HIPAA & the ACH Network
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Neobank Varo on Serving Customers' Needs As P2P Payments See A
AUGUST 2021 Neobank Varo on serving customers’ needs as P2P payments see Nigerian consumers traded $38 million worth of bitcoin on P2P platforms within the past month a rapid rise in usage — Page 12 (News and Trends) — Page 8 (Feature Story) How P2P payments are growing more popular for a range of use cases, and why interoperability will be needed to keep growth robust — Page 16 (Deep Dive) © 2021 PYMNTS.com All Rights Reserved 1 DisbursementsTracker® Table Of Contents WHATʼS INSIDE A look at recent disbursements developments, including why P2P payments are becoming more valuable 03 to consumers and businesses alike and how these solutions are poised to grow even more popular in the years ahead FEATURE STORY An interview with with Wesley Wright, chief commercial and product officer at neobank Varo, on the rapid 08 rise of P2P payments adoption among consumers of all ages and how leveraging internal P2P platforms and partnerships with third-party providers can help FIs cater to customer demand NEWS AND TRENDS The latest headlines from the disbursements space, including recent survey results showing that almost 12 80 percent of U.S. consumers used P2P payments last year and how the U.K. government can take a page from the U.S. in using instant payments to help SMBs stay afloat DEEP DIVE An in-depth look at how P2P payments are meeting the needs of a growing number of consumers, how 16 this shift has prompted consumers to expand how they leverage them and why network interoperability is key to helping the space grow in the future PROVIDER DIRECTORY 21 A look at top disbursement companies ABOUT 116 Information on PYMNTS.com and Ingo Money ACKNOWLEDGMENT The Disbursements Tracker® was produced in collaboration with Ingo Money, and PYMNTS is grateful for the companyʼs support and insight. -

(12) United States Patent (10) Patent No.: US 8,417,636 B2 Love Et Al
USOO841.7636B2 (12) United States Patent (10) Patent No.: US 8,417,636 B2 LOVe et al. (45) Date of Patent: Apr. 9, 2013 (54) APPROVING ACHOPERATOR PROCESSING USPC ............................................................ 705/43 OF ACH PAYMENTS BASED ON AN (58) Field of Classification Search ..................... 705/43 ORIGINATING DEPOSITORY FINANCIAL See application file for complete search history. INSTITUTIONS APPROVED ORIGINATOR LIST (56) References Cited (75) Inventors: Robert Anthony Love, Stockbridge, GA U.S. PATENT DOCUMENTS (US); Lantanya Neale Mauriello, 4,270,042 A 5/1981 Case Suwanee, GA (US); Nesta Valerie 4,727,243 A 2/1988 Savar Reckord-Yarde, Lithonia, GA (US); 4,823,264 A 4/1989 Deming Susan Lynne Robertson, Decatur, GA (Continued) (US); Robert Williams, Decatur, GA (US); Donald E. Nelson, Marietta, GA FOREIGN PATENT DOCUMENTS (US) WO WOOO3OO53 5, 2000 OTHER PUBLICATIONS (73) Assignee: Federal Reserve Bank of Atlanta, Atlanta, GA (US) “Development of interface between FED and Eurogiro', Jan. 14. 2003.* (*) Notice: Subject to any disclaimer, the term of this (Continued) patent is extended or adjusted under 35 U.S.C. 154(b) by 499 days. Primary Examiner — Garcia Ade (21) Appl. No.: 11/416,946 (74)74). Attorney,Att , Agent, or Firm — King & SpaldingSpaldi (57) ABSTRACT (22) Filed: May 3, 2006 Approving automated clearing house (ACH) payments for (65) Prior Publication Data processing by an ACH operator is based on an approved originator list identifying originators authorized by an origi US 2006/02O6427 A1 Sep. 14, 2006 nating depository financial institution (“ODFI) to originate ACH payments and to send those ACH payments to the ACH Related U.S. -
Automated Clearing House (ACH) Key Facts & Responsibilities for ACH Originators
Automated Clearing House (ACH) Key Facts & Responsibilities for ACH Originators Originator Guide July 2020 1 Contents Summary ............................................................................................................................................................... 3 ACH Legal Framework .......................................................................................................................................... 3 Your Responsibilities as an ACH Originator.......................................................................................................... 3 Industry Best Practices ......................................................................................................................................... 4 File Delivery Deadlines & Cutoff Times ................................................................................................................ 4 Direct Deposit Payroll Authorizations (Consumer) .............................................................................................. 4 Debit Authorizations (Consumer) ........................................................................................................................ 4 Corporate Authorizations ..................................................................................................................................... 5 Changing Date or Amount of Debits .................................................................................................................... 5 Pre-Notifications ................................................................................................................................................. -

Electronic Funds Transfer (NACHA) Rules.Pdf
Brigham Young University Office of Compliance and Audit Research Memo NACHA Operating Rules Law/Act: NACHA Operating Rules Public Law Citation: None U.S. Code Citation: None Code of Federal Regulations Citation: None Responsible Regulator: NACHA – The Electronic Payments Association BYU Responsible Officer Richard White, University Treasurer Version 2.0 Effective Date: December 14, 2010 BACKGROUND NACHA – The Electronic Payments Association (NACHA) is a non-profit private-sector trade association that oversees the Automated Clearing House (ACH) Network, which is one of the largest electronic payment transfer networks in the world.1 Formed in 1974 by various state and regional payment associations, NACHA’s purpose was “to establish uniform operating rules for the exchange of ACH payments among ACH associations.”2 Based on NACHA’s work, by 1978 it was possible for two participating financial institutions located in the United States to electronically exchange ACH payments under a common set of rules, known today as the NACHA Operating Rules.3 The ACH Network is a “batch processing, store-and-forward system” that allows for the interbank clearing of electronic payments.4 Electronic transfers in the network are stored then forwarded in batches to their destination banks at a predetermined time.5 ACH payments may include: Direct deposit of payroll, Social Security, and other government benefits; Direct deposit of tax refunds; Direct payment of consumer bills, such as mortgages, loans, utilities, and insurance premiums; Business-to-business -

ACH Network Rules Pandemic-Related Frequently Asked Questions Updated October 27, 2020
ACH Network Rules Pandemic-Related Frequently Asked Questions Updated October 27, 2020 Nacha has developed the following FAQs based on information it has provided, information it has learned, and inquiries posed to Nacha by industry participants. Newly added or revised FAQs are shown at the beginning of each section by date, followed by those previously published. RDFIs Revised October 27, 2020 1. How can an RDFI comply with the rule to obtain the consumer Receiver’s signature on the Written Statement of Unauthorized Debit? In ACH Operations Bulletin #5-2020, Nacha provides relief to RDFIs on the WSUD signature requirement by not enforcing the signature or similar authentication requirement. ACH Operations Bulletin #7-2020 extends this relief indefinitely. Nacha will publish a 30-day advance notice prior to the expiration of this relief. RDFIs that have the ability for consumers to similarly authenticate signatures by remote channels such as online and by telephone should continue to do so 2. If an RDFI has received a request for a copy of a Written Statement of Unauthorized Debit and cannot provide the copy to the ODFI within in ten Banking Days due to the pandemic, will the RDFI be subject to a rules violation? In ACH Operations Bulletin #3-2020, Nacha provides relief to RDFIs from the 10 Banking Day deadline for providing copies of WSUDs to ODFIs. ACH Operations Bulletin #7-2020 extends this relief indefinitely. Nacha will not enforce cases in which a WSUD is provided after the existing 10 Banking Day time frame, but is provided within 20 Banking Days. -
Entitlement Descriptions Mapping and Options Guide
J.P. Morgan Access® Entitlement Descriptions Mapping and Options Guide TM • Administration • J.P. Morgan Concourse • Cash Reports • J.P. Morgan Host-to-Host File Settings and Visibility • Checks • J.P. Morgan Host-to-Host Reporting • Commercial Loans • Merchant Services Reports • Counterparty Portal • Payments TM • Data Once • Statements • Digital Payments • Virtual Account Management (VAM) Portal • Electronic Specialty Account Portal • Virtual Branch • FX • More Services • Global ACH • Utilities • Host-to-Host Online • Security Token ® • J.P. Morgan Access Liquidity Solutions • J.P. Morgan Defined Roles for Express Setup J.P. Morgan Access® Last modified: July 21, 2020 This guide is confidential and proprietary to J.P. Morgan and is provided for your general information only. It is subject to change without notice and is not intended to be legally binding. All services described in this guide are subject to applicable laws and regulations and service terms. Not all products and services are available in all locations. Eligibility for particular products and services will be determined by JPMorgan Chase Bank, N.A. or its affiliates. J.P. Morgan makes no representation as to the legal, regulatory or tax implications of the matters referred to in this guide. J.P. Morgan is a marketing name for the Wholesale Payments businesses of JPMorgan Chase Bank, N.A. and its affiliates worldwide. JPMorgan Chase Bank, N.A., organized under the laws of U.S.A. with limited liability. ©2020 JPMorgan Chase & Co. All rights reserved. 2 J.P. Morgan Access® -

Electronic Funds Transfer Agreement
141180_Muskegon_FCU_EFT_ Agreement_F1.qxp_.qxd 4/26/18 3:48 PM Page 1 11. Confidentiality: In general, you agree that we may disclose information 14. Regulatory Agency: If you believe that we may have violated the 22. Member Liability: You are responsible for all transactions to third parties about your account or the transfers that you make: Michigan Electronic Funds Transfer Act (Michigan Public Act No. 322 you authorize using your electronic funds transfer services under of 1978), you may contact: this Agreement. If you permit someone else to use an electronic A. Where it is necessary for completing transfers, or funds transfer service, your Card or PIN, you are responsible for B. In order to verify the existence and condition of your account for a National Credit Union Administration, Region 1 – Albany any transactions they authorize or conduct on any of your accounts. Electronic third party, such as a credit bureau or merchant, or 9 Washington Square, Washington Avenue Extension If you believe that an electronic funds transfer has been made Albany, NY 12205 C. In order to comply with government agency or court orders, or without your permission, telephoning is the best way of keeping State of Michigan D. If you otherwise give us your written permission. your possible losses down. Department of Insurance and Financial Services You are not liable for an unauthorized MasterCard debit card Funds In addition, if you have a MasterCard debit card, you agree that we may P.O. Box 30224 provide your personal data, to the extent allowed by law, to MasterCard, transaction that was not conducted at an ATM if you can Lansing, MI 48909 demonstrate that you exercised reasonable care in protecting your its Members, or their respective contractors for the purpose of providing 15. -

ACH) Rules for ACH Originators
Automated Clearing House (ACH) Rules for ACH Originators Important Terms ACH NETWORK – The ACH Network is a batch payment system. UniBank forwards entries received from its Originators to the Federal Reserve at the end of the banking day. The Federal Reserve distributes the entries to each Receiving Bank and the Receiving Bank in turn credits or debits its customers. NACHA RULES – NACHA administers the rules that govern the ACH Network. Banks, Originators, and Third Party Service Providers participating in the ACH Network agree to abide by the NACHA Rules. The online copy of the rules may be accessed at http://www.achrulesonline.org/ CREDIT ENTRY – An ACH entry that deposits (credits) funds to a Receiver’s account. DEBIT ENTRY – An ACH entry that withdraws (debits) funds from a Receiver’s account. ORIGINATOR – A company that initiates an ACH debit or credit, through an ODFI or Third-Party Sender, to a Receiver. RECEIVER – The company or individual that receives an ACH debit or credit entry from an Originator. ODFI (ORIGINATING DEPOSITORY FINANCIAL INSTITUTION) – UniBank RDFI (RECEIVING DEPOSITORY FINANCIAL INSTITUTION) – Receiver’s bank. ACH OPERATOR – The Federal Reserve THIRD PARTY SERVICE PROVIDER (TSPS)* – An Organization (not an Originator, ODFI, or RDFI) that performs any functions on behalf of the Originator, ODFI and/or RDFI. This can include the creation of files or acting as a sending point or receiving point for a Participating DFI. (An organization acting as a Third-Party Sender also is a TPSP – see next question for current definition) Examples of TPSP: data processing service bureau, correspondent bank, payable through bank, a banker’s bank, or even a financial institution acting on behalf of another financial institution. -
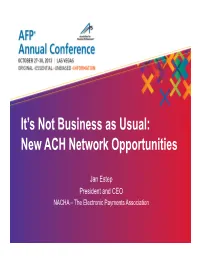
New ACH Network Opportunities
It’s Not Business as Usual: New ACH Network Opportunities Jan Estep President and CEO NACHA – The Electronic Payments Association ACH Network Opportunities • We are actively listening to business needs • We want to help you identify ACH Network solutions • We want to hear from you We are actively listening to business needs Your input has informed the strategic direction of the ACH Network Industry Survey: Longer-Term ACH Network Needs ACH Network should support NACHA should ACH Network ACH Network parallel Users of the ACH focus on should support ACH Network should allow for processing Network expect enabling enhanced should support voluntary or arrangements faster payments increased use of functionality for account “opt‐in” for opt‐in users, and availability ACH credit payment‐related verification applications advanced of funds payments messages applications, or new formats Credit Union 5.7 6.1 8.7 7.0 7.1 8.1 Banks under $5B 5.0 5.4 8.3 7.4 7.4 7.9 Banks over $5B 4.3 5.2 8.0 7.5 7.5 7.8 Tech Provider 5.7 6.6 8.5 7.9 7.6 7.9 End‐user 6.3 6.7 8.3 7.8 7.9 8.9 All Other 5.9 6.4 8.0 7.8 7.9 8.1 (Q15) As you think about the ACH Network and its long-term capabilities into the future, please indicate the degree to which you agree or disagree with the following statements: (Where 1 = Strongly Disagree to 10 = Strongly Agree) The ACH Blueprint Identifies areas of future opportunity – Blueprint “attributes” 1. -
An Overview of Ach
5500 Brooktree Road, Suite 104 Wexford, PA 15090 888-436-5101 www.profituity.com AN OVERVIEW OF ACH © COPYRIGHT 2013, PROFITUITY, LLC Page 2 of 11 Contents Automated Clearing House .................................................................................................................................... 3 The Role of NACHA ................................................................................................................................................... 3 Who Uses ACH ............................................................................................................................................................ 3 How ACH Works ......................................................................................................................................................... 4 Third-Party Service Provider ................................................................................................................................... 4 Various Types of ACH Transactions ..................................................................................................................... 4 Consumer and Non-consumer Checks .............................................................................................................. 6 Check 21......................................................................................................................................................................... 6 Drafts .............................................................................................................................................................................. -

INTERNATIONAL ACH TRANSACTIONS for CORPORATE PRACTITIONERS
INTERNATIONAL ACH TRANSACTIONS for CORPORATE PRACTITIONERS 1. What is an IAT? The IAT is a new Standard Entry Class code for ACH payments to identify international transactions. International transactions are those payments that have been funded internationally or are being sent to another country and a part of the transaction will be processed via the ACH Network. 2. Why was the IAT developed? The IAT was developed in response to a request from the Office of Foreign Asset Control (OFAC). In its letters to NACHA, OFAC stated that it thought that the ACH Network is vulnerable to abuse due to the speed and efficiency of the Network. OFAC understands that there are currently transactions flowing through the Network that are funded by international sources. These transactions cannot currently be identified within the Network and are formatted as domestic transactions. OFAC has requested that NACHA modify the NACHA Operating Rules to adequately identify international transactions and have the banks review the international transactions for OFAC compliance. 3. As a Corporate Originator, does OFAC impact me? Yes, U.S. corporations are also required to comply with OFAC obligations, and the penalties for ignoring those obligations can be both criminal and civil and include both jail time and fines ranging from $10,000 to $10,000,000 per occurrence. If these fines are levied against the financial institution they may be passed back to the corporate originator depending on the specifics of the case and the details of their contract with the financial institution. The fines are levied by the U.S. government and funds collected are the property of the government, not the financial institution. -

Person-To-Person Electronic Funds Transfers: Recent Developments and Policy Issues
No. 10-1 Person-to-Person Electronic Funds Transfers: Recent Developments and Policy Issues Oz Shy Abstract: The paper investigates the reasons why person-to-person electronic funds transfers are still not very common in the United States compared with practices in many other countries. The paper also describes recent enhancements to online and mobile banking that provide account holders with low-cost interfaces to manage person-to-person electronic funds transfers via automated clearing house (ACH). On the theoretical side, the paper characterizes the critical mass levels needed for payment instruments to become widely adopted. Given the Fed's long-term heavy involvement in check clearing, the paper concludes with policy discussions of whether intervention is needed. Keywords: Automated clearing houses (ACH); Person-to-person Electronic Funds Transfers; Account-to-account transfers; Online Banking; Mobile banking. JEL Classifications: E42, G29, D14 Oz Shy is a senior economist at the Federal Reserve Bank of Boston and a member of the Consumer Payments Research Center in the research department. I thank Terri Bradford, Sean Carter, Dickson Chu, Paul Connolly, Marianne Crowe, Jean Fisher, Charles Fletcher, Fumiko Hayashi, Ben Levinger, Suzanne Lorant, Richard Oliver, Scott Schuh, Joanna Stavins, Bob Triest, Marianne Verdier, Mike Zabek, and Jeff Zhang for all their help and guidance. This paper, which may be revised, is available on the web site of the Federal Reserve Bank of Boston at http://www.bos.frb.org/economic/ppdp/index.htm. The views and opinions expressed in this paper are those of the author and do not necessarily represent the views of the Federal Reserve Bank of Boston or the Federal Reserve System.