The Cellular Basis of Disease Cell Injury 1
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Efficacy of Texture and Color Enhancement Imaging In
www.nature.com/scientificreports OPEN Efcacy of Texture and Color Enhancement Imaging in visualizing gastric mucosal atrophy and gastric neoplasms Tsubasa Ishikawa1, Tomoaki Matsumura1*, Kenichiro Okimoto1, Ariki Nagashima1, Wataru Shiratori1, Tatsuya Kaneko1, Hirotaka Oura1, Mamoru Tokunaga1, Naoki Akizue1, Yuki Ohta1, Keiko Saito1, Makoto Arai1,2, Jun Kato1 & Naoya Kato1 In 2020, Olympus Medical Systems Corporation introduced the Texture and Color Enhancement Imaging (TXI) as a new image-enhanced endoscopy. This study aimed to evaluate the visibility of neoplasms and mucosal atrophy in the upper gastrointestinal tract through TXI. We evaluated 72 and 60 images of 12 gastric neoplasms and 20 gastric atrophic/nonatrophic mucosa, respectively. The visibility of gastric mucosal atrophy and gastric neoplasm was assessed by six endoscopists using a previously reported visibility scale (1 = poor to 4 = excellent). Color diferences between gastric mucosal atrophy and nonatrophic mucosa and between gastric neoplasm and adjacent areas were assessed using the International Commission on Illumination L*a*b* color space system. The visibility of mucosal atrophy and gastric neoplasm was signifcantly improved in TXI mode 1 compared with that in white-light imaging (WLI) (visibility score: 3.8 ± 0.5 vs. 2.8 ± 0.9, p < 0.01 for mucosal atrophy; visibility score: 2.8 ± 1.0 vs. 2.0 ± 0.9, p < 0.01 for gastric neoplasm). Regarding gastric atrophic and nonatrophic mucosae, TXI mode 1 had a signifcantly greater color diference than WLI (color diferences: 14.2 ± 8.0 vs. 8.7 ± 4.2, respectively, p < 0.01). TXI may be a useful observation modality in the endoscopic screening of the upper gastrointestinal tract. -

Gas Gangrene Infection of the Eyes and Orbits
Br J Ophthalmol: first published as 10.1136/bjo.69.2.143 on 1 February 1985. Downloaded from British Journal of Ophthalmology, 1985, 69, 143-148 Gas gangrene infection of the eyes and orbits GERARD W CROCK,' WILSON J HERIOT,' PATTABIRAMAN JANAKIRAMAN,' AND JOHN M WEINER2 From the 'Department of Ophthalmology, University ofMelbourne, and the2C H Greer Pathology Laboratory, the Royal Victorian Eye and Ear Hospital, East Melbourne, Australia SUMMARY The literature on Clostridium perfringens infections is reviewed up to 1983. An additional case is reported with bilateral clostridial infections of the eye and orbit. One eye followed the classical course of relentless panophthalmitis, amaurosis, and orbital cellulitis ending in enucleation. The second eye contained intracameral mud and gas bubbles that were removed by vitrectomy instrumentation. Subsequent removal of the toxic cataract resulted in a final aided visual acuity of 6/18, N8. This is the third report of a retained globe, and we believe the only known case where the patient was left with useful vision. Clostridium perfringens is a ubiquitous Gram- arms, chest, and abdomen. He was admitted to a positive bacillus found in soil and bowel flora. It is the general hospital, where he was examined under most common of four clostridia species identified in anaesthesia, and his injuries were attended to. copyright. cases of gas gangrene in man.' All species are obligate Ocular findings. The right cornea and anterior anaerobes and are usually saprophytic rather than chamber were intact. There was a scleral laceration pathogenic. Clostridium perfringens is a feared con- over the superonasal area of the pars plana with taminant of limb injuries and may result in death due vitreous prolapse. -
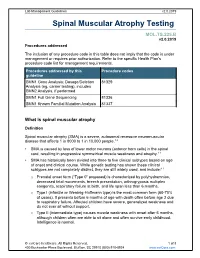
Spinal Muscular Atrophy Testing
Lab Management Guidelines v2.0.2019 Spinal Muscular Atrophy Testing MOL.TS.225.B v2.0.2019 Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline SMN1 Gene Analysis; Dosage/Deletion 81329 Analysis (eg, carrier testing), includes SMN2 Analysis, if performed SMN1 Full Gene Sequencing 81336 SMN1 Known Familial Mutation Analysis 81337 What is spinal muscular atrophy Definition Spinal muscular atrophy (SMA) is a severe, autosomal recessive neuromuscular disease that affects 1 in 8000 to 1 in 10,000 people.1,2 SMA is caused by loss of lower motor neurons (anterior horn cells) in the spinal cord, resulting in progressive symmetrical muscle weakness and atrophy.1-3 SMA has historically been divided into three to five clinical subtypes based on age of onset and clinical course. While genetic testing has shown these clinical subtypes are not completely distinct, they are still widely used, and include:1-3 o Prenatal onset form (“Type 0” proposed) is characterized by polyhydramnios, decreased fetal movements, breech presentation, arthrogryposis multiplex congenita, respiratory failure at birth, and life span less than 6 months. o Type I (infantile or Werdnig-Hoffmann type) is the most common form (60-70% of cases). It presents before 6 months of age with death often before age 2 due to respiratory failure. Affected children have severe, generalized weakness and do not ever sit without support. -

Università Degli Studi Di Milano
UNIVERSITÀ DEGLI STUDI DI MILANO SCUOLA DI DOTTORATO IN MEDICINA MOLECOLARE CICLO XXVIII Anno Accademico 2014/2015 TESI DI DOTTORATO DI RICERCA MED09 STUDIES OF HEME-REGULATED eIF2α KINASE STRESS SIGNALING ON MATURATION OF MACROPHAGES AND ERYTHROBLASTIC ISLAND FORMATION IN IRON RESTRICTIVE ERYTHROPOIESIS Dottorando : Elena PALTRINIERI Matricola N° R10203 TUTORE : Chiar.ma Prof.ssa Maria Domenica CAPPELLINI CO-TUTORE: Prof.ssa Jane-Jane CHEN DIRETTORE DEL DOTTORATO: Chiar.mo Prof. Mario CLERICI ABSTRACT Iron is the most important metal for the human body. Different states of iron deficiency have long existed and remain very common in today’s population. The vast majority of cases of iron deficiency are acquired as a result from blood loss. Any condition in which dietary iron intake does not meet the body’s demands will result in iron deficiency. Iron and heme are both fundamental in hemoglobin synthesis and erythroid cell differentiation. In addition to act as a prosthetic group for hemoglobin, heme regulates the transcription of globin genes and controls the translational activity in erythroid precursors through modulation of the kinase activity of the eIF2α kinase HRI which is regulated by heme. HRI, the heme-regulated inhibitor of translation, was first discovered in reticulocytes under the conditions of iron and heme deficiencies. During heme deficiency conditions, in the erythroid precursors protein synthesis is inhibited by phosphorylation of the α-subunit of the eukaryotic initiation factor 2 (eIF2α) as the result of the activation of HRI. The role of HRI is to control that the amount of globin chains synthesized are not in excess of what can be utilized for hemoglobin tetramers depending of heme available. -

Microsatellite Instability in Colorectal Cancer Liquid Biopsy—Current Updates on Its Potential in Non-Invasive Detection, Prognosis and As a Predictive Marker
diagnostics Review Microsatellite Instability in Colorectal Cancer Liquid Biopsy—Current Updates on Its Potential in Non-Invasive Detection, Prognosis and as a Predictive Marker Francis Yew Fu Tieng 1 , Nadiah Abu 1, Learn-Han Lee 2,* and Nurul-Syakima Ab Mutalib 1,2,3,* 1 UKM Medical Molecular Biology Institute (UMBI), Universiti Kebangsaan Malaysia, Kuala Lumpur 56000, Malaysia; [email protected] (F.Y.F.T.); [email protected] (N.A.) 2 Novel Bacteria and Drug Discovery Research Group, Microbiome and Bioresource Research Strength, Jeffrey Cheah School of Medicine and Health Sciences, Monash University Malaysia, Selangor 47500, Malaysia 3 Faculty of Health Sciences, Universiti Kebangsaan Malaysia, Kuala Lumpur 50300, Malaysia * Correspondence: [email protected] (L.-H.L.); [email protected] (N.-S.A.M.); Tel.: +60-391459073 (N.-S.A.M.) Abstract: Colorectal cancer (CRC) is the third most commonly-diagnosed cancer in the world and ranked second for cancer-related mortality in humans. Microsatellite instability (MSI) is an indicator for Lynch syndrome (LS), an inherited cancer predisposition, and a prognostic marker which predicts the response to immunotherapy. A recent trend in immunotherapy has transformed cancer treatment to provide medical alternatives that have not existed before. It is believed that MSI-high (MSI-H) CRC patients would benefit from immunotherapy due to their increased immune infiltration and higher neo-antigenic loads. MSI testing such as immunohistochemistry (IHC) and PCR MSI assay Citation: Tieng, F.Y.F.; Abu, N.; Lee, has historically been a tissue-based procedure that involves the testing of adequate tissue with a high L.-H.; Ab Mutalib, N.-S. -

General Pathology
Jordan University of Science and Technology Faculty of Medicine 2018-2019 COURSE TITLE : GENERAL PATHOLOGY. COURSE CODE : MED 231. CREDIT HOURS : 3 CREDIT HOURS SEQUENCE : YEAR 2, FIRST SEMESTER COURSE COORDINATOR: Dr. Alia AlMuhtaseb; Dr. Mohammad Orjani CONTACT: [email protected]; [email protected] Course Description: This course deals with the investigation of those pathological mechanisms common to all tissue-cell pathology. Attention is paid to the processes of cellular adaptation, inflammation, repair, immunology, cellular accumulation, and neoplasia. Lecture will attempt first to familiarize the student with our basic layers of defense. Next those vocabulary terms and concepts relevant to the disease process will be introduced. The terminology employed is both medical and chiropractic. Processes and concepts will be developed with the aid of Data show. An interactive format is employed in which the instructor poses questions to enable the student to self-test their knowledge prior to exams and develop skills in communicating these basic pathological concepts to others. During the course and whenever relevant the students are exposed to clinical problems to emphasize the explanations of symptoms, signs, investigations and forms of treatments. Practical sessions are planned to give students the opportunity to expose their knowledge for discussion and confirm concepts learned in lectures. Small group discussions of clinical cases are planned at the end of the course were students are divided into small groups and with the help of an instructor they analyze and discuss the problem. The course will be given through 28 lectures, 7 practical (laboratory) sessions, and one small group discussion activity over 15 weeks and for one whole semester. -

Short Course 10 Metaplasia in The
0 3: 436-446 Rev Esp Patot 1999; Vol. 32, N © Prous Science, SA. © Sociedad Espajiola de Anatomia Patot6gica Short Course 10 © Sociedad Espafiola de Citologia Metaplasia in the gut Chairperson: NA. Wright, UK. Co-chairpersons: G. Coggi, Italy and C. Cuvelier, Belgium. Overview of gastrointestinal metaplasias only in esophagus but also in the duodenum, intestine, gallbladder and even in the pancreas. Well established is columnar metaplasia J. Stachura of esophageal squamous epithelium. Its association with increased risk of esophageal cancer is widely recognized. Recent develop- Dept. of Pathomorphology, Jagiellonian University ments have suggested, however, that only the intestinal type of Faculty of Medicine, Krakdw, Poland. metaplastic epithelium (classic Barrett’s esophagus) predisposes to cancer. Another field of studies is metaplasia in the short seg- ment at the esophago-cardiac junction, its association with Metaplasia is a reversible change in which one aduit cell type is Helicobacter pylon infection and/or reflux disease and intestinal replaced by another. It is always associated with some abnormal metaplasia in the cardiac and fundic areas. stimulation of tissue growth, tissue regeneration or excessive hor- Studies on gastric mucosa metaplasia could be divided into monal stimulation. Heterotopia, on the other hand, takes place dur- those concerned with pathogenesis and detailed structural/func- ing embryogenesis and is usually supposed not to be associated tional features and those concerned with clinical significance. with tissue damage. Pancreatic acinar cell clusters in pediatric gas- We know now that gastric mucosa may show not only complete tric mucosa form another example of aberrant cell differentiation. and incomplete intestinal metaplasia but also others such as ciliary Metaplasia is usually divided into epithelial and connective tis- and pancreatic metaplasia. -

1 Pathology Week 1 – Cellular Adaptation, Injury and Death
Pathology week 1 – Cellular adaptation, injury and death Cellular responses to injury Cellular Responses to Injury Nature and Severity of Injurious Stimulus Cellular Response Altered physiologic stimuli: Cellular adaptations: • ↑demand, ↑ trophic stimulation (e.g. growth factors, hormones) • Hyperplasia, hypertrophy • ↓ nutrients, stimulation • Atrophy • Chronic irritation (chemical or physical) • Metaplasia Reduced oxygen supply; chemical injury; microbial infection Cell injury: • Acute and self-limited • Acute reversible injury • Progessive and severe (including DNA damage) • Irreversible injury → cell death Necrosis Apoptosis • Mild chronic injury • Subcellular alterations in organelles Metabolic alterations, genetic or acquired Intracell accumulations; calcifications Prolonged life span with cumulative sublethal injury Cellular aging Hyperplasia - response to increased demand and external stimulation - ↑ number cells - ↑ volume of organ - often occurs with hypertrophy - occurs if cells able to synthesize DNA – mitotic division - physiologic or pathologic Physiological hyperplasia A) hormonal – ↑ functional capacity tissue when needed (breast in puberty, uterus in pregnancy) B) compensatory - ↑ tissue mass after damage/resection (post-nephrectomy) Mechanisms: - ↑ local production growth factors or activation intracellular signaling pathways o both → production transcription factors that turn on cellular genes incl those encoding growth factors, receptors for GFs, cell cycle regulators →→ cellular proli feration - in hormonal hyperplasia -

Hyperplasia (Growth Factors
Adaptations Robbins Basic Pathology Robbins Basic Pathology Robbins Basic Pathology Coagulation Robbins Basic Pathology Robbins Basic Pathology Homeostasis • Maintenance of a steady state Adaptations • Reversible functional and structural responses to physiologic stress and some pathogenic stimuli • New altered “steady state” is achieved Adaptive responses • Hypertrophy • Altered demand (muscle . hyper = above, more activity) . trophe = nourishment, food • Altered stimulation • Hyperplasia (growth factors, . plastein = (v.) to form, to shape; hormones) (n.) growth, development • Altered nutrition • Dysplasia (including gas exchange) . dys = bad or disordered • Metaplasia . meta = change or beyond • Hypoplasia . hypo = below, less • Atrophy, Aplasia, Agenesis . a = without . nourishment, form, begining Robbins Basic Pathology Cell death, the end result of progressive cell injury, is one of the most crucial events in the evolution of disease in any tissue or organ. It results from diverse causes, including ischemia (reduced blood flow), infection, and toxins. Cell death is also a normal and essential process in embryogenesis, the development of organs, and the maintenance of homeostasis. Two principal pathways of cell death, necrosis and apoptosis. Nutrient deprivation triggers an adaptive cellular response called autophagy that may also culminate in cell death. Adaptations • Hypertrophy • Hyperplasia • Atrophy • Metaplasia HYPERTROPHY Hypertrophy refers to an increase in the size of cells, resulting in an increase in the size of the organ No new cells, just larger cells. The increased size of the cells is due to the synthesis of more structural components of the cells usually proteins. Cells capable of division may respond to stress by undergoing both hyperrtophy and hyperplasia Non-dividing cell increased tissue mass is due to hypertrophy. -

Ghasemi Gh. Comparison of Laparoscopic Ovarian Drilling
Archive of SID Original Article Comparison of Laparoscopic Ovarian Drilling Success between Two Standard and Dose-Adjusted Methods in Polycystic Ovary Syndrome: A Randomized Clinical Trial Leili Hafizi, M.D.1, Maliheh Amirian, M.D.2, Yasmin Davoudi, M.D.3, Mona Jaafari, M.D.1, Ghazal Ghasemi, M.D.1* 1. Department of Obstetrics and Gynaecology, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran 2. Department of IVF and Infertility, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran 3. Department of Radiology, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran Abstract Background: One of the treatment methods for increasing the ovarian response to ovulation induction in polycystic ovary syndrome (PCOS) is laparoscopic ovarian drilling (LOD). The optimal amount of the electrosurgical energy discharged in the ovaries to achieve maximum treatment response with minimal follicle injury is unknown. This study was performed to compare the success level of LOD by means of standard and dose-adjusted treatment methods among infertile clomiphene-resistant PCOS women. Materials and Methods: This randomized clinical trial was conducted on infertile clomiphene citrate-resistant PCOS women in the Gynaecology Department of Imam Reza Hospital between 2016 and 2017. The patients were randomly di- vided into two groups based on the ovarian cautery method. The two groups were examined and compared regarding the antral follicles, the serum levels of anti-Müllerian hormone (AMH), androgens, and mid-luteal progesterone one month after surgery. The regularity of cycles, ovulation, and pregnancy were examined monthly up to six months after surgery. Results: In total, 60 women received bilateral LOD (n=30 per group). -
Cellular Adaptation
Cellular Adaptation Dr. Adeboye OO (MBBS, Cert. LMIH, FMCPath) Dept of Anatomic Pathology Bowen University Cellular adaptation • Cell death is not the only consequence of cellular injury or stress • Cells can respond to excessive physiologic or pathologic stimuli by undergoing both functional and morphologic change in which a new steady state is achieved that preserves the viability of the cell(Adaptation) . • The adaptive response include- • Adaptation of growth and differentiation • Intracellular accumulation • Pathologic calcification • Hyaline change • Cellular aging Adaptation of growth and differentiation • Adaptations are reversible changes in the size, number,phenotype, metabolic activity, or functions of cells in response to changes in their environment. Such adaptations may take several distinct forms : • 1. hyperplasia • 2. hypertrophy • 3. atrophy • 4. metaplasia hypertrophy • Increase in the size of cells that result in the increase in size of the affected organ. • No new cells just larger cells • May coexist with hyperplasia in cells capable of division( eg epithelial, hematopoesis etc), in non dividing cells (eg the nerve ,cardiac and skeletal muscle) increase tissue mass is due to hypertrophy • Can be physiologic or pathologic Physiologic hypertrophy • Caused by- (a) increased functional demand eg hypertrophy of striated muscle in muscle builder.(b) stimulation by hormones or growth factors eg physiologic hypertrophy of the uterus during pregnancy Hypertrophy of uterus during pregnancy Micrograph showing smooth muscle -

Tissue Engineering Strategies to Improve Tendon Healing and Insertion Site Integration
Tissue Engineering Strategies to Improve Tendon Healing and Insertion Site Integration A dissertation submitted to the Division of Research and Advanced Studies of the University of Cincinnati in partial fulfillment of the of the requirements for the degree of DOCTOR OF PHILOSOPHY (Ph.D.) in the Department of Biomedical Engineering of the College of Engineering and Applied Science 2011 by Kirsten Rose Carol Kinneberg B.S., University of Minnesota, Twin Cities, MN, 2006 Committee Chair: Jason T. Shearn Abstract Tendon and ligament tears and ruptures remain common and significant musculoskeletal injuries. Repairing these injuries continues to be a prominent challenge in orthopaedics and sports medicine. Despite advances in surgical techniques and procedures, traditional repair techniques maintain a high incidence of re-rupture. This has led some researchers to consider using tissue engineered constructs (TECs). Previous studies in our laboratory have demonstrated that TEC stiffness at the time of surgery is positively correlated with repair tissue stiffness 12 weeks post-surgery. This correlation provided the rationale for implanting a soft tissue patellar tendon autograft (PTA) to repair a central-third defect in the rabbit patellar tendon (PT). The PTA was significantly stiffer than previous TECs and matched the stiffness of the normal central-third PT. Accordingly, we expected a significant improvement in repair tissue biomechanics relative to both natural healing (NH) and TEC repair. At 12 weeks, treatment with PTA improved repair tissue stiffness relative to NH. However, PTA and NH tissues did not differ in maximum force, modulus or maximum stress. Additionally, neither repair group regenerated normal zonal insertion sites.