Vascular Complications After Radiosurgery for Meningiomas
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
INTRODUCTION Time, Are Discussed in Full, for Without Accurate
Br J Ophthalmol: first published as 10.1136/bjo.31.Suppl.7 on 1 January 1947. Downloaded from INTRODUCTION This is a contribution to the study of vertical defects in the positions of the eyes. It includes a partial survey of the literature and an analysis of a series of 402 patients with horizontal and vertical defects of the concomitant and paralytic types. Methods of investigation, including two that are described for the first time, are discussed in full, for without accurate observations satis- factory treatment is unlikely. The value of the " division " of diplopia is stressed. There are many types of ocular vertical deviations. Their recog- nition is not always easy nor is their interpretation always simple. They must be studied in near and distant vision as well as when the gaze is directed obliquely. Any deviation may depend on the following: 1. The position of ocular rest. 2. The degree of fusion permitting true or alternating hyperphoria. 3. The presence of a paralysed muscle and its stage of recovery. 4. Contraction of antagonist and synergist and inhibitional paresis. 5. The fascial check ligaments restricting ocular rotation. 6. " Abnormal excitations of the centres controlling the non- copyright. parallel movements." Bielschowsky (August, 1938). These will now be considered at length. Position of Ocular Rest.-A vertical angle gamma is a very rare finding. It occurs when the visual line connecting the fovea passes above or below the geometrical axis. This is revealed by a study of the corneal reflexes. Many observers have been tempted to seek the so-called position of rest by withdrawing the bond of fusion. -

Multiple Intracerebral Hemorrhages in an Old Patient with Rheumatoid Arthritis
Multiple Intracerebral Hemorrhages in an Old Patient with Rheumatoid Arthritis INIMIOARA MIHAELA COJOCARU1, 2, V. ŞTEFĂNESCU2, DANIELA TRAŞCĂ2, ADELINA ŞERBAN-PEREŢEANU2, B. CHICOŞ3, M. COJOCARU3,4 1“Carol Davila” University of Medicine and Pharmacy, Bucharest 2Department of Neurology, “Colentina” Clinical Hospital 3“Dr. Ion Stoia” Clinical Center for Rheumatic Diseases 4“Titu Maiorescu” University, Faculty of Medicine, Bucharest, Romania A 78-year-old Caucasian man was admitted in the Department of Neurology for visual disturbances, started two days before. The next day the patient experienced headache, fever and gait disturbances. He had hypertension, diabetes mellitus, an ischemic stroke 13 years ago, longstanding seronegative rheumatoid arthritis (17 years), polynodular goiter, right ischio-pubian fracture and right femoral vein thrombosis a year ago due to a car accident, since he is treated with oral anticoagulants associated to antiaggregant, hypotensors, statin and oral antidiabetics. The neurologic examination had evidenced nuchal rigidity, left homonymous hemianopsia, left central facial palsy, ataxia of the inferior limbs with wide-based gait, achilean reflexes abolished bilaterally, bilaterally abolished plantar reflexes, ideomotor apraxia, dysarthria, hypoprosexia, and preserved consciousness patient. A non-contrast cerebral CT scan had shown right temporal and parieto-occipital intraparenchymatous hemorrhages, a right frontal sequelar lesion, multiple old lacunar infarcts, cortical atrophy. Laboratory findings included an inflammatory syndrome, absence of rheumatoid arthritis positive serology, normal coagulogram, an elevated proteinuria. The cerebral IRM performed on the seventh day of hospitalisation was suggestive for subacute right parietal hemorrhage, old cerebral infarction in the right anterior cerebral artery area, old lacunar infarcts and cerebral atrophy. The anticoagulant and antiaggregant treatment was stopped after a generalized tonic-clonic seizure occurred. -

Facial Nerve Electrodiagnostics for Patients with Facial Palsy: a Clinical Practice Guideline
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Helsingin yliopiston digitaalinen arkisto European Archives of Oto-Rhino-Laryngology (2020) 277:1855–1874 https://doi.org/10.1007/s00405-020-05949-1 REVIEW ARTICLE Facial nerve electrodiagnostics for patients with facial palsy: a clinical practice guideline Orlando Guntinas‑Lichius1,2,3 · Gerd Fabian Volk1,2 · Kerry D. Olsen4 · Antti A. Mäkitie5 · Carl E. Silver6 · Mark E. Zafereo7 · Alessandra Rinaldo8 · Gregory W. Randolph9 · Ricard Simo10 · Ashok R. Shaha11 · Vincent Vander Poorten3,12 · Alfo Ferlito13 Received: 14 March 2020 / Accepted: 27 March 2020 / Published online: 8 April 2020 © The Author(s) 2020 Abstract Purpose Facial nerve electrodiagnostics is a well-established and important tool for decision making in patients with facial nerve diseases. Nevertheless, many otorhinolaryngologist—head and neck surgeons do not routinely use facial nerve electro- diagnostics. This may be due to a current lack of agreement on methodology, interpretation, validity, and clinical application. Electrophysiological analyses of the facial nerve and the mimic muscles can assist in diagnosis, assess the lesion severity, and aid in decision making. With acute facial palsy, it is a valuable tool for predicting recovery. Methods This paper presents a guideline prepared by members of the International Head and Neck Scientifc Group and of the Multidisciplinary Salivary Gland Society for use in cases of peripheral facial nerve disorders based on a systematic literature search. Results Required equipment, practical implementation, and interpretation of the results of facial nerve electrodiagnostics are presented. Conclusion The aim of this guideline is to inform all involved parties (i.e. -

Cranial Nerves 1, 5, 7-12
Cranial Nerve I Olfactory Nerve Nerve fiber modality: Special sensory afferent Cranial Nerves 1, 5, 7-12 Function: Olfaction Remarkable features: – Peripheral processes act as sensory receptors (the other special sensory nerves have separate Warren L Felton III, MD receptors) Professor and Associate Chair of Clinical – Primary afferent neurons undergo continuous Activities, Department of Neurology replacement throughout life Associate Professor of Ophthalmology – Primary afferent neurons synapse with secondary neurons in the olfactory bulb without synapsing Chair, Division of Neuro-Ophthalmology first in the thalamus (as do all other sensory VCU School of Medicine neurons) – Pathways to cortical areas are entirely ipsilateral 1 2 Crania Nerve I Cranial Nerve I Clinical Testing Pathology Anosmia, hyposmia: loss of or impaired Frequently overlooked in neurologic olfaction examination – 1% of population, 50% of population >60 years Aromatic stimulus placed under each – Note: patients with bilateral anosmia often report nostril with the other nostril occluded, eg impaired taste (ageusia, hypogeusia), though coffee, cloves, or soap taste is normal when tested Note that noxious stimuli such as Dysosmia: disordered olfaction ammonia are not used due to concomitant – Parosmia: distorted olfaction stimulation of CN V – Olfactory hallucination: presence of perceived odor in the absence of odor Quantitative clinical tests are available: • Aura preceding complex partial seizures of eg, University of Pennsylvania Smell temporal lobe origin -
Crossed Brainstem Syndrome Revealing
Beucler et al. BMC Neurology (2021) 21:204 https://doi.org/10.1186/s12883-021-02223-7 CASE REPORT Open Access Crossed brainstem syndrome revealing bleeding brainstem cavernous malformation: an illustrative case Nathan Beucler1,2* , Sébastien Boissonneau1,3, Aurélia Ruf4, Stéphane Fuentes1, Romain Carron3,5 and Henry Dufour1,6 Abstract Background: Since the nineteenth century, a great variety of crossed brainstem syndromes (CBS) have been described in the medical literature. A CBS typically combines ipsilateral cranial nerves deficits to contralateral long tracts involvement such as hemiparesis or hemianesthesia. Classical CBS seem in fact not to be so clear-cut entities with up to 20% of patients showing different or unnamed combinations of crossed symptoms. In terms of etiologies, acute brainstem infarction predominates but CBS secondary to hemorrhage, neoplasm, abscess, and demyelination have been described. The aim of this study was to assess the proportion of CBS caused by a bleeding episode arising from a brainstem cavernous malformation (BCM) reported in the literature. Case presentation: We present the case of a typical Foville syndrome in a 65-year-old man that was caused by a pontine BCM with extralesional bleeding. Following the first bleeding episode, a conservative management was decided but the patient had eventually to be operated on soon after the second bleeding event. Discussion: A literature review was conducted focusing on the five most common CBS (Benedikt, Weber, Foville, Millard-Gubler, Wallenberg) on Medline database from inception to 2020. According to the literature, hemorrhagic BCM account for approximately 7 % of CBS. Microsurgical excision may be indicated after the second bleeding episode but needs to be carefully weighted up against the risks of the surgical procedure and openly discussed with the patient. -

The Origin of Facial Palsy in Multiple Sclerosis
ISSN 2470-4059 OTOLARYNGOLOGY Open Journal PUBLISHERS Editorial The Origin of Facial Palsy in Multiple Sclerosis Arianna Di Stadio, MD, PhD1*; Evanthia Bernitsas, MD2 1Department of Neurology, San Camillo Hospital IRCCS, Venice, Italy 2Multiple Sclerosis Center, Wayne State University School of Medicine, Detroit, MI, USA *Corresponding author Arianna Di Stadio, MD, PhD Assistant Professor, Department of Neurology, San Camillo Hospital IRCCS, Venice, Italy; E-mail: [email protected] Article information Received: April 16th, 2018; Accepted: April 27th, 2018; Published: April 30th, 2018 Cite this article Di Stadio A, Bernitsas E. the origin of facial palsy in multiple sclerosis. Otolaryngol Open J. 2018; 4(1): e1-e4. doi: 10.17140/OTLOJ-4-e006 ultiple Sclerosis (MS) is an autoimmune neurodegenera- Mtive disease that affects several people especially in North Figure 1. The Image Summarizes the Facial Pathway from Periphery America and Canada. In 2013, 33 individuals over 100,000 were (Terminal Branch of Facial Nerve) to the Brain Motor Cortex Area (M1) affected from MS; the estimated increase for 5 years of observation ranged from an average of 4.7 per 100,000 in high-income coun- tries to just 0.04 per 100,000 in the low-income countries.1 Women are more affected than men (2.3-3.5:1), but in men, the disease is usually more aggressive and has a worse prog- nosis than in women.2 MS is a demyelinating disorder in which the immune system attacks the neural structures in the central nervous system (CNS)3; this mechanism is determined by a particular class of cells- Microglia- thathave been identified as responsible of the degenera- tive process. -

Noropsikiyatri 2009-4 Link
Case Report /Olgu Sunumu 197 Midbrain Infarction Presenting with Weber’s Syndrome and Central Facial Palsy: A Case Report Orta Beyin ‹nfarkt›na Ba¤l› Geliflen Weber Sendromu ve Santral Fasyal Parezi: Olgu Sunumu Demet ‹LHAN ALGIN, Figen TAfiER*, Sayime AYDIN**, Elif AKSAKALLI*** Dumlup›nar University Faculty of Medicine, Department of Neurology, Kütahya *Dumlup›nar University Faculty of Medicine, Department of Anatomy, Kütahya **Dumlup›nar University Faculty of Medicine, Department of Ophthalmology, Kütahya ***Dumlup›nar University Faculty of Medicine, Department of Physical therapy and Rehabilitation, Kütahya, Turkey ABSTRACT ÖZET Weber's syndrome is a distinctive brainstem disease characterized by ipsilateral Weber sendromu ipsilateral 3. sinir parezisi ve kontrlateral hemipleji ile karak- 3rd nerve palsy with contralateral hemiplegia and is due to an intrinsic or terize özellikli bir beyinsap› hastal›¤›d›r ve ventral orta beyindeki intrinsik veya extrinsic lesion in the ventral midbrain. To date, there is limited literature ekstrinsik lezyona ba¤l› olarak geliflir. Bugüne kadar, santral fasyal parezi ile concerning Weber's syndrome associated with central facial palsy, but none iliflkili Weber sendromu konusunda s›n›rl› say›da literatür mevcuttur, ancak hiç- was demonstrated with comprehensive explanation. We report a rare case biri kapsaml› bir aç›klama ile sunulmam›flt›r. Mesensefalonun ventromedial presented with Weber’s syndrome and central facial palsy caused by infarction krural bölgesinin infarkt›na ba¤l› geliflen Weber sendromu ve santral fasyal pa- of ventromedial crural region of the mesencephalon. rezi ile baflvuran nadir bir olgudan bahsedilmektedir. The patient was a 68-year-old woman who developed central type facial palsy on Olgu, sa¤ santral fasyal parezi, sol 3. -
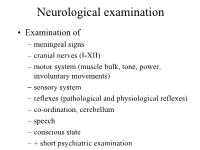
Neurological Examination
Neurological examination • Examination of – meningeal signs – cranial nerves (I-XII) – motor system (muscle bulk, tone, power, involuntary movements) – sensory system – reflexes (pathological and physiological reflexes) – co-ordination, cerebellum – speech – conscious state – + short psychiatric examination MENINGEAL SIGNS • may be caused by: – meningitis (bacterial or viral infection of meninges) – blood in the subarachnoidal space – infiltration of meninges by carcinoma cells – increased intracranial pressure – dehydration Optic nerve (II) Visual acuity Visual field Fundus - Optic disc • Retina • Optic nerve • Chiasm • Optic tract • Lateral geniculate body • Optic radiation • Visual (occipital) cortex VISUAL FIELD - LENS - reversed image 1. The lens produces reversed image 2. Fibers, originating from the upper part of the retina keeps their superior/upper position through the whole optic pathway Visual field Oculomotor (III), trochlear (IV), and abducent (VI) nerves • Oculomotor nerve (III) innervates: medial rectus, superior rectus, inferior rectus, inferior oblique muscles + superior palpebral levator muscle, ciliary muscle, pupillary constrictor muscle • Trochlear nerve (IV) innervates: superior oblique muscle • Abducent nerve (VI) innervates: lateral rectus muscle Nuclei of culomotor (III), trochlear (IV), and abducent (VI) nerves • Oculomotor nerve – Main nucleus (mesencephalon) of oculomotor nerve controls medial rectus, superior rectus, inferior rectus, inferior oblique muscles + superior palpebral levator muscle – Edinger-Westphal -

The Tick Did It, Twice! Alina Reznik, OD Optometry Resident Lynn Community Health Center
The Tick Did It, Twice! Alina Reznik, OD Optometry Resident Lynn Community Health Center Abstract: A tick bite leads a 36-year-old male to Optometry due to bilateral lagophthalmos secondary to bilateral seventh nerve facial weakness. Lyme disease necessitates early detection, diagnosis, along with systemic and ocular treatment to accelerate patient recovery. I. Case History A 36-year-old Hispanic male, referred by primary care, presented for a problem focused exam. Never had an eye exam. Patient reported symptoms of burning, dryness and tearing in both eyes secondarily to the inability to close his eyes, right >left. He also reported new onset severe headaches along with changes in his face for the past week. Patient reported that he “cannot close his eyes.” Patient works in landscaping and reported pulling 2 ticks off his back a few weeks ago. No history of trauma, no other remarkable systemic, medical, ocular or family history. II. Pertinent findings External exam was positive for lagophthalmos OD>OS. On slit lamp exam, patient had 1+scurfs, 1+ capped glands, 2+ diffuse corneal superficial punctate keratitis with accumulation inferiorly (right>left), open anterior chamber with no cells and flare OU. Fundus examination was normal with no posterior inflammation or abnormalities. Patient had no external skin rashes, no vesicles on face and body. Neurological examination: (Will include patient facial photos from all three encounters showing neurological improvement with time and treatment) -Initial encounter: Patient was incapable of fully shutting his eyes. Palpebral fissure size while shutting eyes: OD 9mm, OS 4mm. Absence of forehead winkles above both eyes Show me your teeth? Unable to show teeth, nor move the superior or inferior facial muscles. -

Di Erentiating Facial Weakness Caused by Bell's Palsy Vs. Acute
Dierentiating Facial Weakness Caused by Bell’s Palsy vs. Acute Stroke Can you tell the dierence? Wed, May 7, 2014 By Caitlin Loomis, MD [Caitlin Loomis, MD] , Michael T. Mullen, MD [Michael T. Mullen, MD] Is it Bell's palsy or an acute stroke? Photo Edward T. Dickinson Learning Objectives Learn the basic anatomy of facial muscle control. Recognize the common clinical presentation of Bell’s palsy and ischemic stroke. Understand how to rapidly assess a patient with acute facial weakness to dierentiate between Bell’s palsy and ischemic stroke. You’re responding to a 54-year-old woman with facial weakness. The patient states she looked in the mirror this morning and noticed her face appeared “twisted.” She didn’t notice any facial asymmetry before going to bed the night before. She complains of no pain or numbness. Your assessment shows the right side of her mouth isn’t able to smile and she has diculty closing her right eye. You perform a neurologic exam; strength and sensation are normal throughout, with no weakness in the arms or legs and no other neurologic ndings. She’s able to communicate and answers all questions appropriately. Is this a stroke? Facial Weakness The two most common causes of acute facial paralysis are Bell’s palsy and ischemic stroke.1 EMS providers are often faced with the challenge of dierentiating between these two diagnoses. Because acute stroke is a time-critical illness, the distinction between stroke and Bell’s palsy must be made quickly to avoid unnecessary delays in treatment. Anatomy of Facial Muscle Control Two facial nerves, the right and the left, control all of the muscles in the face. -

Culprit of Facial Nerve Palsy
Original article Emerg Med J: first published as 10.1136/emermed-2019-208691 on 22 October 2019. Downloaded from Image CHALLENGE Culprit of facial nerve palsy CLINICAL INTRODUCTION A female patient aged 78 years with a medical history of hyper- tension, type 2 diabetes and dyslipidemia, presented with right otalgia. At her first consultation, amoxicillin and clavulanic acid and topical ofloxacin were prescribed after the suggestion of a bacterial infection process, but without improvement of the symptoms. She arrived at our ED 3 days later with an acute onset of impaired facial expression and ocular pain. On physical exam- ination, she was noted to have right conjunctival hyperemia, right-sided facial nerve palsy (VI degree on the House-Brack- mann scale) (figure 1) and a vesicular rash on the ipsilateral ear. The remaining neurological examination was normal. QUESTION What is the most likely cause for facial nerve palsy? A. Bell’s palsy Figure 1 Right-sided facial nerve palsy. copyright. B. Acoustic neuroma C. Ramsay Hunt syndrome (RHS) D. Stroke For answer see page 683 http://emj.bmj.com/ on November 8, 2019 by Anne Meneghetti. Protected Becker TK, et al. Emerg Med J 2019;36:660–665. doi:10.1136/emermed-2018-208234 665 Original article Emerg Med J: first published as 10.1136/emermed-2019-208691 on 22 October 2019. Downloaded from Image CHALLENGE Culprit of facial nerve palsy For question see page 665 ANSWER: C Initially, clinicians should focus on determining whether the patient has a peripheral or central cause for the facial nerve palsy.1 A central facial palsy due to a stroke spares the forehead. -
Sparing the Face
CORE Metadata, citation and similar papers at core.ac.uk Provided by RERO DOC Digital Library J Neurol (2009) 256:1017–1018 DOI 10.1007/s00415-009-5041-6 LETTER TO THE EDITORS Sixth cranial nerve palsy and contralateral hemiparesis (Raymond’s syndrome) sparing the face P. Me´gevand Æ B. Pilly Æ J. Delavelle Æ N. Tajouri Æ A. B. Safran Æ T. Landis Æ C. Lu¨scher Received: 4 August 2008 / Revised: 6 January 2009 / Accepted: 28 January 2009 / Published online: 1 March 2009 Ó Springer-Verlag 2009 The combination of VIth cranial (abducens) nerve palsy normal. Deep tendon reflexes were normal and symmetric. and contralateral hemiplegia is termed Raymond’s syn- Cutaneous plantar response was flexor on both sides. There drome [1–3]. Whether this rarely reported syndrome [4] was no ataxia or sensory deficit. Gait was unremarkable. necessarily includes central facial paralysis is debated [5]. Laboratory examinations were normal except for slightly raised liver enzymes. Magnetic resonance imaging, performed 2 days after the onset of symptoms, showed a Case report lesion in the left caudal ventral paramedian pons (Fig. 1a, b). Magnetic resonance angiography as well as extra- and A 74-year old man presented with horizontal diplopia of intracranial ultrasound with Doppler examination did not sudden onset, worsened by directing gaze to the left. His reveal any hemodynamically significant arterial stenosis. past medical history included arterial hypertension treated Heart rhythm remained regular during 24-h monitoring in with an angiotensin conversion enzyme inhibitor, a 60- the stroke unit. pack-per-year smoking history and moderate alcohol The patient was not handicapped by the slight hemipa- consumption.