Intra-Articular Injections for Osteoarthritis of the Knee
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) Patent Application Publication (10) Pub. No.: US 2008/0317805 A1 Mckay Et Al
US 20080317805A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2008/0317805 A1 McKay et al. (43) Pub. Date: Dec. 25, 2008 (54) LOCALLY ADMINISTRATED LOW DOSES Publication Classification OF CORTICOSTEROIDS (51) Int. Cl. A6II 3/566 (2006.01) (76) Inventors: William F. McKay, Memphis, TN A6II 3/56 (2006.01) (US); John Myers Zanella, A6IR 9/00 (2006.01) Cordova, TN (US); Christopher M. A6IP 25/04 (2006.01) Hobot, Tonka Bay, MN (US) (52) U.S. Cl. .......... 424/422:514/169; 514/179; 514/180 (57) ABSTRACT Correspondence Address: This invention provides for using a locally delivered low dose Medtronic Spinal and Biologics of a corticosteroid to treat pain caused by any inflammatory Attn: Noreen Johnson - IP Legal Department disease including sciatica, herniated disc, Stenosis, mylopa 2600 Sofamor Danek Drive thy, low back pain, facet pain, osteoarthritis, rheumatoid Memphis, TN38132 (US) arthritis, osteolysis, tendonitis, carpal tunnel syndrome, or tarsal tunnel syndrome. More specifically, a locally delivered low dose of a corticosteroid can be released into the epidural (21) Appl. No.: 11/765,040 space, perineural space, or the foramenal space at or near the site of a patient's pain by a drug pump or a biodegradable drug (22) Filed: Jun. 19, 2007 depot. E Day 7 8 Day 14 El Day 21 3OO 2OO OO OO Control Dexamethasone DexamethasOne Dexamethasone Fuocinolone Fluocinolone Fuocinolone 2.0 ng/hr 1Ong/hr 50 ng/hr 0.0032ng/hr 0.016 ng/hr 0.08 ng/hr Patent Application Publication Dec. 25, 2008 Sheet 1 of 2 US 2008/0317805 A1 900 ----------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------- 80.0 - 7OO – 6OO - 5OO - E Day 7 EDay 14 40.0 - : El Day 21 2OO - OO = OO – Dexamethasone Dexamethasone Dexamethasone Fuocinolone Fluocinolone Fuocinolone 2.0 ng/hr 1Ong/hr 50 ng/hr O.OO32ng/hr O.016 ng/hr 0.08 nghr Patent Application Publication Dec. -

(12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 De Juan Et Al
US 200601 10428A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 de Juan et al. (43) Pub. Date: May 25, 2006 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA (US); A6F 2/00 (2006.01) Signe E. Varner, Los Angeles, CA (52) U.S. Cl. .............................................................. 424/427 (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Correspondence Address: Featured is a method for instilling one or more bioactive SCOTT PRIBNOW agents into ocular tissue within an eye of a patient for the Kagan Binder, PLLC treatment of an ocular condition, the method comprising Suite 200 concurrently using at least two of the following bioactive 221 Main Street North agent delivery methods (A)-(C): Stillwater, MN 55082 (US) (A) implanting a Sustained release delivery device com (21) Appl. No.: 11/175,850 prising one or more bioactive agents in a posterior region of the eye so that it delivers the one or more (22) Filed: Jul. 5, 2005 bioactive agents into the vitreous humor of the eye; (B) instilling (e.g., injecting or implanting) one or more Related U.S. Application Data bioactive agents Subretinally; and (60) Provisional application No. 60/585,236, filed on Jul. (C) instilling (e.g., injecting or delivering by ocular ion 2, 2004. Provisional application No. 60/669,701, filed tophoresis) one or more bioactive agents into the Vit on Apr. 8, 2005. reous humor of the eye. Patent Application Publication May 25, 2006 Sheet 1 of 22 US 2006/0110428A1 R 2 2 C.6 Fig. -
Jan 19, 2009 Listing of Generic, Non
http://www.medword.com/uspa.html Jan 19, 2009 Listing of generic, non-prescription, prescription, and OTC (over-the-counter) p harmaceuticals A-200 Gel Concentrate A-200 Shampoo Concentrate A-25 A-Cillin A-Fil A-Hydrocort A-methaPred A-Phedrin A-Spas S/L A Plus A.C. & C. A.P.L. A.R.M. Allergy Relief A.R.M. Maximum Strength Caplets A/B Otic A/Fish Oil A/T/S abacavir abarelix-depot-F abarelix-depot-M Abbokinase Abbokinase Open-Cath Abelcet Abenol Abitrate Absorbine Athletes Foot Absorbine Jock Itch Absorbine Jr. Antifungal AC acarbose Accolate Accupep HPF Accupril Accuretic Accutane Accutane Roche acebutolol Acel-Imune Acellular DTP Aceon Acet-2 Acet-3 Acet Codeine 30 Acet Codeine 60 Aceta Aceta Elixir Aceta Tablets acetaminophen acetaminophen-butalbital acetaminophen-caffeine acetaminophen-chlorpheniramine acetaminophen-codeine acetaminophen-dextromethorphan acetaminophen-diphenhydramine acetaminophen-hydrocodone acetaminophen-oxycodone acetaminophen-phenyltoloxamine acetaminophen-propoxyphene acetaminophen-propoxyphene hydrochloride acetaminophen-propoxyphene napsylate acetaminophen-pseudoephedrine acetazolam acetazolamide Acetest acetic acid Acetocot acetohexamide acetophenazine Acetoxyl 10 Gel Acetoxyl 2.5 Gel Acetoxyl 20 Gel Acetoxyl 5 Gel acetylsalicylic acid Achromycin Achromycin V aciclovir Acid Control Acid Phos Fluor Rinse Acilac Aciphex acitretin Aclophen Aclovate Acne-10 Lotion Acne-5 Lotion Acne-Aid Aqua Gel Acne-Aid Gel Acne-Aid Vanishing Cream Acne Aid 10 Cream Acne Lotion 10 Acne Prone Skin Sunscreen Acne Wash Acno Acnomel -

Sheet1 Page 1 a Abamectin Acetazolamide Sodium Adenosine-5-Monophosphate Aklomide Albendazole Alfaxalone Aloe Vera Alphadolone A
Sheet1 A Abamectin Acetazolamide sodium Adenosine-5-monophosphate Aklomide Albendazole Alfaxalone Aloe vera Alphadolone Acetate Alpha-galactosidase Altrenogest Amikacin and its salts Aminopentamide Aminopyridine Amitraz Amoxicillin Amphomycin Amphotericin B Ampicillin Amprolium Anethole Apramycin Asiaticoside Atipamezole Avoparcin Azaperone B Bambermycin Bemegride Benazepril Benzathine cloxacillin Benzoyl Peroxide Benzydamine Bephenium Bephenium Hydroxynaphthoate Betamethasone Boldenone undecylenate Boswellin Bromelain Bromhexine 2-Bromo-2-nitropan-1, 3 diol Bunamidine Buquinolate Butamisole Butonate Butorphanol Page 1 Sheet1 C Calcium glucoheptonate (calcium glucoheptogluconate) Calcium levulinate Cambendazole Caprylic/Capric Acid Monoesters Carbadox Carbomycin Carfentanil Carnidazole Carnitine Carprofen Cefadroxil Ceftiofur sodium Centella asiatica Cephaloridine Cephapirin Chlorine dioxide Chlormadinone acetate Chlorophene Chlorothiazide Chlorpromazine HCl Choline Salicylate Chondroitin sulfate Clazuril Clenbuterol Clindamycin Clomipramine Clopidol Cloprostenol Clotrimazole Cloxacillin Colistin sulfate Copper calcium edetate Copper glycinate Coumaphos Cromolyn sodium Crystalline Hydroxycobalamin Cyclizine Cyclosporin A Cyprenorphine HCl Cythioate D Decoquinate Demeclocycline (Demethylchlortetracycline) Page 2 Sheet1 Deslorelin Desoxycorticosterone Pivalate Detomidine Diaveridine Dichlorvos Diclazuril Dicloxacillin Didecyl dimethyl ammonium chloride Diethanolamine Diethylcarbamazine Dihydrochlorothiazide Diidohydroxyquin Dimethylglycine -

(12) Patent Application Publication (10) Pub. No.: US 2011/0159073 A1 De Juan Et Al
US 20110159073A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2011/0159073 A1 de Juan et al. (43) Pub. Date: Jun. 30, 2011 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA A6F 2/00 (2006.01) (US); Signe E. Varner, Los (52) U.S. Cl. ........................................................ 424/427 Angeles, CA (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Featured is a method for instilling one or more bioactive (21) Appl. No.: 12/981,038 agents into ocular tissue within an eye of a patient for the treatment of an ocular condition, the method comprising con (22) Filed: Dec. 29, 2010 currently using at least two of the following bioactive agent delivery methods (A)-(C): (A) implanting a Sustained release Related U.S. Application Data delivery device comprising one or more bioactive agents in a (63) Continuation of application No. 1 1/175,850, filed on posterior region of the eye so that it delivers the one or more Jul. 5, 2005, now abandoned. bioactive agents into the vitreous humor of the eye; (B) instill ing (e.g., injecting or implanting) one or more bioactive (60) Provisional application No. 60/585,236, filed on Jul. 2, agents Subretinally; and (C) instilling (e.g., injecting or deliv 2004, provisional application No. 60/669,701, filed on ering by ocular iontophoresis) one or more bioactive agents Apr. 8, 2005. into the vitreous humor of the eye. Patent Application Publication Jun. 30, 2011 Sheet 1 of 22 US 2011/O159073 A1 Patent Application Publication Jun. -

USP Endotoxin Limits for Common Injectables
Pharma&Biotech USP Endotoxin Limits for Common Injectables Updated as of August 2011 For reference use only Pharma&Biotech Updated as of August 2011. For reference use only. USP Endotoxin Limits This information is subject to the disclaimer included on page 13. for Common Injectables This table is for informational purposes only. Endotoxin limits should be set on an individual product basis, using the formula found in the Pharmacopeias (Endotoxin Limit = K/M). Description Endotoxin Limit A Acepromazine Maleate Injection 4.5 EU / mg Acetazolamide for Injection 0.5 EU / mg Acetic Acid Irrigation 0.5 EU / ml Acyclovir for Injection 0.174 EU / mg Adenosine Injection (continuous peripheral intravenous infusion) 5.95 EU / mg Adenosine Injection (rapid intravenous) 11.62 EU / mg Alcohol in Dextrose Injection 0.5 EU / ml Alfentanil Injection 10 EU / ml Alprostadil Injection 0.05 EU / µg Alteplase for Injection 1 EU / mg Amifostine for Injection 0.2 EU / mg Amikacin Sulfate Injection 0.33 EU / mg Aminocaproic Acid Injection 0.05 EU / mg Aminohippurate Sodium Injection 0.04 EU / mg Aminopentamide Sulfate Injection 25 EU / mg Aminophylline Injection 1 EU / mg Ammonium Chloride Injection (of Chloride) 1.72 mEq Cl Amobarbital Sodium for Injection 0.4 EU / mg Amoxicillin, Sterile and Suspension 0.25 EU / mg Amphotericin B for Injection (for Intrathecal) 0.9 EU / mg Amphotericin B for Injection (for Parenterals) 5 EU / mg Ampicillin and Sulbactam for Injection 0.17 EU / (1 mg of mix of amp and sulb - 0.67 and 0.33 mg, respectively) Ampicillin for Injection -

Joint Injection Workshop
Joint Injection Workshop Dr Laurel Young Redcliffe and Northside Rheumatology (RNR) Joint injections • Indications • Type of steroid and why • Technique • Complications • Consent – verbal, written • Imaging? Indications for aspirating or injecting joints/soft tissues Reasons for joint aspirations Reasons for injections Exclude infection (mandatory) Diagnostic – eg. LA Therapeutic Diagnostic e.g crystals, (relieve symptoms) inflammation Joints, tendon sheaths, bursa, CTS What to inject? Type of steroid Duration in joint - solubility Corticosteroid Solubility Cost Betamethasone sodium phosphate Most soluble Dexamethasone sodium phosphate Soluble Prednisone sodium phosphate Soluble Methylprednisolone acetate Slightly soluble $4.72 (40mg/vial) Betamethasone sodium phosphate + Slightly soluble $5.34 Bethamethasone acetate (2.96/2.71mg/vial) Triamcinolone diacetate Slightly soluble Prednisolone tebutate Slightly soluble Trimancinolone acetonide Relatively insoluble $27.25 (10mg/vial) $81.39 (40mg/vial) Triamcinolone hexacetonide Relatively insoluble Hydrocortisone acetate Relatively insoluble Dexamethasone acetate Relatively insoluble Fluorinated vs non-fluorinated steroids Methylprednisolone acetate Triamcinolone acetonide Betamethasone Fluorinated steroids risk in s/c injections – fat necrosis, hypopigmentation Corticosteroid Fluorinated Betamethasone sodium phosphate Yes Betamethasone sodium Yes phosphoate/Betamethasone acetate Dexamethasone sodium phosphate Yes Triamcinolone diacetate Yes Trimancinolone acetonide Yes Triamcinolone hexacetonide -

Office Procedures Practice Makes Perfect
Office Procedures Practice Makes Perfect Anthony Luke MD, MPH, CAQ (Sport Med) Essentials of Primary Care 2015 Outline Injections Fracture care • Kinds of injections? • X-ray reading • Practical Tips for • Splinting and bracing Injections in the Office – Upper extremity – Lower extremity 1 Outline My take home tips on Injections: 1.Know your anatomy 2.Use both hands – sense of touch 3.Visualize things in 3D 4.Take your time Outline • Preparation • Landmarks • Common Injections 2 Case Who? 52 year old female, event manager, used to do karate What? L Knee Acute pain, locking and swelling When? Left greater than right knee pain x 7 yrs, after kicked in kneecap during karate; Re-injured 1 week ago How? Stepped off curb Where? Pain diffusely especially posterior Case LOOK 5’2”, 190 lbs • Large effusion FEEL • Tender over patella and medial > lateral joint line MOVE • ROM Left 10° to 105°; Right 0° to 140° SPECIAL TESTS • McMurray positive, pain with hyperflexion, Ligament stress tests negative 3 4 What to do? • 20 gauge needle • Aspirated 60 cc clear yellow fluid • Injected 5 cc 2% Xylocaine, 3cc 0.25% bupivicaine, 2cc Aristospan (Triamcinolone) • Patient pain free after injection • Told temporary relief only • Send fluid? • Refer to Orthopaedics to consider surgery (TKR?) Preparation Needles • 25 gauge – thinner, easier to insert, more resistance • 22 gauge – My preferred needle • 20 gauge – less resistance, easier to aspirate fluid Syringes • 3 – 10 mL syringe for injection • 20 – 60 mL syringe for aspiration 5 Preparation Solutions to be injected • If using bottles that will be used more than once, swab top with alcohol • Withdraw solution in proper order to avoid contamination of larger bottles “Prep” materials (or prep trays) • Betadine and gauze • Alcohol swabs • Bandaid +/- topical anesthetic (i.e. -
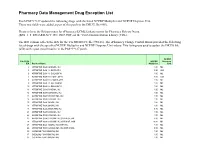
Pharmacy Data Management Drug Exception List
Pharmacy Data Management Drug Exception List Patch PSS*1*127 updated the following drugs with the listed NCPDP Multiplier and NCPDP Dispense Unit. These two fields were added as part of this patch to the DRUG file (#50). Please refer to the Release notes for ePharmacy/ECME Enhancements for Pharmacy Release Notes (BPS_1_5_EPHARMACY_RN_0907.PDF) on the VistA Documentation Library (VDL). The IEN column reflects the IEN for the VA PRODUCT file (#50.68). The ePharmacy Change Control Board provided the following list of drugs with the specified NCPDP Multiplier and NCPDP Dispense Unit values. This listing was used to update the DRUG file (#50) with a post install routine in the PSS*1*127 patch. NCPDP File 50.68 NCPDP Dispense IEN Product Name Multiplier Unit 2 ATROPINE SO4 0.4MG/ML INJ 1.00 ML 3 ATROPINE SO4 1% OINT,OPH 3.50 GM 6 ATROPINE SO4 1% SOLN,OPH 1.00 ML 7 ATROPINE SO4 0.5% OINT,OPH 3.50 GM 8 ATROPINE SO4 0.5% SOLN,OPH 1.00 ML 9 ATROPINE SO4 3% SOLN,OPH 1.00 ML 10 ATROPINE SO4 2% SOLN,OPH 1.00 ML 11 ATROPINE SO4 0.1MG/ML INJ 1.00 ML 12 ATROPINE SO4 0.05MG/ML INJ 1.00 ML 13 ATROPINE SO4 0.4MG/0.5ML INJ 1.00 ML 14 ATROPINE SO4 0.5MG/ML INJ 1.00 ML 15 ATROPINE SO4 1MG/ML INJ 1.00 ML 16 ATROPINE SO4 2MG/ML INJ 1.00 ML 18 ATROPINE SO4 2MG/0.7ML INJ 0.70 ML 21 ATROPINE SO4 0.3MG/ML INJ 1.00 ML 22 ATROPINE SO4 0.8MG/ML INJ 1.00 ML 23 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,5ML 5.00 ML 24 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,10ML 10.00 ML 25 ATROPINE SO4 1MG/ML INJ,AMP,1ML 1.00 ML 26 ATROPINE SO4 0.2MG/0.5ML INJ,AMP,0.5ML 0.50 ML 30 CODEINE PO4 30MG/ML -

MODEL CURRICULUM CERTIFIED MEDICATION AIDE TRAINING PROGRAM Ohio Board of Nursing October 2006
www.nursing.ohio.gov MODEL CURRICULUM CERTIFIED MEDICATION AIDE TRAINING PROGRAM Ohio Board of Nursing October 2006 CERTIFIED MEDICATION AIDE TRAINING PROGRAMS Certified medication aide training programs must comply with the statutory and regulatory requirements specified in Sections 4723.32 through 4723.91 of the Ohio Revised Code and Chapter 4723-27 of the Ohio Administrative Code and be approved by the Ohio Board of Nursing (Board). Among other requirements, the regulations require certified medication aide training programs to provide a curriculum of a minimum of 120 hours, including 80 hours of didactic/laboratory experience and 40 hours of supervised clinical experience. For the didactic and laboratory experience, the rules set forth required curriculum content and hours. This Model Curriculum complies with the curriculum requirements specified in Chapter 4723-27-08 of the Ohio Administrative Code (OAC). A certified medication aide training program may use the Model Curriculum, as written, use the Model Curriculum as a basis and expand upon the content and hours, or establish its own curriculum as long as it meets the requirements of OAC Chapter 4723-27-08. Those interested in becoming an approved certified medication aide training program, should review the requirements of Sections 4723.32 through 4723.91 of the Ohio Revised Code and OAC Chapter 4723-27. Specifically, OAC rules 4723-27-11 through 4723-27-14 provide the requirements for Pilot Program and the training programs, but interested parties should review the entire applicable statute and rules to be familiar with all of the requirements for certified medication aides, the Pilot Program, and training programs. -

Recent Advances in the Analysis of Steroid Hormones and Related Drugs
ANALYTICAL SCIENCES MAY 2004, VOL. 20 767 2004 © The Japan Society for Analytical Chemistry Reviews Recent Advances in the Analysis of Steroid Hormones and Related Drugs Sándor GÖRÖG Gedeon Richter Ltd., P.O.B. 27, H-1475 Budapest, Hungary The development during the last 15 years and the state-of-the-art in the analysis of bulk steroid hormone drugs and hormone-like structures and pharmaceutical formulations made thereof are summarized. Other steroids (sterols, bile acids, cardiac glycosides, vitamins D) as well as biological-clinical aspects and pharmacokinetic and metabolic studies are excluded from this review. The state-of-the-art is summarized based on comparisons of monographs in the latest editions of the European Pharmacopoeia, United States Pharmacopoeia and the Japanese Pharmacopoeia. This is followed by sections dealing with new developments in the methodology for the fields of spectroscopic and spectrophotometric, chromatographic, electrophoretic and hyphenated techniques as well electroanalytical methods. The review is terminated by two problem-oriented sections: examples on impurity and degradation profiling as well as enantiomeric analysis. (Received January 14, 2004; Accepted February 2, 2004) 1 Introduction 767 4·3 Supercritical fluid chromatography (SFC) 2 Steroid Hormone Drugs in Pharmacopoeias 768 4·4 High-performance liquid chromatography 2·1 Assay of bulk drug materials (HPLC) and HPLC-MS 2·2 Related impurities test of bulk drug materials 5 Electrophoretic and Related Methods 776 2·3 Assay of steroid hormone formulations -

Inflammation/Immunology
Inflammation/Immunology The diseases caused by disorders of the immune system fall into two broad categories: immunodeficiency and autoimmunity. Immunotherapy is also often used in the immunosuppressed (such as HIV patients) and people suffering from other immune deficiencies or autoimmune diseases. This includes regulating factors such as IL-2, IL-10, IFN-α. Infection with HIV is characterized not only by development of profound immunodeficiency but also by sustained inflammation and immune activation. Chronic inflammation as a critical driver of immune dysfunction, premature appearance of aging-related diseases, and immune deficiency. www.MedChemExpress.com 1 Inflammation/Immunology Inhibitors & Modulators (+)-Borneol (+)-DHMEQ ((1R,2R,6R)-Dehydroxymethylepoxyquinomicin; (d-Borneol) Cat. No.: HY-N1368A (1R,2R,6R)-DHMEQ) Cat. No.: HY-14645A Bioactivity: (+)-Borneol (d-Borneol) is a natural bicyclic monoterpene used Bioactivity: (+)-DHMEQ is an activator of antioxidant transcription factor for analgesia and anesthesia in traditional Chinese medicine; Nrf2. (+)-DHMEQ is the enantiomer of (-)-DHMEQ. (-)-DHMEQ enhances GABA receptor activity with an EC50 of 248 μM. inhibits NF-kB than its enantiomer (+)-DHMEQ. Purity: 98.0% Purity: 98.02% Clinical Data: No Development Reported Clinical Data: No Development Reported Size: 10mM x 1mL in DMSO, Size: 10mM x 1mL in DMSO, 100 mg 2 mg, 5 mg, 10 mg, 25 mg (-)-Epicatechin (-)-Ketoconazole ((-)-Epicatechol; Epicatechin; epi-Catechin) Cat. No.: HY-N0001 Cat. No.: HY-B0105B Bioactivity: (-)-Epicatechin inhibits cyclooxygenase-1 ( COX-1) with an Bioactivity: (-)-Ketoconazole is one of the enantiomer of Ketoconazole. Ketoconazole is a racemic mixture of two enantiomers, IC50 of 3.2 μM. (-)-Epicatechin inhibits the IL-1β-induced expression of iNOS by blocking the nuclear localization of the levoketoconazole ((2S,4R)-(−)-ketoconazole) and p65 subunit of NF-κB.