Identification of FHL1 As a Regulator of Skeletal Muscle
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Role of IL-1 in Adipose Browning and Muscle Wasting in CKD-Associated Cachexia
bioRxiv preprint doi: https://doi.org/10.1101/2021.02.05.429984; this version posted February 7, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. The role of IL-1 in adipose browning and muscle wasting in CKD-associated cachexia Wai W Cheung1*, Ronghao Zheng2*, Sheng Hao3, Zhen Wang4, Alex Gonzalez1, Ping Zhou5, Hal M Hoffman6, Robert H Mak1 1 Pediatric Nephrology, Rady Children’s Hospital San Diego, University of California, San Diego, USA 2 Department of Pediatric Nephrology, Rheumatology, and Immunology, Maternal and Child Health Hospital of Hubei Province, TongJi Medical College, Huazhong University of Science and Technology, Wuhan, China 3Department of Nephrology and Rheumatology, Shanghai Children’s Hospital, Shanghai Jiao Tong University, Shanghai, China 4Department of Pediatrics, Shanghai General Hospital, Shanghai Jiao Tong University, Shanghai, China 5 Department of Pediatrics, the Second Affiliated Hospital of Harbin Medical University, Harbin, China 6 Department of Pediatrics, University of California, San Diego, USA * These authors contributed equally to this work. Correspondence: Robert H Mak Division of Pediatric Nephrology Rady Children’s Hospital University of California, San Diego 9500 Gilman Drive, MC0831, La Jolla, California 92093-0831, USA P: 858-822-6717 F: 858-822-6776 E-mail: [email protected] Running title: Anakinra attenuates uremic cachexia bioRxiv preprint doi: https://doi.org/10.1101/2021.02.05.429984; this version posted February 7, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. -

Single-Cell RNA Sequencing Demonstrates the Molecular and Cellular Reprogramming of Metastatic Lung Adenocarcinoma
ARTICLE https://doi.org/10.1038/s41467-020-16164-1 OPEN Single-cell RNA sequencing demonstrates the molecular and cellular reprogramming of metastatic lung adenocarcinoma Nayoung Kim 1,2,3,13, Hong Kwan Kim4,13, Kyungjong Lee 5,13, Yourae Hong 1,6, Jong Ho Cho4, Jung Won Choi7, Jung-Il Lee7, Yeon-Lim Suh8,BoMiKu9, Hye Hyeon Eum 1,2,3, Soyean Choi 1, Yoon-La Choi6,10,11, Je-Gun Joung1, Woong-Yang Park 1,2,6, Hyun Ae Jung12, Jong-Mu Sun12, Se-Hoon Lee12, ✉ ✉ Jin Seok Ahn12, Keunchil Park12, Myung-Ju Ahn 12 & Hae-Ock Lee 1,2,3,6 1234567890():,; Advanced metastatic cancer poses utmost clinical challenges and may present molecular and cellular features distinct from an early-stage cancer. Herein, we present single-cell tran- scriptome profiling of metastatic lung adenocarcinoma, the most prevalent histological lung cancer type diagnosed at stage IV in over 40% of all cases. From 208,506 cells populating the normal tissues or early to metastatic stage cancer in 44 patients, we identify a cancer cell subtype deviating from the normal differentiation trajectory and dominating the metastatic stage. In all stages, the stromal and immune cell dynamics reveal ontological and functional changes that create a pro-tumoral and immunosuppressive microenvironment. Normal resident myeloid cell populations are gradually replaced with monocyte-derived macrophages and dendritic cells, along with T-cell exhaustion. This extensive single-cell analysis enhances our understanding of molecular and cellular dynamics in metastatic lung cancer and reveals potential diagnostic and therapeutic targets in cancer-microenvironment interactions. 1 Samsung Genome Institute, Samsung Medical Center, Seoul 06351, Korea. -
LSD1 Dual Function in Mediating Epigenetic Corruption of the Vitamin
Battaglia et al. Clinical Epigenetics (2017) 9:82 DOI 10.1186/s13148-017-0382-y RESEARCH Open Access LSD1 dual function in mediating epigenetic corruption of the vitamin D signaling in prostate cancer Sebastiano Battaglia1*, Ellen Karasik2, Bryan Gillard2, Jennifer Williams2, Trisha Winchester3, Michael T. Moser2, Dominic J Smiraglia3 and Barbara A. Foster2* Abstract Background: Lysine-specific demethylase 1A (LSD1) is a key regulator of the androgen (AR) and estrogen receptors (ER), and LSD1 levels correlate with tumor aggressiveness. Here, we demonstrate that LSD1 regulates vitamin D receptor (VDR) activity and is a mediator of 1,25(OH)2-D3 (vitamin D) action in prostate cancer (PCa). Methods: Athymic nude mice were xenografted with CWR22 cells and monitored weekly after testosterone pellet removal. Expression of LSD1 and VDR (IHC) were correlated with tumor growth using log-rank test. TRAMP tumors and prostates from wild-type (WT) mice were used to evaluate VDR and LSD1 expression via IHC and western blotting. The presence of VDR and LSD1 in the same transcriptional complex was evaluated via immunoprecipitation (IP) using nuclear cell lysate. The effect of LSD1 and 1,25(OH)2-D3 on cell viability was evaluated in C4-2 and BC1A cells via trypanblueexclusion.TheroleofLSD1inVDR-mediatedgenetranscriptionwasevaluatedforCdkn1a, E2f1, Cyp24a1,andS100g via qRT-PCR-TaqMan and via chromatin immunoprecipitation assay. Methylation of Cdkn1a TSS was measured via bisulfite sequencing, and methylation of a panel of cancer-related genes was quantified using methyl arrays. The Cancer Genome Atlas data were retrieved to identify genes whose status correlates with LSD1 and DNA methyltransferase 1 (DNMT1). -

Placental Transcriptome Adaptations to Maternal Nutrient Restriction in Sheep
International Journal of Molecular Sciences Article Placental Transcriptome Adaptations to Maternal Nutrient Restriction in Sheep Chelsie B. Steinhauser 1,†, Colleen A. Lambo 2,†, Katharine Askelson 1, Gregory W. Burns 3, Susanta K. Behura 4,5, Thomas E. Spencer 4, Fuller W. Bazer 1 and Michael Carey Satterfield 1,* 1 Department of Animal Science, Texas A & M University, College Station, TX 77843, USA; [email protected] (C.B.S.); [email protected] (K.A.); [email protected] (F.W.B.) 2 Department of Veterinary Physiology and Pharmacology, Texas A & M University, College Station, TX 77843, USA; [email protected] 3 Department of Obstetrics, Gynecology and Reproductive Biology, Michigan State University, Grand Rapids, MI 49503, USA; [email protected] 4 Division of Animal Sciences, University of Missouri, Columbia, MO 65211, USA; [email protected] (S.K.B.); [email protected] (T.E.S.) 5 Institute for Data Science and Informatics, University of Missouri, Columbia, MO 65211, USA * Correspondence: csatterfi[email protected]; Tel.: +1-979-845-6448 † These authors contributed equally to this work. Abstract: Placental development is modified in response to maternal nutrient restriction (NR), resulting in a spectrum of fetal growth rates. Pregnant sheep carrying singleton fetuses and fed either 100% (n = 8) or 50% (NR; n = 28) of their National Research Council (NRC) recommended intake from days 35–135 of pregnancy were used to elucidate placentome transcriptome alterations at both Citation: Steinhauser, C.B.; Lambo, day 70 and day 135. NR fetuses were further designated into upper (NR NonSGA; n = 7) and lower C.A.; Askelson, K.; Burns, G.W.; quartiles (NR SGA; n = 7) based on day 135 fetal weight. -
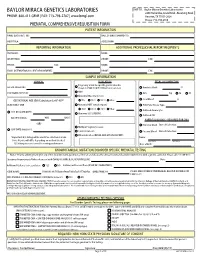
Prenatal Testing Requisition Form
BAYLOR MIRACA GENETICS LABORATORIES SHIP TO: Baylor Miraca Genetics Laboratories 2450 Holcombe, Grand Blvd. -Receiving Dock PHONE: 800-411-GENE | FAX: 713-798-2787 | www.bmgl.com Houston, TX 77021-2024 Phone: 713-798-6555 PRENATAL COMPREHENSIVE REQUISITION FORM PATIENT INFORMATION NAME (LAST,FIRST, MI): DATE OF BIRTH (MM/DD/YY): HOSPITAL#: ACCESSION#: REPORTING INFORMATION ADDITIONAL PROFESSIONAL REPORT RECIPIENTS PHYSICIAN: NAME: INSTITUTION: PHONE: FAX: PHONE: FAX: NAME: EMAIL (INTERNATIONAL CLIENT REQUIREMENT): PHONE: FAX: SAMPLE INFORMATION CLINICAL INDICATION FETAL SPECIMEN TYPE Pregnancy at risk for specific genetic disorder DATE OF COLLECTION: (Complete FAMILIAL MUTATION information below) Amniotic Fluid: cc AMA PERFORMING PHYSICIAN: CVS: mg TA TC Abnormal Maternal Screen: Fetal Blood: cc GESTATIONAL AGE (GA) Calculation for AF-AFP* NTD TRI 21 TRI 18 Other: SELECT ONLY ONE: Abnormal NIPT (attach report): POC/Fetal Tissue, Type: TRI 21 TRI 13 TRI 18 Other: Cultured Amniocytes U/S DATE (MM/DD/YY): Abnormal U/S (SPECIFY): Cultured CVS GA ON U/S DATE: WKS DAYS PARENTAL BLOODS - REQUIRED FOR CMA -OR- Maternal Blood Date of Collection: Multiple Pregnancy Losses LMP DATE (MM/DD/YY): Parental Concern Paternal Blood Date of Collection: Other Indication (DETAIL AND ATTACH REPORT): *Important: U/S dating will be used if no selection is made. Name: Note: Results will differ depending on method checked. Last Name First Name U/S dating increases overall screening performance. Date of Birth: KNOWN FAMILIAL MUTATION/DISORDER SPECIFIC PRENATAL TESTING Notice: Prior to ordering testing for any of the disorders listed, you must call the lab and discuss the clinical history and sample requirements with a genetic counselor. -
![[Thesis Title Goes Here]](https://docslib.b-cdn.net/cover/4522/thesis-title-goes-here-1504522.webp)
[Thesis Title Goes Here]
Understanding Pathways Regulating Liver versus Pancreas Fate Decision and beta-cell Regeneration A Dissertation Presented to The Academic Faculty by Jin Xu In Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in Biology in the School of Biological Sciences Georgia Institute of Technology August 2017 Copyright © 2017 by Jin Xu Understanding Pathways Regulating Liver versus Pancreas Fate Decision and beta-cell Regeneration Approved by: Dr. Chong Shin, Advisor Dr. Francesca Storici School of Biological Sciences School of Biological Sciences Georgia Institute of Technology Georgia Institute of Technology Dr. Alfred Merrill Dr. Yury Chernoff School of Biological Sciences School of Biological Sciences Georgia Institute of Technology Georgia Institute of Technology Dr. Young Jang School of Biological Sciences Georgia Institute of Technology Date Approved: July 17, 2017 ACKNOWLEDGEMENTS I would like to extend my deepest gratitude to my advisor Dr. Chong Shin for her invaluable guidance. My success would not have been possible without the continuous support and nurturing of her. I am also grateful to my committee members, Dr. Francesca Storici, Dr. Alfred Merrill, Dr. Yury Chernoff, and Dr. Young Jang for their insightful questions and discussions on my thesis proposal and for reviewing this dissertation. I also wish to thank my parents and my friends for their unconditional support and love. iv TABLE OF CONTENTS ACKNOWLEDGEMENTS .............................................................................................. -

Bioinformatics Analysis to Screen Key Genes in Papillary Thyroid Carcinoma
ONCOLOGY LETTERS 19: 195-204, 2020 Bioinformatics analysis to screen key genes in papillary thyroid carcinoma YUANHU LIU1*, SHUWEI GAO2*, YAQIONG JIN2, YERAN YANG2, JUN TAI1, SHENGCAI WANG1, HUI YANG2, PING CHU2, SHUJING HAN2, JIE LU2, XIN NI1,2, YONGBO YU2 and YONGLI GUO2 1Department of Otolaryngology, Head and Neck Surgery, Beijing Children's Hospital, Capital Medical University, National Center for Children's Health; 2Beijing Key Laboratory for Pediatric Diseases of Otolaryngology, Head and Neck Surgery, MOE Key Laboratory of Major Diseases in Children, Beijing Pediatric Research Institute, Beijing Children's Hospital, Capital Medical University, National Center for Children's Health, Beijing 100045, P.R. China Received April 22, 2019; Accepted September 24, 2019 DOI: 10.3892/ol.2019.11100 Abstract. Papillary thyroid carcinoma (PTC) is the most verifying their potential for clinical diagnosis. Taken together, common type of thyroid carcinoma, and its incidence has the findings of the present study suggest that these genes and been on the increase in recent years. However, the molecular related pathways are involved in key events of PTC progression mechanism of PTC is unclear and misdiagnosis remains a and facilitate the identification of prognostic biomarkers. major issue. Therefore, the present study aimed to investigate this mechanism, and to identify key prognostic biomarkers. Introduction Integrated analysis was used to explore differentially expressed genes (DEGs) between PTC and healthy thyroid tissue. To Thyroid carcinoma is the most common malignancy of investigate the functions and pathways associated with DEGs, the head and neck, and accounts for 91.5% of all endocrine Gene Ontology, pathway and protein-protein interaction (PPI) malignancies (1). -

Proteomic Identification of FHL1 As the Protein Mutated in Human Reducing Body Myopathy
Proteomic identification of FHL1 as the protein mutated in human reducing body myopathy Joachim Schessl, … , Christina A. Mitchell, Carsten G. Bönnemann J Clin Invest. 2008;118(3):904-912. https://doi.org/10.1172/JCI34450. Research Article Genetics Reducing body myopathy (RBM) is a rare disorder causing progressive muscular weakness characterized by aggresome- like inclusions in the myofibrils. Identification of genes responsible for RBM by traditional genetic approaches has been impossible due to the frequently sporadic occurrence in affected patients and small family sizes. As an alternative approach to gene identification, we used laser microdissection of intracytoplasmic inclusions identified in patient muscle biopsies, followed by nanoflow liquid chromatography–tandem mass spectrometry and proteomic analysis. The most prominent component of the inclusions was the Xq26.3-encoded four and a half LIM domain 1 (FHL1) protein, expressed predominantly in skeletal but also in cardiac muscle. Mutational analysis identified 4 FHL1 mutations in 2 sporadic unrelated females and in 2 families with severely affected boys and less-affected mothers. Transfection of kidney COS-7 and skeletal muscle C2C12 cells with mutant FHL1 induced the formation of aggresome-like inclusions that incorporated both mutant and wild-type FHL1 and trapped other proteins in a dominant-negative manner. Thus, a novel laser microdissection/proteomics approach has helped identify both inherited and de novo mutations in FHL1, thereby defining a new X-linked protein aggregation disorder of muscle. Find the latest version: https://jci.me/34450/pdf Research article Proteomic identification of FHL1 as the protein mutated in human reducing body myopathy Joachim Schessl,1 Yaqun Zou,1 Meagan J. -

FHL1 Mutants That Cause Clinically Distinct Human Myopathies Form
ß 2014. Published by The Company of Biologists Ltd | Journal of Cell Science (2014) 127, 2269–2281 doi:10.1242/jcs.140905 RESEARCH ARTICLE FHL1 mutants that cause clinically distinct human myopathies form protein aggregates and impair myoblast differentiation Brendan R. Wilding1, Meagan J. McGrath1, Gise`le Bonne2,3,4 and Christina A. Mitchell1,* ABSTRACT conserved cysteine and histidine residues mediate Zn2+ binding, which stabilises the folding and structure of the LIM domain. FHL1 mutations cause several clinically heterogeneous myopathies, FHL1 binds to signalling and cytoskeletal proteins, as well as including reducing body myopathy (RBM), scapuloperoneal myopathy transcription factors, acting as a transcriptional regulator of (SPM) and X-linked myopathy with postural muscle atrophy (XMPMA). nuclear factor of activated T cells (NFATc1) to enhance the The molecular mechanisms underlying the pathogenesis of FHL1 expression of genes that increase skeletal-muscle fibre size myopathies are unknown. Protein aggregates, designated ‘reducing (Cowling et al., 2008). bodies’, that contain mutant FHL1 are detected in RBM muscle but not FHL1 is mutated in six clinically distinct human myopathies, in several other FHL1 myopathies. Here, RBM, SPM and XMPMA including reducing body myopathy (RBM) (Schessl et al., 2008; FHL1 mutants were expressed in C2C12 cells and showed equivalent Schessl et al., 2009; Shalaby et al., 2009; Schessl et al., 2010; protein expression to wild-type FHL1. These mutants formed Selcen et al., 2011; Schreckenbach et al., 2013), X-linked aggregates that were positive for the reducing body stain dominant scapuloperoneal myopathy (SPM) (Quinzii et al., Menadione-NBT, analogous to RBM muscle aggregates. However, 2008; Chen et al., 2010), X-linked myopathy with postural hypertrophic cardiomyopathy (HCM) and Emery-Dreifuss muscular muscle atrophy (XMPMA) (Windpassinger et al., 2008), rigid- dystrophy (EDMD) FHL1 mutants generally exhibited reduced spine syndrome (RSS) (Shalaby et al., 2008), hypertrophic expression. -

Deletion of the Sclerotome-Enriched Lncrna PEAT Augments Ribosomal Protein Expression
Deletion of the sclerotome-enriched lncRNA PEAT augments ribosomal protein expression David A. Stafforda, Darwin S. Dichmanna, Jessica K. Changb, and Richard M. Harlanda,1 aDepartment of Molecular and Cell Biology, University of California, Berkeley, CA 94720; and bDepartment of Genetics, Stanford University, Stanford, CA 94305-5120 Contributed by Richard M. Harland, September 23, 2016 (sent for review July 22, 2016; reviewed by Margaret Buckingham and Chen-Ming Fan) To define a complete catalog of the genes that are activated during developing sclerotome by dissection from early embryos at 8- to mouse sclerotome formation, we sequenced RNA from embryonic 9.5-d postconception is technically difficult. Although a model mouse tissue directed to form sclerotome in culture. In addition to for presomitic mesoderm culture from stem cells has been de- well-known early markers of sclerotome, such as Pax1, Pax9,andthe veloped (10), this has not been exploited as an in vitro model of Bapx2/Nkx3-2 homolog Nkx3-1, the long-noncoding RNA PEAT (Pax1 the sclerotome. To obtain sufficient sclerotomal transcripts for enhancer antisense transcript) was induced in sclerotome-directed RNA-seq, we chemically treated explants of embryonic tissue to samples. Strikingly, PEAT is located just upstream of the Pax1 gene. bias differentiation of fluorescently marked presomitic mesoderm Using CRISPR/Cas9, we generated a mouse line bearing a complete toward the sclerotome. Following FACS, we compared control deletion of the PEAT-transcribed unit. RNA-seq on PEAT mutant and induced cultures to define the sclerotome transcriptome. In embryos showed that loss of PEAT modestly increases bone mor- addition to the previously described transcription factors, we identi- phogenetic protein target gene expression and also elevates the fied an uncharacterized noncoding RNA transcript that we named expression of a large subset of ribosomal protein mRNAs. -

Analysis of Gene Expression in Wild Type and Notch1 Mutant Retinal Cells by Single Cell Profiling Karolina Mizeracka1, Jeffrey M
Research Article Developmental Dynamics DOI 10.1002/dvdy.24006 Analysis of gene expression in wild type and Notch1 mutant retinal cells by single cell profiling Karolina Mizeracka1, Jeffrey M. Trimarchi1,2, Michael B. Stadler3, Constance L. Cepko1,4 1 Department of Genetics, Department of Ophthalmology, Harvard Medical School, Boston, MA 02115 2 Current Address: Department of Genetics, Development and Cell Biology, Iowa State University, Ames, IA 50014 3 Friedrich Miescher Institute for Biomedical Research, 4058 Basel, Switzerland 4 Howard Hughes Medical Institute, Department of Genetics, Department of Ophthalmology, Harvard Medical School, Boston, MA 02115 Correspondence: Constance Cepko 77 Avenue Louis Pasteur, Boston, MA 02115 Phone: (617) 432-7618 Fax: (617) 432-7595 Running title: Single cell profiling of Notch1 mutant retinal cells Key words: retina, progenitor, microarray, cell fate Summary: • Profiling of individual Notch1 deficient and wild type postnatal retinal cells on microarrays reveals changes in gene expression obscured by whole tissue analysis • Notch1 deficient cells downregulate progenitor and cell cycle markers with a concomitant upregulation in early rod photoreceptor markers • Based on classification, single Notch1 deficient and wild type cells represent Developmental Dynamics transition from progenitor to postmitotic cell • Individual wild type retinal cells express cell type markers of both photoreceptors and interneurons Grant sponsor and number: National Institutes of Health Grant R01EY09676 Accepted Articles are accepted, unedited articles for future issues, temporarily published online in advance of the final edited version. © 2013 Wiley Periodicals, Inc. Received: Mar 04, 2013; Revised: May 02, 2013; Accepted: May 13, 2013 Developmental Dynamics Page 2 of 66 Abstract Background: The vertebrate retina comprises sensory neurons, the photoreceptors, as well as many other types of neurons and one type of glial cell. -

Chikungunya Virus (CHIKV) Is Determined by a Wide Range of Host Factors
bioRxiv preprint doi: https://doi.org/10.1101/2020.09.29.319343; this version posted September 29, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Structural and Functional Characterization of Host FHL1 Protein Interaction with Hypervariable Domain of Chikungunya Virus nsP3 Protein Tetyana Lukash1, Tatiana Agback2, Francisco Dominguez1, Nikita Shiliaev1, Chetan Meshram1, Elena I. Frolova1, Peter Agback2*, Ilya Frolov1* Running title: FHL1 interaction with CHIKV nsP3 HVD 1Department of Microbiology, University of Alabama at Birmingham, AL, USA. 2Department of Molecular Sciences, Swedish University of Agricultural Sciences, Uppsala, Sweden. *Corresponding authors: Correspondence and requests for materials should be addressed to I.F. (mailing address: Department of Microbiology, University of Alabama at Birmingham, 1720 2nd Avenue South, BBRB 373/Box 3, Birmingham, AL 35294-2170; phone 1-(205)996-8957; email: [email protected]) or to P.A. (mailing address: Department of Molecular Sciences, Swedish University of Agricultural Sciences, Box 7015, SE-750 07 Uppsala, Sweden; phone +46-18-671581; email: [email protected]) 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.09.29.319343; this version posted September 29, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. ABSTRACT Decades of insufficient control resulted in unprecedented spread of chikungunya virus (CHIKV) around the globe and millions already suffered from the highly debilitating disease. Nevertheless, the current understanding of CHIKV-host interactions and adaptability of the virus to replication in mosquitoes and mammalian hosts is still elusive.