Future Diagnostic & Therapeutic Targets in Cardiorenal Syndromes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Guidelines on Pulmonary Hypertension 2015 (TF08) - Task Force Members and Additional Contributors
Guidelines on Pulmonary Hypertension 2015 (TF08) - Task Force Members and Additional Contributors For ESC Guidelines: The report below lists declarations of interest as reported to the ESC by the experts covering the period of the Guidelines production, from Task Force creation to publication. Expert Type of Relationship with Industry Beghetti Maurice A - Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc. - Novartis : Pulmonary hypertension imatinib (2012) - Pfizer : Pulmonary hypertension sildenafil (2012-2013) - Bayer Schering Pharma : Pulmonary hypertension riociguat (2012-2013-2014-2015) - Eli Lilly : Pulmonary hypertension tadalafil (2012-2013-2014-2015) - Actelion : Pulmonary hypertension, Tracleer, Macitentan, Selexipag (2012-2013-2014-2015) - GlaxoSmithKline : pulmonary hypertension Ambrisentan (2012-2015) - Novartis : Pulmonary hypertension riociguat (2013) - GlaxoSmithKline : ambrisentan (2014) D - Research funding (departmental or institutional). - Actelion : no relation to a specific product (2012-2013) - Bayer Schering Pharma : no relation to a specific product (2014-2015) Galie Nazzareno A - Direct Personal payment: Speaker fees, Honoraria, Consultancy, Advisory Board fees, Investigator, Committee Member, etc. - Eli Lilly : pulmonary hypertension (2012-2013) - Novartis : pulmonary hypertension (2012-2013) - Pfizer : pulmonary hypertension (2012-2013) - Actelion : pulmonary hypertension (2012-2013) - GlaxoSmithKline : pulmonary hypertension (2012-2013) -

Cardiorenal Syndrome in Patients with Heart Failure
CARDIORENAL SYNDROME IN PATIENTS WITH HEART FAILURE IN KANO. A DISSERTATION SUBMITTED TO THE NATIONAL POSTGRADUATE MEDICAL COLLEGE OF NIGERIA IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE AWARD OF FELLOWSHIP OF THE COLLEGE IN INTERNAL MEDICINE (CARDIOLOGY). BY DR MUHAMMAD NAZIR SHEHU M.B, B.S [B.U.K.] 2002 DEPARTMENT OF MEDICINE AMINU KANO TEACHING HOSPITAL, KANO. MAY 2014 i DECLARATION I hereby declare that this work is original unless otherwise acknowledged. This work has not been presented to any other College for Fellowship and has not been submitted elsewhere for publication. Signature---------------------------- Date---------------------- DR MUHAMMAD NAZIR SHEHU May 2014 ii CERTIFICATION I SUPERVISORS’ CERTIFICATION This study reported in this Dissertation was done by the candidate under our supervision. We also supervised the writing of the Dissertation. SUPERVISOR 1. SIGNATURE/DATE:……………………………………………….. Professor SA Isezuo (FMCP) Professor of Medicine and Consultant Physician/Cardiologist, Usman Danfodiyo University Teaching Hospital,Sokoto. 2. SIGNATURE/DATE:……………………………………………….. Professor B. N. Okeahialam, (FWACP). Professor of Medicine and Consultant Physician/Cardiologist, Jos University Teaching Hospital, Jos, Plateau State, Nigeria. 3. SIGNATURE/DATE:------------------------------------------------------- DR M. M. BORODO (FMCP) Associate Professor of Medicine and Consultant Physician/Gastroenterologist, Aminu Kano Teaching Hospital, Kano, Kano State, Nigeria. iii CERTIFICATION II HEAD OF DEPARTMENT’S CERTIFICATION This -

Classification Decisions Taken by the Harmonized System Committee from the 47Th to 60Th Sessions (2011
CLASSIFICATION DECISIONS TAKEN BY THE HARMONIZED SYSTEM COMMITTEE FROM THE 47TH TO 60TH SESSIONS (2011 - 2018) WORLD CUSTOMS ORGANIZATION Rue du Marché 30 B-1210 Brussels Belgium November 2011 Copyright © 2011 World Customs Organization. All rights reserved. Requests and inquiries concerning translation, reproduction and adaptation rights should be addressed to [email protected]. D/2011/0448/25 The following list contains the classification decisions (other than those subject to a reservation) taken by the Harmonized System Committee ( 47th Session – March 2011) on specific products, together with their related Harmonized System code numbers and, in certain cases, the classification rationale. Advice Parties seeking to import or export merchandise covered by a decision are advised to verify the implementation of the decision by the importing or exporting country, as the case may be. HS codes Classification No Product description Classification considered rationale 1. Preparation, in the form of a powder, consisting of 92 % sugar, 6 % 2106.90 GRIs 1 and 6 black currant powder, anticaking agent, citric acid and black currant flavouring, put up for retail sale in 32-gram sachets, intended to be consumed as a beverage after mixing with hot water. 2. Vanutide cridificar (INN List 100). 3002.20 3. Certain INN products. Chapters 28, 29 (See “INN List 101” at the end of this publication.) and 30 4. Certain INN products. Chapters 13, 29 (See “INN List 102” at the end of this publication.) and 30 5. Certain INN products. Chapters 28, 29, (See “INN List 103” at the end of this publication.) 30, 35 and 39 6. Re-classification of INN products. -

The Evolution of Heart Failure with Reduced Ejection Fraction Pharmacotherapy: What Do We Have and Where Are We Going?
Pharmacology & Therapeutics 178 (2017) 67–82 Contents lists available at ScienceDirect Pharmacology & Therapeutics journal homepage: www.elsevier.com/locate/pharmthera Associate editor: M. Curtis The evolution of heart failure with reduced ejection fraction pharmacotherapy: What do we have and where are we going? Ahmed Selim, Ronald Zolty, Yiannis S. Chatzizisis ⁎ Division of Cardiovascular Medicine, University of Nebraska Medical Center, Omaha, NE, USA article info abstract Available online 21 March 2017 Cardiovascular diseases represent a leading cause of mortality and increased healthcare expenditure worldwide. Heart failure, which simply describes an inability of the heart to meet the body's needs, is the end point for many Keywords: other cardiovascular conditions. The last three decades have witnessed significant efforts aiming at the discovery Heart failure of treatments to improve the survival and quality of life of patients with heart failure; many were successful, Reduced ejection fraction while others failed. Given that most of the successes in treating heart failure were achieved in patients with re- Pharmacotherapy duced left ventricular ejection fraction (HFrEF), we constructed this review to look at the recent evolution of Novel drugs HFrEF pharmacotherapy. We also explore some of the ongoing clinical trials for new drugs, and investigate poten- tial treatment targets and pathways that might play a role in treating HFrEF in the future. © 2017 Elsevier Inc. All rights reserved. Contents 1. Introduction.............................................. -

Cardio-Renal Syndrome
Kelly Li RSC Symposium 2017 . 40-50% of patients with HF have co-existing CKD (GFR<60) . Reductions in GFR strongly affect all-cause mortality in HF patients . CKD is a powerful independent risk factor for the development and progression of CVD and outcomes . >60% CKD patients have CVD, and degree of CVD correlates with CKD severity . Patients with stage 3 or higher CKD have a threefold higher risk of HF . Systemic disorders can cause both cardiac and renal dysfunction Schefold et al Nature Reviews Nephrology 2016 Comorbid conditions at end of year Australia 40 30 20 % % of patients Coronary 10 Peripheral vascular Lung Cerebrovascular 0 2005 2007 2009 2011 2013 2015 Suspected cases included 2016 ANZDATA Annual Report, Figure 2.10 Cause of death Deaths occurring during 2015 Australia New Zealand 100 80 60 Percent 40 20 0 HD PD Tx HD PD Tx Cardiovascular Withdrawal Cancer Infection Other 2016 ANZDATA Annual Report, Figure 3.5 Wali et al JACC 2005 Figure 2. Kaplan-Meier plot of cumulative incidence of cardiovascular death or unplanned admission to hospital for the management of worsening CHF stratified by approximate quintiles of eGFR in mL/min per 1.73 m2 (time in years). Hillege et al Circulation 2016 Schefold et al Nature Reviews Nephrology 2016 Schefold et al Nature Reviews Nephrology 2016 . Cardiorenal syndrome complex and bi-directional . Haemodynamic interactions . Neurohormonal dysregulation . Inflammation and other metabolic changes Schefold et al Nature Reviews Nephrology 2016 Schefold et al Nature Reviews Nephrology 2016 Schefold et al Nature Reviews Nephrology 2016 Schefold et al Nature Reviews Nephrology 2016 Schefold et al Nature Reviews Nephrology 2016 Schefold et al Nature Reviews Nephrology 2016 Schefold et al Nature Reviews Nephrology 2016 Schefold et al Nature Reviews Nephrology 2016 Schefold et al Nature Reviews Nephrology 2016 . -

Involvement of Cyclic Guanosine Monophosphate-Dependent Protein Kinase I in Renal Antifibrotic Effects of Serelaxin
fphar-07-00195 July 9, 2016 Time: 13:1 # 1 View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Frontiers - Publisher Connector ORIGINAL RESEARCH published: 12 July 2016 doi: 10.3389/fphar.2016.00195 Involvement of Cyclic Guanosine Monophosphate-Dependent Protein Kinase I in Renal Antifibrotic Effects of Serelaxin Veronika Wetzl1,2†, Elisabeth Schinner1†, Frieder Kees1, Franz Hofmann3, Lothar Faerber1,2 and Jens Schlossmann1* 1 Department of Pharmacology and Toxicology, University of Regensburg, Regensburg, Germany, 2 Novartis Pharma GmbH, Nuremberg, Germany, 3 Institute of Pharmacology and Toxicology, Technical University of Munich, Munich, Germany Introduction: Kidney fibrosis has shown to be ameliorated through the involvement of cyclic guanosine monophosphate (cGMP) and its dependent protein kinase I (cGKI). Serelaxin, the recombinant form of human relaxin-II, increases cGMP levels and has Edited by: Enno Klussmann, shown beneficial effects on kidney function in acute heart failure patients. Antifibrotic Max Delbrüeck Center for Molecular properties of serelaxin are supposed to be mediated via relaxin family peptide receptor Medicine, Germany 1 and subsequently enhanced nitric oxide/ cGMP to inhibit transforming growth factor- Reviewed by: Friedrich Wilhelm Herberg, b (TGF-b) signaling. This study examines the involvement of cGKI in the antifibrotic University of Kassel, Germany signaling of serelaxin. Choel Kim, Baylor College of Medicine, USA Methods and Results: Kidney fibrosis was induced by unilateral ureteral obstruction in *Correspondence: wildtype (WT) and cGKI knock-out (KO) mice. After 7 days, renal antifibrotic effects Jens Schlossmann of serelaxin were assessed. Serelaxin treatment for 7 days significantly increased [email protected] regensburg.de cGMP in the kidney of WT and cGKI-KO. -

Jimmunol.1800856.Full.Pdf
Healthy Donors Exhibit a CD4 T Cell Repertoire Specific to the Immunogenic Human Hormone H2-Relaxin before Injection This information is current as of September 26, 2021. Aurélien Azam, Yann Gallais, Sergio Mallart, Stephane Illiano, Olivier Duclos, Catherine Prades and Bernard Maillère J Immunol published online 17 May 2019 http://www.jimmunol.org/content/early/2019/05/14/jimmun Downloaded from ol.1800856 Supplementary http://www.jimmunol.org/content/suppl/2019/05/14/jimmunol.180085 http://www.jimmunol.org/ Material 6.DCSupplemental Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists by guest on September 26, 2021 • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2019 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Published May 17, 2019, doi:10.4049/jimmunol.1800856 The Journal of Immunology Healthy Donors Exhibit a CD4 T Cell Repertoire Specific to the Immunogenic Human Hormone H2-Relaxin before Injection Aure´lien Azam,*,† Yann Gallais,† Sergio Mallart,‡ Stephane Illiano,x Olivier Duclos,‡ Catherine Prades,* and Bernard Maille`re† H2-relaxin (RLN2) is a two-chain peptide hormone structurally related to insulin with a therapeutic potential in multiple indica- tions. -

Cardiorenal Syndrome: Emerging Role of Medical Imaging for Clinical Diagnosis and Management
Journal of Personalized Medicine Review Cardiorenal Syndrome: Emerging Role of Medical Imaging for Clinical Diagnosis and Management Ling Lin 1 , Xuhui Zhou 2,* , Ilona A. Dekkers 1 and Hildo J. Lamb 1 1 Cardiovascular Imaging Group (CVIG), Department of Radiology, Leiden University Medical Center, 2333 ZA Leiden, The Netherlands; [email protected] (L.L.); [email protected] (I.A.D.); [email protected] (H.J.L.) 2 Department of Radiology, The Eighth Affiliated Hospital of Sun Yat-sen University, Shenzhen 510833, China * Correspondence: [email protected]; Tel.: +86-755-83982222 Abstract: Cardiorenal syndrome (CRS) concerns the interconnection between heart and kidneys in which the dysfunction of one organ leads to abnormalities of the other. The main clinical challenges associated with cardiorenal syndrome are the lack of tools for early diagnosis, prognosis, and evaluation of therapeutic effects. Ultrasound, computed tomography, nuclear medicine, and magnetic resonance imaging are increasingly used for clinical management of cardiovascular and renal diseases. In the last decade, rapid development of imaging techniques provides a number of promising biomarkers for functional evaluation and tissue characterization. This review summarizes the applicability as well as the future technological potential of each imaging modality in the assessment of CRS. Furthermore, opportunities for a comprehensive imaging approach for the evaluation of CRS are defined. Citation: Lin, L.; Zhou, X.; Dekkers, Keywords: cardiorenal syndrome; imaging biomarker; tissue characterization I.A.; Lamb, H.J. Cardiorenal Syndrome: Emerging Role of Medical Imaging for Clinical Diagnosis and Management. J. Pers. Med. 2021, 11, 1. Introduction 734. https://doi.org/10.3390/ Cardiorenal syndrome (CRS) is an umbrella term describing the interactions between jpm11080734 concomitant cardiac and renal dysfunctions, in which acute or chronic dysfunction of one organ may induce or precipitate dysfunction of the other [1]. -
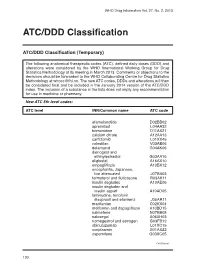
ATC/DDD Classification
WHO Drug Information Vol. 27, No. 2, 2013 ATC/DDD Classification ATC/DDD Classification (Temporary) The following anatomical therapeutic codes (ATC), defined daily doses (DDD) and alterations were considered by the WHO International Working Group for Drug Statistics Methodology at its meeting in March 2013. Comments or objections to the decisions should be forwarded to the WHO Collaborating Centre for Drug Statistics Methodology at [email protected]. The new ATC codes, DDDs and alterations will then be considered final and be included in the January 2014 version of the ATC/DDD index. The inclusion of a substance in the lists does not imply any recommendation for use in medicine or pharmacy. New ATC 5th level codes: ATC level INN/Common name ATC code afamelanotide D02BB02 apremilast L04AA32 brimonidine D11AX21 calcium citrate A12AA13 carfilzomib L01XX45 colestilan V03AE06 delamanid G04AK06 dienogest and ethinylestradiol G03AA16 eliglustat A16AX10 empagliflozin A10BX12 encephalitis, Japanese, live attenuated J07BA03 formoterol and fluticasone R03AK11 insulin degludec A10AE06 insulin degludec and insulin aspart A10AD05 lamivudine, tenofovir disoproxil and efavirenz J05AR11 macitentan C02KX04 metformin and dapagliflozin A10BD15 nalmefene N07BB05 naloxegol A06AH03 nomegestrol and estrogen G03FB12 obinutuzumab L01XC15 ocriplasmin S01AX22 ospemifene G03XC05 Continued/ 130 WHO Drug Information Vol. 27, No. 2, 2013 ATC/DDD Classification ATC level INN/Common name ATC code pomalidomide L04AX06 serelaxin C01DX21 strontium ranelate and colecalciferol -

Cardiorenal Syndrome
Journal of the American College of Cardiology Vol. 52, No. 19, 2008 © 2008 by the American College of Cardiology Foundation ISSN 0735-1097/08/$34.00 Published by Elsevier Inc. doi:10.1016/j.jacc.2008.07.051 STATE-OF-THE-ART PAPER Cardiorenal Syndrome Claudio Ronco, MD,* Mikko Haapio, MD,† Andrew A. House, MSC, MD,‡ Nagesh Anavekar, MD,§ Rinaldo Bellomo, MD¶ Vicenza, Italy; Helsinki, Finland; London, Ontario, Canada; and Melbourne, Australia The term cardiorenal syndrome (CRS) increasingly has been used without a consistent or well-accepted defini- tion. To include the vast array of interrelated derangements, and to stress the bidirectional nature of heart- kidney interactions, we present a new classification of the CRS with 5 subtypes that reflect the pathophysiology, the time-frame, and the nature of concomitant cardiac and renal dysfunction. CRS can be generally defined as a pathophysiologic disorder of the heart and kidneys whereby acute or chronic dysfunction of 1 organ may induce acute or chronic dysfunction of the other. Type 1 CRS reflects an abrupt worsening of cardiac function (e.g., acute cardiogenic shock or decompensated congestive heart failure) leading to acute kidney injury. Type 2 CRS comprises chronic abnormalities in cardiac function (e.g., chronic congestive heart failure) causing progressive chronic kidney disease. Type 3 CRS consists of an abrupt worsening of renal function (e.g., acute kidney isch- emia or glomerulonephritis) causing acute cardiac dysfunction (e.g., heart failure, arrhythmia, ischemia). Type 4 CRS describes a state of chronic kidney disease (e.g., chronic glomerular disease) contributing to decreased car- diac function, cardiac hypertrophy, and/or increased risk of adverse cardiovascular events. -
Heart Failure
Heart Failure Peter A. McCullough, MD, MPH, FACC, FACP, FAHA, FCCP Consultant Cardiologist, Chief Academic and Scientific Officer St. John Providence Health System Providence Park Heart Institute Novi, MI USA e-mail: [email protected] Outline Definitions Complex, bidirectional pathogenesis Example of novel target Therapy Putting it all together Outline Definitions Complex, bidirectional pathogenesis Example of novel target Therapy Putting it all together Definition of Heart Failure (HF) •• TheThe failure of the heart as a pump resulting in inadequate cardiac output to peripheral tissues and stasis of blood in the lungs resulting most commonly in fatigue and pulmonary congestion.congestion. •• A complex mechanical and neurohumoral syndrome characterized by effort intolerance, fluid retention, and reduced longevity. •• At least 7 definitions in the literature based on tested scoring schemes and expert opinion. Heart Failure as a Clinical Clinical presentationSyndrome of acute kidney injury Stasis of blood, tissue deposition of water and salt resulting in effort intolerance, progressive dyspnea, fatigue, edema Definition and Classification of the Cardio-Renal Syndromes Cardio-Renal Syndromes (CRS) General Definition: Disorders of the heart and kidneys whereby acute or chronic dysfunction in one organ may induce acute or chronic dysfunction of the other Acute Cardio-Renal Syndrome (Type 1) Acute worsening of cardiac function leading to renal dysfunction Chronic Cardio-Renal Syndrome (Type 2) Chronic abnormalities in cardiac -

Amiodarone-Induced Hypothyroidism Presenting As Cardiorenal Syndrome
Hindawi Publishing Corporation Case Reports in Cardiology Volume 2012, Article ID 161450, 3 pages doi:10.1155/2012/161450 Case Report Amiodarone-Induced Hypothyroidism Presenting as Cardiorenal Syndrome Evan L. Hardegree1 and Robert C. Albright2 1 Department of Medicine, Mayo Clinic, 200 First Street SW, Rochester, MN 55905, USA 2 Division of Nephrology and Hypertension, Mayo Clinic, 200 First Street SW, Rochester, MN 55905, USA CorrespondenceshouldbeaddressedtoEvanL.Hardegree,[email protected] Received 6 March 2012; Accepted 14 May 2012 Academic Editors: H. Kitaoka and A. J. Mansur Copyright © 2012 E. L. Hardegree and R. C. Albright. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Here we present the case of a 90-year-old man with chronic heart and renal failure who was admitted with what appeared to be a simple heart failure exacerbation. However, further investigation led to the diagnosis of profound amiodarone-induced hypothy- roidism as the cause of his acute decompensation, highlighting the importance of a broad differential diagnosis and thorough investigation. 1. Introduction (LVEF) of 15% with a dual-chamber pacemaker for car- diac resynchronization; paroxysmal atrial fibrillation and In patients with concurrent heart and renal failure (cardiore- frequent ven-tricular ectopy requiring initiation of amio- nal syndrome), common causes of decompensation may in- darone 6 months prior (200 mcg/day); stage IV chronic clude myocardial ischemia, excessive salt ingestion, and med- kidney disease, not on dialysis. The patient reported full ication noncompliance. However, there are many conditions compliance with his medical heart failure regimen and that may tip this delicate balance.