Case Management Examples Page - 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Case Closed, Vol. 27 Ebook Free Download
CASE CLOSED, VOL. 27 PDF, EPUB, EBOOK Gosho Aoyama | 184 pages | 29 Oct 2009 | Viz Media, Subs. of Shogakukan Inc | 9781421516790 | English | San Francisco, United States Case Closed, Vol. 27 PDF Book January 20, [22] Ai Haibara. Views Read Edit View history. Until Jimmy can find a cure for his miniature malady, he takes on the pseudonym Conan Edogawa and continues to solve all the cases that come his way. The Junior Detective League and Dr. Retrieved November 13, January 17, [8]. Product Details. They must solve the mystery of the manor before they are all killed off or kill each other. They talk about how Shinichi's absence has been filled with Dr. Chicago 7. April 10, [18] Rachel calls Richard to get involved. Rachel thinks it could be the ghost of the woman's clock tower mechanic who died four years prior. Conan's deductions impress Jodie who looks at him with great interest. Categories : Case Closed chapter lists. And they could have thought Shimizu was proposing a cigarette to Bito. An unknown person steals the police's investigation records relating to Richard Moore, and Conan is worried it could be the Black Organization. The Junior Detectives find the missing boy and reconstruct the diary pages revealing the kidnapping motive and what happened to the kidnapper. The Junior Detectives meet an elderly man who seems to have a lot on his schedule, but is actually planning on committing suicide. Magic Kaito Episodes. Anime News Network. Later, a kid who is known to be an obsessive liar tells the Detective Boys his home has been invaded but is taken away by his parents. -

Star Channels, May 3-9, 2020
MAY 3 - 9, 2020 staradvertiser.com MONEY PROBLEMS Showtime’s most provocative corporate drama, Billions, returns for its fi fth season and fans of the show can’t wait to see more of their favorite fi ctional billionaires as they scheme and slither their way to the top of the Wall Street food chain. Paul Giamatti and Damian Lewis star, while Julianna Margulies and Corey Stoll join the cast. Airing Sunday, May 3, on Showtime. A SPECIAL COVID-19 PRESENTATION Join host, Lyla Berg as she speaks with community experts about COVID-19. Tune in Wednesday, May 6 and May 20 at 6:30pm on Channel 53 WEDNESDAYW at 6:30pm - - olelo.org Also available on Olelonet and Olelo YouTube. Channel 53 ¶ ¶ 590126_IslandFocus_Ad_COVID19_2in_R.indd 1 4/30/20 9:29 AM ON THE COVER | BILLIONS A few billion more Wall Street gets a new Prince by the coronavirus pandemic. The first seven disappearance in Season 1 to the two men episodes will air starting this week, and the going head to head in court in Season 3, it ap- in Season 5 of ‘Billions’ show will take a break mid-June at a natural pears the billionaires will squabble over just point in the story arc. At this stage, there is about anything from money and business to By Dana Simpson no way to know when the second part of the women and politics. TV Media season will air, but the much-anticipated re- Just when it seemed they would band maining episodes will be filmed and released together to form an alliance — especially asten your seatbelts for another year of as soon as the production process is safe to with Axe’s focus now more clearly aimed dollars and deceit. -
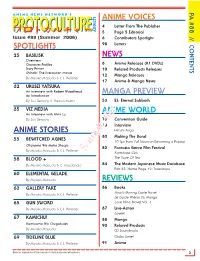
Protoculture Addicts
PA #88 // CONTENTS PA A N I M E N E W S N E T W O R K ' S ANIME VOICES 4 Letter From The Publisher PROTOCULTURE¯:paKu]-PROTOCULTURE ADDICTS 5 Page 5 Editorial Issue #88 (Summer 2006) 6 Contributors Spotlight SPOTLIGHTS 98 Letters 25 BASILISK NEWS Overview Character Profiles 8 Anime Releases (R1 DVDs) Story Primer 10 Related Products Releases Shinobi: The live-action movie 12 Manga Releases By Miyako Matsuda & C.J. Pelletier 17 Anime & Manga News 32 URUSEI YATSURA An interview with Robert Woodhead MANGA PREVIEW An Introduction By Zac Bertschy & Therron Martin 53 ES: Eternal Sabbath 35 VIZ MEDIA ANIME WORLD An interview with Alvin Lu By Zac Bertschy 73 Convention Guide 78 Interview ANIME STORIES Hitoshi Ariga 80 Making The Band 55 BEWITCHED AGNES 10 Tips from Full Moon on Becoming a Popstar Okusama Wa Maho Shoujo 82 Fantasia Genre Film Festival By Miyako Matsuda & C.J. Pelletier Sample fileKamikaze Girls 58 BLOOD + The Taste Of Tea By Miyako Matsuda & C. Macdonald 84 The Modern Japanese Music Database Part 35: Home Page 19: Triceratops 60 ELEMENTAL GELADE By Miyako Matsuda REVIEWS 63 GALLERY FAKE 86 Books Howl’s Moving Castle Novel By Miyako Matsuda & C.J. Pelletier Le Guide Phénix Du Manga 65 GUN SWORD Love Hina, Novel Vol. 1 By Miyako Matsuda & C.J. Pelletier 87 Live-Action Lorelei 67 KAMICHU! 88 Manga Kamisama Wa Chugakusei 90 Related Products By Miyako Matsuda CD Soundtracks 69 TIDELINE BLUE Otaku Unite! By Miyako Matsuda & C.J. Pelletier 91 Anime More on: www.protoculture-mag.com & www.animenewsnetwork.com 3 ○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○ LETTER FROM THE PUBLISHER A N I M E N E W S N E T W O R K ' S PROTOCULTUREPROTOCULTURE¯:paKu]- ADDICTS Over seven years of writing and editing anime reviews, I’ve put a lot of thought into what a Issue #88 (Summer 2006) review should be and should do, as well as what is shouldn’t be and shouldn’t do. -

14-1096 Luna Torres V. Lynch (05/19/2016)
(Slip Opinion) OCTOBER TERM, 2015 1 Syllabus NOTE: Where it is feasible, a syllabus (headnote) will be released, as is being done in connection with this case, at the time the opinion is issued. The syllabus constitutes no part of the opinion of the Court but has been prepared by the Reporter of Decisions for the convenience of the reader. See United States v. Detroit Timber & Lumber Co., 200 U. S. 321, 337. SUPREME COURT OF THE UNITED STATES Syllabus LUNA TORRES v. LYNCH, ATTORNEY GENERAL CERTIORARI TO THE UNITED STATES COURT OF APPEALS FOR THE SECOND CIRCUIT No. 14–1096. Argued November 3, 2015—Decided May 19, 2016 Any alien convicted of an “aggravated felony” after entering the United States is deportable, ineligible for several forms of discretionary re- lief, and subject to expedited removal. 8 U. S. C. §§1227(a)(2)(A)(iii), (3). An “aggravated felony” is defined as any of numerous offenses listed in §1101(a)(43), each of which is typically identified either as an offense “described in” a specific federal statute or by a generic la- bel (e.g., “murder”). Section 1101(a)(43)’s penultimate sentence states that each enumerated crime is an aggravated felony irrespec- tive of whether it violates federal, state, or foreign law. Petitioner Jorge Luna Torres (Luna), a lawful permanent resident, pleaded guilty in a New York court to attempted third-degree arson. When immigration officials discovered his conviction, they initiated removal proceedings. The Immigration Judge determined that Luna’s arson conviction was for an “aggravated felony” and held that Luna was therefore ineligible for discretionary relief. -

Case Closed (Surrealistic Horror Story) a Couple of Friends Are Hanging Outside for a Picnic. They Keep Roaming in the Road on A
Case Closed (Surrealistic Horror Story) A couple of friends are hanging outside for a picnic. They keep roaming in the road on a shinny day. They come to find a haunted house and decided to explore it. The house is filled with dust and dirt is almost about to break up. Nevertheless they decided to go in and take a break before proceeding ahead. After exploring the house, friends get hungry and sit down in a room to have lunch. They realized they are out of food and decided to bring some foods while one girl stayed inside as she was getting headache and takes a nap while others go out. She sleeps for many hours (time lapse) and wakes up at night. She noticed no one around in the haunted house and starts to panic and decide to open every door looking for others but ended up going to the same place all the time. Then she tries to take a call for her friends with her smart phone but realize there are no signals in the smart phone. Then she hears an old cartoon laughing sound somewhere in the house and follows that room. She pokes in and shocks seeing a little girl watching a black and white TV. The place implies 70‟s year old vintage environment. The TV, clothes the little girl is wearing, foods all of them were object of 70 year. She gets closer and tries to touch her but realize the girl is unaware of her presence and could not feel as she continues watching the cartoon while laughing miserably. -

Sailor Mars Meet Maroku
sailor mars meet maroku By GIRNESS Submitted: August 11, 2005 Updated: August 11, 2005 sailor mars and maroku meet during a battle then fall in love they start to go futher and futher into their relationship boy will sango be mad when she comes back =:) hope you like it Provided by Fanart Central. http://www.fanart-central.net/stories/user/GIRNESS/18890/sailor-mars-meet-maroku Chapter 1 - sango leaves 2 Chapter 2 - sango leaves 15 1 - sango leaves Fanart Central A.whitelink { COLOR: #0000ff}A.whitelink:hover { BACKGROUND-COLOR: transparent}A.whitelink:visited { COLOR: #0000ff}A.BoxTitleLink { COLOR: #000; TEXT-DECORATION: underline}A.BoxTitleLink:hover { COLOR: #465584; TEXT-DECORATION: underline}A.BoxTitleLink:visited { COLOR: #000; TEXT-DECORATION: underline}A.normal { COLOR: blue}A.normal:hover { BACKGROUND-COLOR: transparent}A.normal:visited { COLOR: #000020}A { COLOR: #0000dd}A:hover { COLOR: #cc0000}A:visited { COLOR: #000020}A.onlineMemberLinkHelper { COLOR: #ff0000}A.onlineMemberLinkHelper:hover { COLOR: #ffaaaa}A.onlineMemberLinkHelper:visited { COLOR: #cc0000}.BoxTitleColor { COLOR: #000000} picture name Description Keywords All Anime/Manga (0)Books (258)Cartoons (428)Comics (555)Fantasy (474)Furries (0)Games (64)Misc (176)Movies (435)Original (0)Paintings (197)Real People (752)Tutorials (0)TV (169) Add Story Title: Description: Keywords: Category: Anime/Manga +.hack // Legend of Twilight's Bracelet +Aura +Balmung +Crossovers +Hotaru +Komiyan III +Mireille +Original .hack Characters +Reina +Reki +Shugo +.hack // Sign +Mimiru -

Csr Frequently Asked Questions
CSR FREQUENTLY ASKED QUESTIONS JULY 2012 LIST OF NEW QUESTIONS Chap 4, Sec. 4.4, Question 2 Page 14 Chap 5, Sec. 5.4, Question 1 Page 16 Chap 6, Sec. 6.4, Question 12 Page 29 Chap 6, Sec. 6.4, Question 13 Pages 30-31 Chap 6, Sec. 6.4, Question 14 Pages 31-32 Chap 8, Question 32 Pages 56-57 Table of Contents CHAPTER I – Purpose, Scope, and Effective Date ...................................................... 3 CHAPTER II – Key Definitions ..................................................................................... 3 Section 2.1 – Definition of Case .................................................................................... 3 Section 2.2 – Definition of Legal Assistance................................................................. 4 Section 2.4 – Definition of Client .................................................................................. 8 CHAPTER III – Case Management Systems ................................................................ 9 Section 3.2 – Single Recording of Cases ....................................................................... 9 Section 3.3 – Timely Closing of Cases ........................................................................ 10 Section 3.5 – Identification and De-Selection of Non-CSR Cases .............................. 12 CHAPTER IV – Reporting Requirements .................................................................. 13 Section 4.4 – Inclusion of Certain Subrecipient Cases ................................................ 13 CHAPTER V – Documentation Requirements -

2013 1St Quarter
Juan F. v. Malloy Exit Plan Quarterly Report June 2013 Juan F. v. Malloy Exit Plan Quarterly Report January 1, 2013 - March 31, 2013 Civil Action No. 2:89 CV 859 (SRU) Submitted by: DCF Court Monitor's Office 300 Church St, 4th Floor Wallingford, CT 06492 Tel: 203-741-0458 Fax: 203-741-0462 E-Mail: [email protected] Juan F. v. Malloy Exit Plan Quarterly Report June 2013 Table of Contents Juan F. v Malloy Exit Plan Quarterly Report January 1, 2013 - March 31, 2013 Section Page Highlights 3 Juan F. Exit Plan Outcome Measure Overview Chart 8 (January 1, 2013 - March 31, 2013) 9 Juan F. Pre-Certification Review-Status Update First Quarter 2013 44 Monitor's Office Case Review for Outcome Measure 3 and Outcome Measure 15 66 Juan F. Action Plan Monitoring Report Appendix 1 - Commissioner's Highlights from: The Department of 80 Children and Families Exit Plan Outcome Measures Summary Report: First Quarter Report (January 1, 2013 - March 31, 2013) 2 Juan F. v. Malloy Exit Plan Quarterly Report June 2013 Juan F. v Malloy Exit Plan Quarterly Report January 1, 2013 - March 31, 2013 Highlights • The Court Monitor's quarterly review of the Department's efforts to meet the Exit Plan Outcome Measures during the period of January 1, 2013 through March 31, 2013 indicates the Department achieved 13 of the 22 Outcome Measures. The nine measures not met include: Outcome Measure 3 (Case Planning), Outcome Measure 7 (Reunification), Outcome Measure 8 (Adoption), Outcome Measure 10 (Sibling Placements), Outcome Measure 11 (Re-Entry into DCF Custody), Outcome Measure 15 (Children's Needs Met), Outcome Measure 17 (Worker-Child Visitation In-Home)1, Outcome Measure 18 (Caseload Standards), and Outcome Measure 21 (Discharge to Adult Services). -

Salesforce Jump Start
See results from Salesforce faster than ever with Salesforce Jump Start Jump Start Maps Growth: Live Tracking Jump Start Maps Growth: Maps Jump Start Growth: Territory Planning We know you want to see value from Salesforce fast – and you want to get your Jump Start Maps Plus: Maps Advanced platform set up right the first time around. That's where the Salesforce Jump Start Jump Start Maps Plus: Territory Planning program can help. How It Works Quick and Flexible Tailored to Your Best Practices for Implementation Business Success Deploy Salesforce within Configure your end-to-end Get your team up to speed weeks by meeting with our business and processes. with guided walkthroughs, experts, who can help you And boost team efficiency as well as 30, 60, and maximize efficiency. with guidance and setup. 90-day recommendations. Ready To Learn More? Get to know more about the features, deliverable, and process of each specific Jump Start. Click your product of choice below to visit the datasheet. Sales Cloud Marketing Cloud Service Cloud Jump Start Maps Growth: Live Tracking Pardot Jump Start Maps Growth: Maps TabCRM Jump Start Growth: Territory Planning Datorama: Email Performance Jump Start Maps Plus: Maps Advanced Datorama: Media Performance Jump Start Maps Plus: Territory Planning Achieve Sales Excellence faster than ever with Sales Cloud Jump Start You’ve made a great decision to connect with your customers in a whole new way. As you prepare for launch, you probably want to hit the ground running with a quick implementation that sets up your Sales team for long-term success. -

Supsensions and Debarments
APPENDIX E SUSPENSIONS AND DEBARMENTS Th is appendix presents a comprehensive list of suspensions and debarments related to Iraq reconstruction contracts or Army support contracts in Iraq and Kuwait. ◆ Table E.1 Suspensions and Debarments (Army) Suspension and Reason for Name Position Debarment Action Taken Action Case Status Awarded contract to KBR subcontractor under Suspended, 9/17/2005; LOGCAP III contract in exchange for 20% kickback Employee, proposed for debarment, Bribery of Government Powell, Glenn Allen of contract price. Employer unaware of actions. On LOGCAP Contractor 12/13/2005; debarred, Offi cial 8/19/2005, pled guilty to a two-count criminal informa- 2/16/2006 tion charging him with fraud. Case closed. Suspended, 7/25/2005; LOGCAP proposed for debarment, Allegations of Failure Failure to perform a contract for the delivery of ice to DXB International Subcontractor 7/25/2005; debarred, To Perform a Contract Army troops in Iraq. Case closed. 9/29/2005 Suspended, 7/25/2005; SDO determined that debarment was not appropriate Employee, DXB Allegations of Failure Name Withheld proposed for debarment, based on lack of substantiation of allegations. Case International To Perform a Contract 7/25/2005 closed. Suspended, 7/25/2005; Employee, DXB proposed for debarment, Allegations of Failure Failure to perform a contract for the delivery of ice to Ludwig, Steven International 7/25/2005; debarred, To Perform a Contract Army troops in Iraq. Case closed. 9/29/2005 Provided payments to Army fi nance offi ce personnel Proposed for debarment, Jasmine at Camp Arifjan, Kuwait, for expedition of payments Contractor, Area 2/27/2006; debarred, International Bribery of Government due on Army contracts. -

Copy of Anime Licensing Information
Title Owner Rating Length ANN .hack//G.U. Trilogy Bandai 13UP Movie 7.58655 .hack//Legend of the Twilight Bandai 13UP 12 ep. 6.43177 .hack//ROOTS Bandai 13UP 26 ep. 6.60439 .hack//SIGN Bandai 13UP 26 ep. 6.9994 0091 Funimation TVMA 10 Tokyo Warriors MediaBlasters 13UP 6 ep. 5.03647 2009 Lost Memories ADV R 2009 Lost Memories/Yesterday ADV R 3 x 3 Eyes Geneon 16UP 801 TTS Airbats ADV 15UP A Tree of Palme ADV TV14 Movie 6.72217 Abarashi Family ADV MA AD Police (TV) ADV 15UP AD Police Files Animeigo 17UP Adventures of the MiniGoddess Geneon 13UP 48 ep/7min each 6.48196 Afro Samurai Funimation TVMA Afro Samurai: Resurrection Funimation TVMA Agent Aika Central Park Media 16UP Ah! My Buddha MediaBlasters 13UP 13 ep. 6.28279 Ah! My Goddess Geneon 13UP 5 ep. 7.52072 Ah! My Goddess MediaBlasters 13UP 26 ep. 7.58773 Ah! My Goddess 2: Flights of Fancy Funimation TVPG 24 ep. 7.76708 Ai Yori Aoshi Geneon 13UP 24 ep. 7.25091 Ai Yori Aoshi ~Enishi~ Geneon 13UP 13 ep. 7.14424 Aika R16 Virgin Mission Bandai 16UP Air Funimation 14UP Movie 7.4069 Air Funimation TV14 13 ep. 7.99849 Air Gear Funimation TVMA Akira Geneon R Alien Nine Central Park Media 13UP 4 ep. 6.85277 All Purpose Cultural Cat Girl Nuku Nuku Dash! ADV 15UP All Purpose Cultural Cat Girl Nuku Nuku TV ADV 12UP 14 ep. 6.23837 Amon Saga Manga Video NA Angel Links Bandai 13UP 13 ep. 5.91024 Angel Sanctuary Central Park Media 16UP Angel Tales Bandai 13UP 14 ep. -

Read Book Case Closed: Vol.40 Pdf Free Download
CASE CLOSED: VOL.40 PDF, EPUB, EBOOK Gosho Aoyama | 184 pages | 10 Nov 2011 | Viz Media, Subs. of Shogakukan Inc | 9781421535005 | English | San Francisco, United States Case Closed: Vol.40 PDF Book Donate Today. Retrieved November 19, Retrieved October 10, Retrieved February 21, Pickup not available. Please Save My Earth. I agree to the Terms and Conditions. Viz Media. This new model will increase opportunities for the community to contribute to ;login: and engage with its content. Gosho Aoyama. By Gosho Aoyama. But to find her, they'll have to crack a numerical code that takes them on a wild goose chase through the local zoo! Magic Kaito Episodes. December 25, []. We aim to show you accurate product information. Chingwin Publishing Group. December 24, []. Related Searches. Rik Farrow, the current editor of the magazine, will continue to provide leadership for the overall content offered in ;login: , which will be released via our website on a regular basis throughout the year. Retrieved October 20, You may block cookies via standard web-browser settings, but this site may not function correctly without cookies. August 18, []. Episode list 1 Season 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Episode list 2 Season 16 17 18 19 20 21 22 23 24 25 26 27 28 29 OVAs Lupin the 3rd vs. Recent searches Clear All. You have been sent an email with instructions on how to reset your password. Book Depository. December 10, [42] Egmont licensed series in Sweden , Norway , Finland and Denmark , but dropped them either because low sales Sweden , [16] unknown reason Denmark and Norway [17] [18] or when Egmont closed its manga-publishing division in Finland.