A Conversation with Errol Norwitz, MD, Phd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
MHA/ONL Patientcarelink Nursing-Sensitive Measure Report
MHA/ONL PatientCareLink Nursing-Sensitive Measure Report Statistical Appendix April 2016 April 2016 Statistical Appendix Contents Explanation of Analysis of the Statistical Significance of Hospital Measure Rates Acute Care Hospitals Bed-size Group Category Listing Specialty Hospital Listing Acute Care Hospitals o NSC-2 Pressure Ulcer Prevalence . Acute Care Hospital Bed-size Group Measure Data Graphs o NSC-3 Patient Falls . Acute Care Hospital Bed-size Group Measure Data Graphs o NSC-4 Falls with Injury . Acute Care Hospital Bed-size Group Measure Data Graphs Specialty Hospitals o NSC-2 Pressure Ulcer Prevalence . Rehabilitation Hospitals Group Measure Data Graphs . Long-term Acute Care Hospitals Group Measure Data Graphs o NSC-3 Patient Falls . Rehabilitation Hospitals Group Measure Data Graphs . Long-term Acute Care Hospitals Group Measure Data Graphs o NSC-4 Falls with Injury . Rehabilitation Hospitals Group Measure Data Graphs . Long-term Acute Care Hospitals Group Measure Data Graphs April 2016 MHA OCT 2007 Analysis of the Statistical Significance of Hospital Measure Rates Because the measure rates for the hospitals are for a specific period of time, and because there is variability in performance over time because of chance and other factors, there is a degree of uncertainty about the extent to which a hospital’s measure rate may reflect its true underlying performance. Without taking this uncertainty into account, we cannot conclude that a hospital with a measure rate that is higher or lower than the group rate is truly performing at a worse or better rate than the group. Statisticians use confidence intervals to account for this uncertainty. -

How to Find Us!
How To Find Us! FLOATING HOSPITAL FOR CHILDREN is easily accessible by car from the Massachusetts Turnpike (Route 90), the Central Artery and the Southeast Expressway (Route 93). The hospital is located in downtown Boston — in Chinatown and the Theater District — and within walking distance of the Boston Common, Downtown Crossing and many hotels and restaurants. The main entrance for patients and visitors at Tufts Medical Center is 800 Washington Street, Boston, MA 02111. Floating Hospital for Children is located at 755 Washington Street. Emergency services for adult as well as pediatric patients are located at the North Building, 830 Washington Street. Telephone driving directions are available by calling 617-636-5000, ext. 5 or visit www.tuftsmedicalcenter.org/directions. IF USING GPS for directions, we recommend you plug in the address of our from from 93 New Hampshire 95 New Hampshire parking garage: 274 Tremont Street, Boston, MA 02111. Be sure to include the zipcode. from and Maine Western MA 128 BY CAB AND TRAIN: The hospital is a 15-to-20-minute cab ride from Logan Airport 2 95 and within walking distance of South Station. 1 FROM THE NORTH (I-93 SOUTHBOUND): Logan TUFTS MEDICAL International ▶ Take Exit 20 A (South Station) onto Purchase Street. Continue along Purchase Street Airport from CENTER and FLOATING HOSPITAL (this becomes Surface Artery). New York FOR CHILDREN ▶ Turn right onto Kneeland Street. Go straight several blocks. 90 ▶ Turn left onto Tremont Street. Tufts Medical Center and Floating Hospital for Children Boston Harbor Garage is on your left, just past the Citi Performing Arts Center. -

Lawrence General Hospital
Massachusetts Hospital Payment Variation 2015 2016 Share of # Hospital Relative Relative Commercial MA Acute Hospital Commercial Relative Price (Weighted Average 2016) Price Price Payments Statewide Results Published By CHIA February 2018 1 Baystate Noble 0.681 0.682 0.2% Baystate Noble Hospital 2 Holyoke Medical Center 0.722 0.728 0.2% Holyoke Medical Center 3 Lawrence General 0.754 0.736 0.4% Lawrence General Hospital 4 Anna Jaques 0.756 0.743 0.5% Anna Jaques Hospital 5 Baystate Wing 0.749 0.752 0.2% Baystate Wing Hospital 6 Cambridge Health Alliance 0.797 0.754 0.6% Cambridge Health Alliance 7 BIDH - Milton 0.760 0.757 0.4% Beth Israel Deaconess- Milton 8 Massachusetts Eye & Ear 0.833 0.760 Massachusetts Eye & Ear 9 Heywood Hospital 0.752 0.763 0.4% Heywood Hospital 10 Signature Brockton 0.785 0.787 0.7% Signature Brockton Hospital 11 Mercy Medical Center 0.806 0.796 0.6% Mercy Medical Center 12 HealthAlliance 0.781 0.804 0.4% HealthAlliance Hospital 80% of Average 13 Emerson 0.846 0.824 1.1% Emerson Hospital 14 Steward Morton 0.855 0.837 0.4% Steward Morton Hospital 15 Milford Regional 0.840 0.840 1.1% Milford Regional Medical Center 16 Lowell General 0.822 0.850 1.6% Lowell General Hospital 85% of Average 17 Northeast Beverly 0.867 0.851 1.3% Northeast Hospital 18 MetroWest 0.856 0.853 1.0% MetroWest Medical Center 19 Steward Holy Family 0.859 0.857 0.7% Steward Holy Family Hospital 20 Winchester Hospital 0.892 0.865 1.6% Beth Israel Deaconess - Plymouth 21 BIDH - Plymouth 0.861 0.865 0.8% Winchester Hospital Underpaid Hospitals -
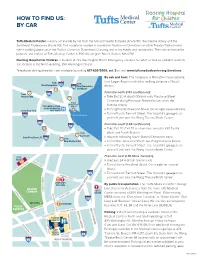
How to Find Us: by Car
HOW TO FIND US: BY CAR Tufts Medical Center is easily accessible by car from the Massachusetts Turnpike (Route 90), the Central Artery and the Southeast Expressway (Route 93). The hospital is located in downtown Boston—in Chinatown and the Theater District—and within walking distance of the Boston Common, Downtown Crossing and many hotels and restaurants. The main entrance for patients and visitors at Tufts Medical Center is 800 Washington Street, Boston, MA 02111. Floating Hospital for Children is located at 755 Washington Street. Emergency services for adult as well as pediatric patients are located at the North Building, 830 Washington Street. Telephone driving directions are available by calling 617-636-5000, ext. 5 or visit www.tuftsmedicalcenter.org/directions. By cab and train: The hospital is a 15-to-20-minute cab ride from Logan Airport and within walking distance of South from from New Hampshire 93 95 New Hampshire Station. 128 and Maine 2 From the north (I-93 southbound): from 95 Western MA » 1 Take Exit 20 A (South Station) onto Purchase Street. Continue along Purchase Street (this becomes the Logan International TUFTS MEDICAL CENTER Airport Surface Artery). & FLOATING HOSPITAL from New York FOR CHILDREN » Turn right onto Kneeland Street. Go straight several blocks. » Turn left onto Tremont Street. The hospital’s garage is on 90 Boston Harbor your left, just past the Wang Theatre/Boch Center. 95 From the south (I-93 northbound): 93 128 » Take Exit 20 (Exit 20 is a two-lane ramp for I-90 East & from West, and South Station). 3 Cape Cod from Providence, RI » Stay left, following South Station/Chinatown signs. -

PEDIATRIC Emergency Medicine
Newton-Wellesley Hospital’s HeaHealthSolthSoururcece Summer 2016 Family-centered Care Shark Bite on Spring Break Pediatric Emergency Medicine Programs & Classes “We were standing in the water getting ready to head back to the “I decided not to have surgery in Florida because it wasn’t urgent. beach when it felt like a bear trap grabbed the back of my foot. I was leaving the next day and decided I wanted to wait until I re- Right in the muscle,” says Dan. “I screamed and then took a couple turned to Boston to determine the best place to have the procedure.” steps to run when I felt something bite me again. With the second bite, the shark got my Achilles tendon so my leg gave out from When Dan returned to Massachusetts, he and his mom visited under me and I shouted, ‘I'm bit! I'm bit!’” Newton-Wellesley Hospital’s Emergency Department to determine his next steps. His care team in the ED recommended that he con- Dan managed to crawl out of the water and look at his ankle. sult an orthopaedic surgeon about the tear in his Achilles tendon There was a big gash across his Achilles down to the bone and his and the possibility of some of the shark tooth still being in his foot was limp. His friends carried him off the beach to get help. ankle, which they were able to see in an X-ray and MRI. “I almost fainted at that moment but didn't,” he says. “It started “After my trip to the Emergency Room my mom and I went to a to bleed like crazy but there was no pain; I guess I was in shock. -

MCPAP Family Brochure
MCPAP Regional Teams Connecting Primary Care Additional Services with Child Psychiatry Regional MCPAP teams consist of child The Triple P Positive Parenting Program is psychiatrists, licensed therapists, care available to parents at the MCPAP office (and coordinators, and appropriate administrative some PCP offices) by support. Some teams also have an Advanced referral from your Practice Registered Nurse (APRN). child’s PCP. Triple P gives parents tips to help them handle Western Massachusetts challenges with their Baystate Medical Center children’s behaviors. Some of these behaviors MCPAP for Moms is a program to help Central Massachusetts might include temper tantrums, bedtime, women who are pregnant, or have just given University of Massachusetts mealtime or chore struggles, bullying, birth, with depression and other mental health homework, and other concerns. The Triple P concerns. Screening new mothers for Medical Center provider will meet with parents two to four depression is an important part of well-baby Northeast Region times. These meetings can help make being visits. Your mental health affects the healthy North Shore Medical Center a parent less stressful and more enjoyable. development of your baby and family. If you are a new mom and have concerns about Boston/Metro Region I your emotional well-being you Massachusetts General Hospital should talk to your baby’s PCP. Boston/Metro Region II S/he will help you coordinate Tufts Medical Center/ with your own PCP to access the services of Boston Children’s Hospital MCPAP for Moms. Southeast Region You can find more McLean Hospital - Southeast information at mcpapformoms.org on the “For Mothers We work with your child’s Please visit our website: www.mcpap.org and Families” tab. -

First Do No Harm
WINTER 2021 ` First Do No Harm Quality and Patient Safety Division, Massachusetts Board of Registration in Medicine Message from QPSD Leadership Julian N. Robinson, MD Daniela Brown, MSN, RN, CIC Chairperson, QPS Committee Director, QPS Division Dear Colleagues, As we navigate through a second surge of the pandemic, the disproportionate impact In This Issue being experienced by minorities and people of color continues to be evident. Long- standing health and social inequities have put racial, ethnic, and LGBTQ minority groups at higher risk of serious illness and death related to Covid 19. In order to combat these 1 Message from QPS inequities, barriers such as lack of access to care, poverty, food insecurity, and discrimination must be identified and acted upon. Leadership 2 QPS Committee member The Quality and Patient Safety Division (QPSD) has asked several of the hospitals that Ziad Alfarah, MD report to us to share some of the programs that they have implemented to address the inequities in healthcare. Many organizations are attempting to close that gap by 3 Cambridge Health Alliance addressing the social, physical and economic conditions that impact health. We Hospital encourage all hospitals and ambulatory clinics to continue to share their efforts with us 4 Massachusetts General through their reporting. QPS Committee member, Dr. Ziad Alfarah also shares his thoughts Hospital on the changes that we individually can make in the fight against racism. 5 McLean Hospital The QPSD is mindful of the ongoing toll the pandemic has taken on hospitals and 6 Tufts Medical Center ambulatory clinics in the Commonwealth. In 2020, we attempted to reduce the burden 7 Update: Reporting to QPSD related to reporting by excusing the spring annual and semi-annual reports and making the fall semi-annual report and select SQRs optional. -

How to Find Us!
How To Find Us! Tufts Medical Center and Floating Hospital for Children are easily accessible by car from the Massachusetts Turnpike (Route 90), the Central Artery and the Southeast Expressway (Route 93). The hospitals are located in downtown Boston, in Chinatown and the Theater District and within walking distance of the Boston Common, Downtown Crossing and many hotels and restaurants. The main entrance for patients and visitors at Tufts Medical Center is 800 Washington Street. Floating Hospital for Children is located at 735 Washington Street. Emergency services for adult as well as pediatric patients are located at the North Building, 830 Washington Street. FROM THE NORTH (I-93 SOUTHBOUND): from from 93 New Hampshire 95 New Hampshire ▶ Take Exit 20 A (South Station) onto Purchase Street. Continue along Purchase Street from and Maine Western MA 128 (this becomes Surface Artery). 2 95 ▶ Turn right onto Kneeland Street. Go straight several blocks. 1 ▶ Turn left onto Tremont Street. Tufts Medical Center and Floating Hospital for Children Logan Garage is on your left, just past the Citi Performing Arts Center. TUFTS MEDICAL International Airport from CENTER and FLOATING HOSPITAL FROM THE SOUTH (I-93 NORTHBOUND): New York FOR CHILDREN 90 ▶ Take Exit 20 (Exit 20 is a two-lane ramp for I-90 East & West, and South Station). ▶ Stay left, following South Station/Chinatown signs. Boston Harbor 95 93 ▶ Turn left on Kneeland Street. Go straight several blocks. ▶ Turn left onto Tremont Street. Tufts Medical Center and Floating Hospital for Children 128 Garage is on your left, just past the Citi Performing Arts Center. -

2019 Community Health Needs Assessment
2019 Community Health Needs Assessment 0 Mission Statement Tufts Medical Center (Tufts MC) is committed to improving the health and wellbeing of the communities we serve. As part of that mission, Tufts MC strives to reduce both health disparities and health inequities in those communities. We seek to identify current and emerging health needs, collaborate with community partners, provide culturally and linguistically appropriate health services and resources, and address community health needs through education, prevention, and treatment. Background The Medical Center is committed not only to its role in providing the highest quality care to its patients and their families, but also to its role as an anchor institution in Boston. In addition to the life-saving care that takes place within its walls, Tufts Medical Center supports impactful work in its partner communities. That work is guided by the findings of our triennial Community Health Needs Assessment (CHNA). In order to ensure that Tufts MC remains at the forefront of the effort to improve the health of community members, we must understand what issues and systems most affect the health of these communities. To that end, the CHNA is an opportunity to engage community members and to seek their input to inform our efforts over the ensuing three years. With an emphasis on the Boston neighborhoods of Chinatown, Dorchester, South Boston, and the South End, as well as the City of Quincy and the Greater Boston Asian community, Tufts MC combines the invaluable insights and contributions offered by community members with an analysis of available public health data in order to identify health priorities in each of these communities. -

NOTICE of PUBLIC HEARING Notice Is Hereby Given That a Public
(Notice date: December 21, 2018; 2:00pm) NOTICE OF PUBLIC HEARING Notice is hereby given that a public hearing will be conducted by the Massachusetts Development Finance Agency (“MDFA”) on January 8, 2019, at 10:00 a.m. at its offices located at 99 High Street, Boston, Massachusetts. If MDFA’s offices are closed on January 8, 2019 due to unforeseen circumstances, including adverse weather conditions, the public hearing will be held on the next business day on which MDFA’s offices are open at the same time and location. The purpose of the hearing will be the proposed issuance of qualified 501(c)(3) bonds, as defined in Section 145 of the Internal Revenue Code of 1986, as amended, in an aggregate principal amount not to exceed $376,000,000 (the “Bonds”), for a plan of financing for Wellforce, Inc. (“Wellforce”) to finance and refinance healthcare facilities owned and/or operated or to be owned and/or operated by Wellforce or its affiliates described herein and related working capital expenditures, including costs of issuance, at the addresses noted herein, including, but not limited to: I. Financing new costs of healthcare facilities in an overall aggregate principal amount not to exceed $118,000,000 and to be allocated in whole or in part, at one or more of the locations in Massachusetts as follows: A. Construction, renovation, improvement and equipping of healthcare facilities for Tufts Medical Center, Inc. (“TMC”) each located on the main campus of Tufts Medical Center, the principal address of which is 800 Washington Street, Boston -

Massachusetts Contracted Hospitals Community Health Centers (Chcs)
Massachusetts Contracted Hospitals Community Health Centers (CHCs) Addison Gilbert Hospital, Gloucester Massachusetts Eye and Ear Infirmary, Boston Boston Health Care for the Homeless Program, Boston Hilltown CHC, (2 locations) Worthington, Huntington Anna Jaques Hospital, Newburyport Massachusetts General Hospital, Boston Bowdoin Street CHC, Dorchester Holyoke Health Center, Holyoke Athol Memorial Hospital, Athol Melrose-Wakefield Hospital, Melrose Brockton Neighborhood Health Center, (2 locations) Island Health Care, Edgartown Baystate Medical Center, Springfield Mercy Medical Center, Springfield Brockton Lowell CHC, Lowell Baystate Noble Hospital, Westfield MetroWest Medical Center (Framingham Union Hospital), Brookside CHC, Jamaica Plain Lynn CHC, (2 locations) Lynn Baystate Wing Hospital (Wing Memorial Hospital), Palmer Framingham Cambridge Health Alliance Health Centers, Manet CHC, (5 locations) Quincy (3), Hull, Taunton (4 locations) Cambridge, Somerville, Malden, Revere Berkshire Medical Center, Pittsfield Metrowest Medical Center (Leonard Morse Hospital), Natick Mattapan CHC, Mattapan Caring Health Center, (3 locations) Springfield Beth Israel Deaconess Hospital - Milton (Milton Hospital), Milford Regional Medical Center, Milford MGH Charlestown Health Care Center, Charlestown Milton Morton Hospital, Taunton Charles River Community Health, (2 locations) Brighton, Waltham MGH Chelsea Health Care Center, Boston Beth Israel Deaconess Hospital - Needham, Needham Mount Auburn Hospital, Cambridge Chicopee Health Center, Chicopee MGH -

Healthy Futures
Working together for Healthy Futures A MAGAZINE FOR REFERRING PHYSICIANs FALL 2013 A new team for kids with GI and nutrition challenges 3 4 PLUS Developmental Screening 3 Pediatric Gastroenterology 4 Pediatric Psychiatry 6 6 The principal pediatric teaching hospital for Tufts University School of Medicine A LETTER FROM JOHN SCHREIBER, MD Dear Physicians, Typically I use this space in Healthy Futures to talk about why I think Floating Hospital for Children at Tufts Medical Center is an incredibly special place worthy of your referrals. But this time I’d like to allow some of our patients and their parents speak for themselves. Below are some comments from our families posted on Floating Hospital’s Facebook page. By the way, if you’d like to keep up with what’s happening at Floating Hospital, “liking” our Facebook page is a great way to connect. And you can always get in touch with me at jschreiber@ tuftsmedicalcenter.org or 617-636-8031. All the best, John Schreiber, MD, MPH Pediatrician-in-Chief, Chief Administrative Officer Floating Hospital for Children at Tufts Medical Center Chairman, Department of Pediatrics Tufts University School of Medicine My 6 month old is preparing for his second surgery at Floating Hospital. Both are minor surgeries, but I would absolutely recommend Floating for any procedure. We travel from Taunton to Floating for almost everything with our twins. Well worth the drive. Everyone has been wonderful & SO supportive!” Our 7 year old son has had 6 surgeries at the Floating I’m a new patient at Floating, but I just love them.