reducing inflammation within the skin, making it less red and itchy. What are the different strengths of topical corticosteroids? Topical steroids come in a number of different strengths. It is therefore very important that you follow the advice of your doctor or specialist nurse and apply the correct strength of steroid to a given area of the body. The strengths of the most commonly prescribed topical steroids in the UK are listed in the table below. Table 1 - strengths of commonly prescribed topical steroids Strength Chemical name Common trade names Mild Hydrocortisone 0.5%, 1.0%, 2.5% Hydrocortisone Dioderm®, Efcortelan®, Mildison® Moderate Betamethasone valerate 0.025% Betnovate-RD® Clobetasone butyrate 0.05% Eumovate®, Clobavate® Fluocinolone acetonide 0.001% Synalar 1 in 4 dilution® Fluocortolone 0.25% Ultralanum Plain® Fludroxycortide 0.0125% Haelan® Tape Strong Betamethasone valerate 0.1% Betnovate® Diflucortolone valerate 0.1% Nerisone® Fluocinolone acetonide 0.025% Synalar® Fluticasone propionate 0.05% Cutivate® Hydrocortisone butyrate 0.1% Locoid® Mometasone furoate 0.1% Elocon® Very strong Clobetasol propionate 0.1% Dermovate®, Clarelux® Diflucortolone valerate 0.3% Nerisone Forte® 1 of 5 In adults, stronger steroids are generally used on the body and mild or moderate steroids are used on the face and skin folds (armpits, breast folds, groin and genitals). -

Clobetasone Butyrate, a New Topical Corticosteroid: Clinical Activity and Effects on Pituitary-Adrenal Axis Function and Model of Epidermal Atrophy
626 BRITISH MEDICAL JOURNAL 13 SEPTEMBER 1975 17 Anderson, J. R., Goudie, R. B., and Gray, K. G., British J7ournal of 21 Temple, R., et al., Mayo Clinic Proceedings, 1972, 47, 872. Experimental Pathology, 1960, 41, 364. 22 Carlson, H. E., Temple, R., and Robbins, J., Journal of Clinical Endo- Br Med J: first published as 10.1136/bmj.3.5984.626 on 13 September 1975. Downloaded from 18 Fulthorpe, A. J., et al., Journal of Clinical Pathology, 1961, 14 654. crinology and Metabolism, 1973, 36, 1251. 19 Holborow, E. J., et al., British J7ournal of Experimental Pathology, 1959, '3 Cotton, G.. E., Gorman, C. A., and Mayberry, W. E., New England 40, 583. Journal of Medicine, 1971, 285, 529. 20 Evered, D. C., et al., British Medical.Journal, 1973, 1, 657. 24 Utiger, R. D., Journal of Clinical Investigation, 1965, 44, 1277. Clobetasone Butyrate, A New Topical Corticosteroid: Clinical Activity and Effects on Pituitary-Adrenal Axis Function and Model of Epidermal Atrophy D. D. MUNRO, LYN WILSON British Medical Journal, 1975, 3, 626-628 Studies THE DRUG Summary ClobetasQne butyrate is 21-chloro-11 dehydro betamethasone 17- butyrate. It was selected for study because screening tests indicated a Clobetasone butyrate is a new corticosteroid, selected separation of topical from systemic activity. The comparative values for study because of its combitation of good activity in for topical and systemic activityl of clobetasone butyrate and five the vasoconstriction test and low systemic activity in other steroids are given in the table (in arbitrary units). animals. Formulated as an 005o% ointment and cream (MolivateN it was clinically effective in patients with Comparative Topical (Vasoconstriction) and Systemic (Thymus Involution) eczema, its activity being significantly greater than that Activities of Six Corticosteroids of hydrocortisone 1% or fluocortolone 020°, (Ultradil). -

Malta Medicines List April 08
Defined Daily Doses Pharmacological Dispensing Active Ingredients Trade Name Dosage strength Dosage form ATC Code Comments (WHO) Classification Class Glucobay 50 50mg Alpha Glucosidase Inhibitor - Blood Acarbose Tablet 300mg A10BF01 PoM Glucose Lowering Glucobay 100 100mg Medicine Rantudil® Forte 60mg Capsule hard Anti-inflammatory and Acemetacine 0.12g anti rheumatic, non M01AB11 PoM steroidal Rantudil® Retard 90mg Slow release capsule Carbonic Anhydrase Inhibitor - Acetazolamide Diamox 250mg Tablet 750mg S01EC01 PoM Antiglaucoma Preparation Parasympatho- Powder and solvent for solution for mimetic - Acetylcholine Chloride Miovisin® 10mg/ml Refer to PIL S01EB09 PoM eye irrigation Antiglaucoma Preparation Acetylcysteine 200mg/ml Concentrate for solution for Acetylcysteine 200mg/ml Refer to PIL Antidote PoM Injection injection V03AB23 Zovirax™ Suspension 200mg/5ml Oral suspension Aciclovir Medovir 200 200mg Tablet Virucid 200 Zovirax® 200mg Dispersible film-coated tablets 4g Antiviral J05AB01 PoM Zovirax® 800mg Aciclovir Medovir 800 800mg Tablet Aciclovir Virucid 800 Virucid 400 400mg Tablet Aciclovir Merck 250mg Powder for solution for inj Immunovir® Zovirax® Cream PoM PoM Numark Cold Sore Cream 5% w/w (5g/100g)Cream Refer to PIL Antiviral D06BB03 Vitasorb Cold Sore OTC Cream Medovir PoM Neotigason® 10mg Acitretin Capsule 35mg Retinoid - Antipsoriatic D05BB02 PoM Neotigason® 25mg Acrivastine Benadryl® Allergy Relief 8mg Capsule 24mg Antihistamine R06AX18 OTC Carbomix 81.3%w/w Granules for oral suspension Antidiarrhoeal and Activated Charcoal -

Pharmacokinetics of Ophthalmic Corticosteroids
British Journal ofOphthalmology 1992; 76: 681-684 681 MINI REVIEW Br J Ophthalmol: first published as 10.1136/bjo.76.11.681 on 1 November 1992. Downloaded from Pharmacokinetics of ophthalmic corticosteroids Corticosteroids have been used by ophthalmologists with an identical vehicle, the aqueous humour concentrations of increasing frequency over the past 30 years, with the these steroids are almost identical.'9 None the less it is concomitant development of a diverse range of drop, essential when considering such empirical data, to recall that ointment, subconjunctival, and oral preparations. Though the systemic anti-inflammatory effect of both betamethasone the clinical benefits and side effects of such corticosteroid and dexamethasone is five to seven times that of predniso- preparations have been well documented, their basic lone.39"' The local anti-inflammatory potency of ocular pharmacokinetics in the human eye have yet to be fully steroids has yet to be fully investigated and whilst early work established. Indeed most of our pharmacokinetic knowledge suggested that prednisolone acetate 1% had the greatest anti- of these drugs has been elucidated by extrapolation of data inflammatory effect in experimental keratitis,'7 later studies obtained from rabbit experiments.1-26 These results can be demonstrated that fluorometholone acetate in a 1% formu- significantly disparate from human data because of the lation was equally efficacious in the same model.26 However, thinner rabbit cornea, lower rabbit blink rate, effect of prednisolone -

For TOR – Expansion Case
SEAC, Gujarat: Page 1 of 10 For TOR – Expansion Case 1. Basic Information of the Project: i Name & Address of the Project site (Complete M/s. Stermone Chemicals Pvt. Ltd., details with plot no./Survey no., Landmark etc. ) Plot No. 34/01, Paldi, Golana Road, Taluka: Khambhat, Dist.Anand ii Name of the Applicant Mr. Premchand S. Patil iii Address for correspondence Plot No. 34/01, Paldi, Golana Road, Taluka: Khambhat, Dist. Anand iv Contact no. and e-mail ID of the Applicant [email protected] Cell No:- +91-9727877450 v Aerial distance of nearest Habitat (KM) Khambhat : 6.40 km vi Longitude & Latitude of the Project Site: (4 Project Site: corners of the site) 1) 22˚ 21’ 40 .38” N 72˚ 35’ 02 .10” E 2) 22˚ 21’ 39 .40” N 72˚ 35’ 06 .30” E 3) 22˚ 21’ 41 .69” N 72˚ 35’ 09 .21” E 4) 22˚ 21’ 43 .69” N 72˚ 35’ 04 .62” E vii Category as per the Schedule to the EIA 5(f) , “Category B” Notification 2006 i.e. 1(d), 2(b), 5(f) etc. viii Applicability of General Conditions of EIA -- Notification 2006: i.e. Ensure that I. Protected areas notified under the Wildlife (Protection) Act, 1972; II. CEPI areas III. Eco-sensitive areas and IV. Inter-state boundaries and international boundaries; are not located within 5 km or 10 km (as the case may be) area from the boundary of the proposed site. 2. Online application proposal no. : _______ 3. Date of application for TOR: 14/02/2018 4. Project status: Expansion 5. -

G/TBT/N/CAN/435 11 December 2014 (14-7223) Page: 1/2 Committee on Technical Barriers to Trade Original
G/TBT/N/CAN/435 11 December 2014 (14-7223) Page: 1/2 Committee on Technical Barriers to Trade Original: English/French NOTIFICATION The following notification is being circulated in accordance with Article 10.6 1. Notifying Member: CANADA If applicable, name of local government involved (Article 3.2 and 7.2): 2. Agency responsible: Department of Health Name and address (including telephone and fax numbers, email and website addresses, if available) of agency or authority designated to handle comments regarding the notification shall be indicated if different from above: Canada's SPS & TBT Notification Authority and Enquiry Point Foreign Affairs, Trade and Development Canada Technical Barriers and Regulations Division (TIB) 111 Sussex Drive Ottawa, ON K1A 0G2 Canada Telephone: (343)203-4273 Fax: (613)943-0346 E-mail: [email protected] 3. Notified under Article 2.9.2 [ X ], 2.10.1 [ ], 5.6.2 [ ], 5.7.1 [ ], other: 4. Products covered (HS or CCCN where applicable, otherwise national tariff heading. ICS numbers may be provided in addition, where applicable): Prescription status of medicinal ingredients for human use (ICS: 11.120; HS: 3004.90) 5. Title, number of pages and language(s) of the notified document: Notice of Consultation- Prescription Drug List (PDL): Mometasone Furoate Monohydrate (2 pages, in English and French) 6. Description of content: The purpose of this Notice of Consultation is to provide an opportunity to comment on the proposal to revise the listing for Adrenocortical hormones on the Prescription Drug List (PDL) to allow the nonprescription use of Mometasone furoate monohydrate for the conditions listed below. -
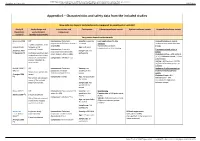
Appendix 6 – Characteristics and Safety Data from the Included Studies
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Open Appendix 6 – Characteristics and safety data from the included studies How safe are topical corticosteroids compared to emollient or vehicle? Study ID Study design and Intervention and Participants Cutaneous adverse events Systemic adverse events Unspecified adverse events (Systematic study duration comparator review*) (Quality assessment) Very potent topical corticosteroids Breneman 2003 RCT Intervention: Clobetasol Severity: moderate Local application site skin Unspecified adverse events (1) propionate 0.05% lotion (twice a to severe reactions Incidence comparable between 2 weeks treatment, then day) (n=96) No clinically significant groups. (unpublished) followed up for Age: ≥ 12 years telangiectasia or skin thinning additional 2 weeks Intervention: Clobetasol Treatment-related adverse (Feldman 2005 Sample size: 229 propionate 0.05% emollient events (2) Nankervis (3)) Cochrane risk of bias tool: participants cream (twice a day) (n=100) Clobetasol lotion = 4/96 patients randomisation described, (4.2%); Clobetasol cream = 1/100 allocation concealment Comparator: Vehicle (n=33) patients (1%) unclear, intention-to- Vehicle = 6/33 patients (18.2%) treat unclear. (Difference between groups: p= 0.0006a) Kimball 2008 (4) RCT Intervention: Clobetasol Severity: not Incidence of adverse events or (trial a) propionate emulsion specified in the treatment related adverse Duration not specified in formulation foam 0.05% review events (Frangos 2008 review Clobetasol foam = 8% (5)) Comparator: Vehicle Age: not specified in Risk of bias not assessed Vehicle foam = 10% the review in any of the included (no significant differences systematic reviews. -

Improved Penetrating Topical Pharmaceutical Compositions Containing Corticosteroids
Europaisches Patentamt ® European Patent Office © Publication number: 0 129 283 Office europeen des brevets A2 © EUROPEAN PATENT APPLICATION © Application number: 84200821.1 ©Int CI.3: A 61 K 31/57 A 61 K 47/00, A 61 K 9/06 © Date of filing: 12.06.84 © Priority: 21.06.83 US 506274 © Applicant: THE PROCTER & GAMBLE COMPANY 01.02.84 US 576065 301 East Sixth Street Cincinnati Ohio 45201 (US) © Date of publication of application: © Inventor: Cooper, Eugene Rex 27.12.84 Bulletin 84/52 2425 Ambassador Drive Cincinnati, OH 45231 (US) © Designated Contracting States: BE CH DE FR GB IT Li NL SE © Inventor: Loomans, Maurice Edward 5231 Jessup Road Cincinnati, OH 45239IUS) © Inventor: Fawzi, Mahdi Bakir 11 Timberline Drive Flanders New Jersey 07836(US) © Representative: Suslic, Lydia et al, Procter & Gamble European Technical Center Temselaan 100 B-1820 Strombeek-Bever(BE) © Improved penetrating topical pharmaceutical compositions containing corticosteroids. Topical pharmaceutical compositions containing a cor- ticosteroid component and a penetration-enhancing vehicle are disclosed. The vehicle comprises a binary combination of a C3-C4 diol and a "cell-envelope disordering compound". The vehicle provides marked transepidermal and percutaneous delivery of corticosteroids. A method of treating certain rheumatic and inflammatory conditions, systemically or loc- ally, is also disclosed. TECHNICAL FIELD The present invention relates to topical compositions effective in delivering high levels of certain pharmaceutically-active cor- ticosteroid agents through the integument. Because of the ease of access, dynamics of application, large surface area, vast exposure to the circulatory and lymphatic networks, and non-invasive nature of the treatment, the delivery of pharmaceutically-active agents through the skin has long been a promising concept.