PA Marketplace Glossary of Dental Terms
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tooth Size Proportions Useful in Early Diagnosis
#63 Ortho-Tain, Inc. 1-800-541-6612 Tooth Size Proportions Useful In Early Diagnosis As the permanent incisors begin to erupt starting with the lower central, it becomes helpful to predict the sizes of the other upper and lower adult incisors to determine the required space necessary for straightness. Although there are variations in the mesio-distal widths of the teeth in any individual when proportions are used, the sizes of the unerupted permanent teeth can at least be fairly accurately pre-determined from the mesio-distal measurements obtained from the measurements of already erupted permanent teeth. As the mandibular permanent central breaks tissue, a mesio-distal measurement of the tooth is taken. The size of the lower adult lateral is obtained by adding 0.5 mm.. to the lower central size (see a). (a) Width of lower lateral = m-d width of lower central + 0.5 mm. The sizes of the upper incisors then become important as well. The upper permanent central is 3.25 mm.. wider than the lower central (see b). (b) Size of upper central = m-d width of lower central + 3.25 mm. The size of the upper lateral is 2.0 mm. smaller mesio-distally than the maxillary central (see c), and 1.25 mm. larger than the lower central (see d). (c) Size of upper lateral = m-d width of upper central - 2.0 mm. (d) Size of upper lateral = m-d width of lower central + 1.25 mm. The combined mesio-distal widths of the lower four adult incisors are four times the width of the mandibular central plus 1.0 mm. -
Crocodile Facts and Figures
Crocodile facts The saltwater crocodile is the largest living reptile species. It can grow up to six metres and is a serious threat to humans. Saltwater crocodiles have evolved special characteristics that make them excellent predators. • Large saltwater crocodiles can stay underwater for at least one hour because they can reduce their heart rate to 2-3 beats per minute. This means that crocodiles can wait underwater until they see prey, or if people are using the same spot regularly, the crocodile can wait underwater until someone approaches the water’s edge. • A crocodile can float with only eyes and nostrils exposed, enabling it to approach prey without being detected. • When under water, a special transparent eyelid protects the crocodile’s eye. This means that crocodiles can still see when they are completely submerged. • The tail of a crocodile is solid muscle and a major source of power, making it a strong swimmer and able to make sudden lunges out of the water to capture prey. These strong muscles also mean that for shorts bursts of time crocodiles can move faster than humans can on land. • Crocodiles have a thin layer of guanine crystals behind their retina. This intensifies images, allowing crocodiles to see better at low light levels. • Crocodiles have a ‘minimum exposure’ posture in the water, which means that only their sensory organs of eyes, cranial platform, ears and nostrils remain out of the water. This means that they often go unseen by prey, but if they are observed, the prey is often not able to tell how big the crocodile is. -

Veterinary Dentistry Basics
Veterinary Dentistry Basics Introduction This program will guide you, step by step, through the most important features of veterinary dentistry in current best practice. This chapter covers the basics of veterinary dentistry and should enable you to: ü Describe the anatomical components of a tooth and relate it to location and function ü Know the main landmarks important in assessment of dental disease ü Understand tooth numbering and formulae in different species. ã 2002 eMedia Unit RVC 1 of 10 Dental Anatomy Crown The crown is normally covered by enamel and meets the root at an important landmark called the cemento-enamel junction (CEJ). The CEJ is anatomically the neck of the tooth and is not normally visible. Root Teeth may have one or more roots. In those teeth with two or more roots the point where they diverge is called the furcation angle. This can be a bifurcation or a trifurcation. At the end of the root is the apex, which can have a single foramen (humans), a multiple canal delta arrangement (cats and dogs) or remain open as in herbivores. In some herbivores the apex closes eventually (horse) whereas whereas in others it remains open throughout life. The apical area is where nerves, blood vessels and lymphatics travel into the pulp. Alveolar Bone The roots are encased in the alveolar processes of the jaws. The process comprises alveolar bone, trabecular bone and compact bone. The densest bone lines the alveolus and is called the cribriform plate. It may be seen radiographically as a white line called the lamina dura. -

Identification Notes &~@~-/~: ~~*~@~,~ 'PTILE
CATEGORY Identification Notes &~@~-/~: ~~*~@~,~ ‘PTILE for wildlife law enforcement ~ C.rnrn.n N.rn./s: Al@~O~, c~~~dil., ~i~.xl, Gharial PROBLEM: Skulls of Crocodilians are often imported as souvenirs. nalch (-”W 4(JI -“by ieeth ??la&ularJy+i9 GUIDE TO PRELIMINARY IDENTIFICATION OF CROCODILL4N SKULLS 1. Nasal bones separated from nasal aperture; mandibular symphysis extends to the 15th tooth. 2. Gavialis gangeticus Nasal bones entering the nasal aperture; mandibular symphysisdoes not extend beyond the8th tooth . Tomistoma schlegelii 2. Nasal bones separated from premaxillary bones; 27 -29maxi11aryteeth,25 -26mandibularteeth Nasal bones in contact with premaxillaq bo Qoco@khs acutus teeth, 18-19 mandibular teeth . Tomiitomaschlegelii 3. Fourth mandibular tooth usually fitting into a notch in the maxilla~, 16-19 maxillary teeth, 14-15 mandibular teeth . .4 Osteolaemus temaspis Fourth mandibular tooth usually fitting into a pit in the maxilla~, 14-20 maxillary teeth, 17-22 mandibular teeth . .5 4. Nasal bones do not divide nasal aperture. .. CrocodylW (12 species) Alligator m&siss@piensh Nasalboncx divide nasal aperture . Osteolaemustetraspk. 5. Nasal bones do not divide nasal aperture. .6 . Paleosuchus mgonatus Bony septum divides nasal aperture . .. Alligator (2 species) 6. Fiveteethinpremaxilla~ bone . .7 . Melanosuchus niger Four teeth in premaxillary bone. ...Paleosuchus (2species) 7. Vomerexposed on the palate . Melanosuchusniger Caiman crocodiles Vomer not exposed on palate . ...”..Caiman (2species) Illustrations from: Moo~ C. C 1921 Me&m, F. 19S1 L-.. Submitted by: Stephen D. Busack, Chief, Morphology Section, National Fish& Wildlife Forensics LabDate submitted 6/3/91 Prepared in cooperation with the National Fkh & Wdlife Forensics Laboratoy, Ashlar@ OR, USA ‘—m More on reverse side>>> IDentMcation Notes CATEGORY: REPTILE for wildlife law enforcement -- Crocodylia II CAmmom Nda Alligator, Crocodile, Caiman, Gharial REFERENCES Medem, F. -

SHARK FACTS There Are 510 Species of Sharks
1 SHARK FACTS There are 510 species of sharks. Let’s learn more about a few of them. Common Six-gilled Thresher Shark Shark • Known for its 10 foot tail • Can grow up to 16 feet long • Stuns and herds fish with its long tail • Has six pairs of gills instead of the average of five • Warm blooded • Has one dorsal fin at the back of its body • Feeds on squid and schooling fish • Also known as cow shark or mud shark • Prefers to stay towards the top of deep bodies • Deep water shark of water Shortfin Great Mako Hammerhead Shark Shark • Bluish gray on top part of body and white on • Eyes are at opposite sides of its rectangular the belly shaped head • Has extremely sharp teeth, that stick out even when • Feeds on crustaceans, octopuses, rays and its mouth is shut small sharks • Feeds on sharks, swordfish and tuna • Usually found around tropical reefs • Jumps high in the air to escape fishing hooks • Can give birth to over 40 pups in one litter • Fastest of all the sharks as it can swim over 30 mph • Has a heigtened sense of electro-reception 2 SHARK FACTS Bull Nurse Shark Shark • Can grow up to 11 feet long and over 200 pounds • Has long, fleshy appendages called barbels that hang below its snout • Gray to brown in color with a white belly • Feeds on crab, lobster, urchins and fish • Feeds on fish, dolphins, sea turtles and other sharks • Usually found near rocky reefs, mudflats • Found in fresh and salt water and sandbars • Aggressive species • Enjoys laying on the ocean floor • Nocturnal animal Great Epaulette White Shark Shark • Can grow -

From Molecules to Mastication: the Development and Evolution of Teeth Andrew H
Advanced Review From molecules to mastication: the development and evolution of teeth Andrew H. Jheon,1,† Kerstin Seidel,1,† Brian Biehs1 and Ophir D. Klein1,2∗ Teeth are unique to vertebrates and have played a central role in their evolution. The molecular pathways and morphogenetic processes involved in tooth development have been the focus of intense investigation over the past few decades, and the tooth is an important model system for many areas of research. Developmental biologists have exploited the clear distinction between the epithelium and the underlying mesenchyme during tooth development to elucidate reciprocal epithelial/mesenchymal interactions during organogenesis. The preservation of teeth in the fossil record makes these organs invaluable for the work of paleontologists, anthropologists, and evolutionary biologists. In addition, with the recent identification and characterization of dental stem cells, teeth have become of interest to the field of regenerative medicine. Here, we review the major research areas and studies in the development and evolution of teeth, including morphogenesis, genetics and signaling, evolution of tooth development, and dental stem cells. © 2012 Wiley Periodicals, Inc. How to cite this article: WIREs Dev Biol 2013, 2:165–182. doi: 10.1002/wdev.63 MORPHOGENESIS AND of natural selection in response to the environmental DEVELOPMENT pressures provided by various types of food (Figure 2). Teeth, or tooth-like structures called odontodes he formation of a head with complex jaws or denticles, are present in all vertebrate groups, Tand networked sensory organs was a central although they have been lost in some lineages. Most innovation in the evolution of vertebrates, allowing fish and reptiles, and many amphibians, possess 1 the shift to an active predatory lifestyle. -

Tooth Anatomy
Tooth Anatomy To understand some of the concepts and terms that we use in discussing dental conditions, it is helpful to have a picture of what these terms represent. This picture is from the American Veterinary Dental College. Pulp Dentin Crown Enamel Gingiva Root Periodontal Ligament Alveolar Bone supporting the tooth Crown: The portion of the tooth projecting from the gums. It is covered by a layer of enamel, though dentin makes up the bulk of the tooth structure. The crown is the working part of the tooth. In dogs and cats, most teeth are conical or pyramidal in shape for cutting and shearing action. Gingiva: The gum tissue surrounds the crown of the tooth and protects the root and bone which are subgingival (below the gum line). The gingiva is the first line of defense against periodontal disease. The space where the gingiva meets the crown is where periodontal pockets develop. Measurements are taken here with a periodontal probe to assess the stage of periodontal disease. When periodontal disease progresses it can involve the Alveolar Bone, leading to bone loss and root exposure. Root Canal: The root canal contains the pulp. This living tissue is protected by the crown and contains blood vessels, nerves and specialized cells that produce dentin. Dentin is produced throughout the life of the tooth, which causes the pulp canal to narrow as pets age. Damage to the pulp causes endodontic disease which is painful, and can lead to infection and loss of the tooth. Periodontal Ligament: This tissue is what connects the tooth root to the bone to keep it anchored to its socket. -

The Serrated Teeth Ofsebecus and the Iberoccitanian Crocodile. A
STVDIA GEOLÓGICA SALMANTICENSIA, XXIX, 127-144 (1994) THE SERRATED TEETH OF SEBECUS AND THE IBEROCCITANIAN CROCODILE, A MORPHOLOGICAL AND ULTRASTRUCTURAL COMPARISON O. LEGASA (*) A. D. BUSCALIONI (*) Z. GASPARINI (**) RESUMEN:- Se compara la morfología y ultraestructura del esmalte de dientes aserrados de cocodrilos. La muestra está compuesta por coronas aisladas atribuidas a la forma iberoccitana (Eoceno de la cuenca del Duero) y Sebecus (S. ?huilensis y S. icaeorhinus del Mioceno medio de Colombia y Eoceno inferior de Argentina). Se examinaron caracteres cuantitativos y cualitativos de la corona y sus márgenes aserrados. En este sentido, se han explorado todas las variables que caracterizan la simetría de la corona dentaria, diferenciando los dientes más grandes de Sebecus ?huilensis de los de la forma iberoccitana. El análisis de la ultraestructura evidencia una organización pseudoprismática del esmalte de Sebecus ?huilensis, contrastando con el modelo aprismático del cocodrilo iberoccitano. En este artículo se definen los dientes aserrados como aquellos que poseen carenas con dentículos aislados. Un dentículo aislado es una unidad morfológica discreta. Esta definición excluye los dientes con carenas crenulados formadas por crestas anastomosadas convergentes, que proceden de la ornamentación del esmalte. También, se evalúan aspectos funcionales de los dientes considerando los microdesgastes observados en los dentículos aislados. ABSTRACT:- The morphology and enamel ultrastructure of serrated teeth of crocodiles is compared. The sample is composed by isolated teeth attributed to the iberoccitanian form (Eocene of the Duero basin, Spain) and Sebecus (S. ?huilensis and (*): Unidad de Paleontología. Dpto. Biología. Universidad Autónoma, Cantoblanco 28049 Madrid, Spain. (**): Museo de La Plata, Paseo del Bosque s/n. 1900 La Plata. -

Vol 35, Number 4, December 2020
The ECPHORA The Newsletter of the Calvert Marine Museum Fossil Club Volume 35 Number 4 December 2020 Features Up and Coming Artist Art by Eaton Ekarintaragun Shark Dentitions by George F. Klein Pathologic Shark Teeth by Bill Heim Inside President’s Column Membership Renewal Polymer Ammonite Ecphoras Found Pathological Otodus Tooth Fossil Carcharodon carcharias Tooth Found Special Needs Night Self-Bitten Snaggletooth Bohaska on the Beach Seahorse Skeleton and CMMFC young member, Eaton Ekarintaragun loves both paleontology much more… and art. Here is an example of one of his recent pieces. This is Eaton's CMM Fossil Club interpretation/creation of a Synthetoceras. Meetings. Note the new day of the week, date, and time for our next fossil club meeting. Monday, February 22, 2021, 7 pm, Zoom meeting. Public lecture by Dr. Victor Perez to begin at 7:30 pm. Zoom invitation to follow via email. Work in progress. Photos submitted by Pitoon Ekarintaragun. ☼ CALVERT MARINE MUSEUM www.calvertmarinemuseum.com 2 The Ecphora December 2020 Greetings Club Members! Sculpey Polymer Clay Ammonite President’s Column. Every time it seems it can’t get worse 2020 dishes out something new. As I write this my neighbor was just taken away via ambulance, the remote server for my workplace crashed and the water main for our street ruptured. All of this within 2 hours on a Monday afternoon. Ugh. I hope everyone is coping as best as possible during this crazy year and is relaxing whenever possible outdoors, be it just taking a walk or getting in a fossil excursion. Keeping stress-free seems to be the best medicine lately. -

Glossary of Commonly Used Dental Terms
Glossary of Commonly Used Dental Terms A • Abutment: A tooth or implant used to support a prosthesis. A crown unit used as part of a fixed bridge. • Abscess: A localized inflammation due to a collection of pus in the bone or soft tissue, usually caused by an infection. • Amalgam: A dental filling material, composed of mercury and other minerals, used to fill decayed teeth. • Alveoloplasty: A surgical procedure used to recontour the supporting bone struc tures in preparation of a complete or partial denture. • Anesthetic: A class of drugs that eliminated of reduces pain. See local anesthetic. • Anterior: Refers to the teeth and tissues located towards the front of the mouth (upper or lower incisors and canines). • Apex: The tip end of a root. • Apexification: A method of inducing apical closure, or the continual apical develop ment of the root of an incompletely formed tooth, in which the pulp is no longer vital. B • Bicuspid: A two-cuspid tooth found between the molar and the cuspid also known as an eye tooth or canine tooth. • Biopsy: A process of removing tissue to determine the existence of pathology. • Bitewing x-ray: X-rays taken of the crowns of teeth to check for decay. • Bleaching: The technique of applying a chemical agent, usually hydrogen peroxide, to the teeth to whiten them. • Bondin: A process to chemically etch the tooth's enamel to better attach ( bond ) composite filling material, veneers, or plastic/acrylic. • Bone loss: The breakdown and loss of the bone that supports the teeth, usually caused by infection or long-term occlusal ( chewing areas of the teeth ) stress. -

Glossary • Amalgam: Common Filling Material, Also Known As “Silver Fillings,” Containing Mercury (Approx
Glossary • Amalgam: common filling material, also known as “silver fillings,” containing mercury (approx. 50 percent), silver, tin, copper, and zinc. • Anorexia nervosa: a psychiatric diagnosis that describes an eating disorder characterized by low body weight and body image distortion. Individuals with anorexia often control body weight by voluntary starvation, purging, vomiting, excessive exercise, or other weight control measures, such as diet pills or diuretic drugs. • Bacteremia: the presence of bacteria in the blood. It is most commonly diagnosed by blood culture. • Binge eating: a psychiatric disorder in which a subject periodically does not exercise control over consumption of food. • Bright Futures: a national health promotion initiative. It is a vision, a philosophy, a set of expert guidelines, and a practical developmental approach to providing health supervision for children and adolescents from birth through age 21. The mission of Bright Futures is to promote and improve the health, education, and well-being of infants, children, adolescents, families, and communities. • Bulimia: a psychological condition in which the subject engages in recurrent binge eating followed by an intentional purging. Purging typically takes the form of vomiting; inappropriate use of laxatives, enemas, diuretics or other medication; excessive physical exercise, or fasting. • Burning mouth syndrome (BMS) or (Glossodynia): a condition characterized by a burning or tingling sensation on the lips, tongue, or entire mouth. Possible causes include nutritional deficiencies, chronic anxiety or depression, type 2 diabetes, menopause, oral disorders such as thrush or dry mouth, or damaged nerves. • Cardiovascular disease: class of diseases that involve the heart and/or blood vessels (arteries and veins). • Caries experience: represented by a missing tooth or presence of a cavity or a filling, indicating that opportunities for primary prevention may have been missed. -
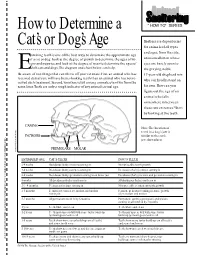
How to Determine a Cat's Or Dog's
How to Determine a “HOW TO” SERIES Cat’s or Dog’s Age Shelters are depositories for animals of all types and ages, from the cute, xamining teeth is one of the best ways to determine the approximate age of a cat or dog. Look at the degree of growth to determine the ages of kit- unweaned kitten whose tens and puppies,and look at the degree of wear to determine the ages of eyes are barely open to Eadult cats and dogs.The diagram and chart below can help. the graying, noble Be aware of two things that can throw off your estimate. First, an animal who has 17-year-old shepherd mix received dental care will have better-looking teeth than an animal who has not re- who can hardly stand on ceived such treatment.Second,variations exist among animals,even two from the same litter.Teeth are only a rough indicator of any animal’s actual age. his own.How can you figure out the age of an animal who falls somewhere in between these two extremes? Start by looking at the teeth. CANINE Note:The location of teeth in a dog’s jaw is INCISORS similar to the cat’s jaw shown here. PREMOLARS MOLAR Illustration by Susie DuckworthIllustration by ESTIMATED AGE CAT’S TEETH DOG’S TEETH 2-4 weeks Deciduous (baby) incisors coming in No noticeable tooth growth 3-4 weeks Deciduous (baby) canines coming in Deciduous (baby) canines coming in 4-6 weeks Deciduous (baby) premolars coming in on lower jaw Deciduous (baby) incisors and premolars coming in 8 weeks All deciduous (baby) teeth are in All deciduous (baby) teeth are in 1 3 ⁄2 - 4 months Permanent incisors coming in No