Issues in Endocrinology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bronson Healthcare Midwest Epic Review of Systems 10.3
Bronson HealthCare Midwest Epic Review of Systems 10.3 Constitution Endocrine Activity Change Y N Cold intolerance Y N Appetite Change Y N Heat intolerance Y N Chills Y N Polydipsia Y N Diaphoresis Y N Polyuria Y N Fatigue Y N GU Fever Y N Difficulty urinating Y N Unexpctd wt chnge Y N Dyspareunia Y N HENT Dysuria Y N Facial Swelling Y N Enuresis Y N Neck pain Y N Flank pain Y N Neck stiffness Y N Frequency Y N Ear Discharge Y N Genital Sore Y N Hearing loss Y N Hematuria Y N Ear pain Y N Menstrual problem Y N Tinnitus Y N Pelvic pain Y N Nosebleeds Y N Urgency Y N Congestion Y N Urine decreased Y N Rhinorrhea Y N Vaginal bleeding Y N Postnasal drip Y N Vaginal discharge Y N Sneezing Y N Vaginal pain Y N Sinus Pressure Y N Musc Dental problem Y N Arthralgias Y N Drooling Y N Back pain Y N Mouth sores Y N Gait problem Y N Sore throat Y N Joint swelling Y N Trouble swallowing Y N Myalgias Y N Voice Change Y N Skin Eyes Color change Y N Eye Discharge Y N Pallor Y N Eye itching Y N Rash Y N Eye pain Y N Wound Y N Last Name: ___________________________________ First Name: ______________________________________ Date of Birth: _____________________________ Today’s Date: __________________________________________ Bronson HealthCare Midwest Epic Review of Systems 10.3 Eye redness Y N Allergy/Immuno Photophobia Y N Env allergies Y N Visual disturbance Y N Food Allergies Y N Respiratory Immunocompromised Y N Apnea Y N Neurological Chest tightness Y N Dizziness Y N Choking Y N Facial asymmetry Y N Cough Y N Headaches Y N Shortness of breath Y N Light-headedness -

Modified Heller´S Esophageal Myotomy Associated with Dor's
Crimson Publishers Research Article Wings to the Research Modified Heller´s Esophageal Myotomy Associated with Dor’s Fundoplication A Surgical Alternative for the Treatment of Dolico Megaesophagus Fernando Athayde Veloso Madureira*, Francisco Alberto Vela Cabrera, Vernaza ISSN: 2637-7632 Monsalve M, Moreno Cando J, Charuri Furtado L and Isis Wanderley De Sena Schramm Department of General Surgery, Brazil Abstracts The most performed surgery for the treatment of achalasia is Heller´s esophageal myotomy associated or no with anti-reflux fundoplication. We propose in cases of advanced megaesophagus, specifically in the dolico megaesophagus, a technical variation. The aim of this study was to describe Heller´s myotomy modified by Madureira associated with Dor´s fundoplication as an alternative for the treatment of dolico megaesophagus,Materials and methods: assessing its effectiveness at through dysphagia scores and quality of life questionnaires. *Corresponding author: proposes the dissection ofTechnical the esophagus Note describing intrathoracic, the withsurgical circumferential procedure and release presenting of it, in the the results most of three patients with advanced dolico megaesophagus, operated from 2014 to 2017. The technique A. V. Madureira F, MsC, Phd. Americas Medical City Department of General extensive possible by trans hiatal route. Then the esophagus is retracted and fixed circumferentially in the Surgery, Full Professor of General pillars of the diaphragm with six or seven point. The goal is at least on the third part of the esophagus, to achieveResults: its broad mobilization and rectification of it; then is added a traditional Heller myotomy. Submission:Surgery At UNIRIO and PUC- Rio, Brazil Published: The mean dysphagia score in pre-op was 10points and in the post- op was 1.3 points (maximum October 09, 2019 of 10 points being observed each between the pre and postoperative 8.67 points, 86.7%) The mean October 24, 2019 hospitalization time was one day. -

The Association Between Hypocalcemia and Outcome in COVID-19 Patients: a Retrospective Study
The Association Between Hypocalcemia and Outcome in COVID-19 Patients: a Retrospective Study Bhagwan Singh Patidar All India Institute of Medical Sciences Tapasyapreeti Mukhopadhayay All India Institute of Medical Sciences Arulselvi Subramanian ( [email protected] ) All India Institute of Medical Sciences https://orcid.org/0000-0001-7797-6683 Riicha Aggarwal All India Institute of Medical Sciences Kapil Dev Soni All India Institute of Medical Sciences Neeraj Nischal All India Institute of Medical Sciences Debasis Sahoo All India Institute of Medical Sciences Surbhi Surbhi All India Institute of Medical Sciences Ravindra Mohan Pandey All India Institute of Medical Sciences Naveet Wig All India Institute of Medical Sciences Rajesh Malhotra All India Institute of Medical Sciences Anjan Trikha All India Institute of Medical Sciences Research Article Keywords: Calcium, Coronavirus, Laboratory parameters, Mortality, NLR, Pandemic Posted Date: March 16th, 2021 DOI: https://doi.org/10.21203/rs.3.rs-302159/v1 Page 1/14 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 2/14 Abstract Background: Calcium has been shown to have a vital role in the pathophysiology of SARS-CoV and MERS-CoV diseases but less is known about hypocalcemia in COVID-19 patients and its association with the disease severity and the nal outcome. Therefore, this study was conducted with an aim to assess the clinical features in the COVID-19 patients having hypocalcemia and to observe its impact on COVID- 19 disease severity and nal outcome. Method: In this retrospective study, consecutive COVID-19 patients of all age groups were enrolled. -

W10: Causes and Co-Morbidities of Nocturia Workshop Chair: An-Sofie Goessaert, Belgium 12 September 2017 09:00 - 10:30
W10: Causes and Co-morbidities of Nocturia Workshop Chair: An-Sofie Goessaert, Belgium 12 September 2017 09:00 - 10:30 Start End Topic Speakers 09:00 09:20 Phenotyping Nocturia – Judge a Book by its Cover? An-Sofie Goessaert 09:20 09:40 Sleep and Nocturia – Central Mechanisms into Business? Karlien Dhondt 09:40 10:00 Bladder and Kidney – Making the Bladder Gladder or Lowering Philip Van Kerrebroeck the Water Levels? 10:00 10:20 Questionnaire on Nocturia – to TANGO or Not to TANGO? Wendy Bower 10:20 10:30 Questions All Speaker Powerpoint Slides Please note that where authorised by the speaker all PowerPoint slides presented at the workshop will be made available after the meeting via the ICS website www.ics.org/2017/programme Please do not film or photograph the slides during the workshop as this is distracting for the speakers. Aims of Workshop Nocturia is a highly prevalent condition affecting both men and women of all ages. It is no longer a problem merely attributed to overactive bladder or benign prostate hyperplasia. There can be an impairment in one or more factors of the triad brain-kidney- bladder but also other factors such as obesity, hypertension, peripheral edema, sleep disturbance, depression, medication, etc can play a role. The objective of this workshop is to provide an overview on causes and co-morbidities of nocturia and how to identify them. Learning Objectives This workshop should allow the attendant to know the answers to following questions: 1. What physical features can help you to identify possible causes or co-morbidities of nocturia? 2. -

Clinical Physiology Aspects of Chloremia in Fluid Therapy: a Systematic Review David Astapenko1,2* , Pavel Navratil2,3, Jiri Pouska4,5 and Vladimir Cerny1,2,6,7,8,9
Astapenko et al. Perioperative Medicine (2020) 9:40 https://doi.org/10.1186/s13741-020-00171-3 REVIEW Open Access Clinical physiology aspects of chloremia in fluid therapy: a systematic review David Astapenko1,2* , Pavel Navratil2,3, Jiri Pouska4,5 and Vladimir Cerny1,2,6,7,8,9 Abstract Background: This systematic review discusses a clinical physiology aspect of chloride in fluid therapy. Crystalloid solutions are one of the most widely used remedies. While generally used in medicine for almost 190 years, studies focused largely on their safety have only been published since the new millennium. The most widely used solution, normal saline, is most often referred to in this context. Its excessive administration results in hyperchloremic metabolic acidosis with other consequences, including higher mortality rates. Methods: Original papers and review articles eligible for developing the present paper were identified by searching online in the electronic MEDLINE database. The keywords searched for included hyperchloremia, hypochloremia, and compound words containing the word “chloride,” infusion therapy, metabolic acidosis, renal failure, and review. Results: A total of 21,758 papers published before 31 May 2020 were identified; of this number, 630 duplicates were removed from the list. Upon excluding articles based on their title or abstract, 1850 papers were screened, of which 63 full-text articles were assessed. Conclusions: According to the latest medical concepts, dyschloremia (both hyperchloremia and hypochloremia) represents a factor indisputably having a negative effect on selected variables of clinical outcome. As infusion therapy can significantly impact chloride homeostasis of the body, the choice of infusion solutions should always take into account the potentially adverse impact of chloride content on chloremia and organ function. -

Dieulafoy's Lesion Associated with Megaesophagus
vv ISSN: 2455-2283 DOI: https://dx.doi.org/10.17352/acg CLINICAL GROUP Received: 21 September, 2020 Case Report Accepted: 06 October, 2020 Published: 07 October, 2020 *Corresponding author: Valdemir José Alegre Salles, Dieulafoy’s Lesion Associated Assistant Doctor Profesor, Department of Medicine, University of Taubaté, Brazil, Tel: +55-15-12-3681-3888; Fax: +55-15-12-3631-606; E-mail: with Megaesophagus Keywords: Dieulafoy’s lesion; Esophageal Valdemir José Alegre Salles1,2*, Rafael Borges Resende3, achalasia; Haematemesis; Endoscopic hemoclip; Gastrointestinal bleeding 3 2,4 Gustavo Seiji , and Rodrigo Correia Coaglio https://www.peertechz.com 1Assistant Doctor Profesor, Department of Medicine, University of Taubaté, Brazil 2General Surgeon at the Regional Hospital of Paraíba Valley, Taubaté, Brazil 3Endoscopist Physician at the Regional Hospital of Paraíba Valley, Taubaté, Brazil 4Assistant Profesor, Department of Medicine, University of Taubaté, Brazil A 31-years-old male patient, with no previous symptoms, admitted to the ER with massive hematemesis that started about 2 hours ago and already with hemodynamic repercussions. After initial care with clinical management for compensation, and airway protection (intubation) he underwent esophagogastroduodenoscopy (EGD), which was absolutely inconclusive due to the large amount of solid food remains and clots already in the proximal esophagus with increased esophageal gauge. After a 24 hours fasting, and 3 inconclusive EGD, since we don’t have the availability of an overtube, we decided to use a calibrated esophageal probe (Levine 22) and to maintain lavage and aspiration of the contents, until the probe returned clear. In this period, the patient presented several episodes of hematimetric decrease and melena, maintaining hemodynamic stability with intensive clinical support. -

A 27-Month-Old Boy with Polyuria and Polydipsia
UC Davis UC Davis Previously Published Works Title A 27-Month-Old Boy with Polyuria and Polydipsia. Permalink https://escholarship.org/uc/item/8x24x4p2 Authors Lee, Yvonne Winnicki, Erica Butani, Lavjay et al. Publication Date 2018 DOI 10.1155/2018/4281217 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Hindawi Case Reports in Pediatrics Volume 2018, Article ID 4281217, 4 pages https://doi.org/10.1155/2018/4281217 Case Report A 27-Month-Old Boy with Polyuria and Polydipsia Yvonne Lee,1 Erica Winnicki,2 Lavjay Butani ,3 and Stephanie Nguyen 3 1Department of Pediatrics, Section of Endocrinology, Kaiser Permanente Oakland Medical Center, Oakland, CA, USA 2Department of Pediatrics, Section of Nephrology, University of California, San Francisco, San Francisco, CA, USA 3Department of Pediatrics, Section of Nephrology, University of California, Davis, Sacramento, CA, USA Correspondence should be addressed to Stephanie Nguyen; [email protected] Received 16 May 2018; Accepted 1 August 2018; Published 23 August 2018 Academic Editor: Anselm Chi-wai Lee Copyright © 2018 Yvonne Lee et al. )is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Psychogenic polydipsia is a well-described phenomenon in those with a diagnosed psychiatric disorder such as schizophrenia and anxiety disorders. Primary polydipsia is differentiated from psychogenic polydipsia by the lack of a clear psychotic disturbance. We present a case of a 27-month-old boy who presented with polyuria and polydipsia. Laboratory studies, imaging, and an observed water deprivation test were consistent with primary polydipsia. -

Polyphagia Ellen N
W0117-Section I (31-50).qxd 4/23/04 7:26 PM Page 124 CHAPTER • 34 Polyphagia Ellen N. Behrend olyphagia is the consumption of food in excess of and liver disease) lead to polyphagia by unknown mecha- normal caloric intake. Hunger and satiety and, conse- nisms. Secondary polyphagia can also be caused by certain P quently, feeding behavior are primarily controlled by drugs. certain regions in the central nervous system (CNS), but many factors affect the function of these areas. Thus polypha- gia can be classified as primary (i.e., a CNS abnormality) or HISTORY secondary (i.e., a systemic problem affecting the CNS). Secondary polyphagia is by far more common and usually is Any change in body weight is an important differentiating accompanied by clinical signs of the underlying disease. feature of the various causes of polyphagia (Figure 34-1). Determining whether weight gain or loss has occurred should Primary or drug-induced polyphagia typically results in weight be the first step in formulating a list of differential diagnoses gain, because nutrients are adequate and feeding is inappro- and a diagnostic plan. priately increased. Pathologic secondary polyphagia is more commonly associated with weight loss, because the nutrient supply usually does not meet physiologic demands. However, PHYSIOLOGY some causes, such as acromegaly, hypoglycemia caused by an insulinoma, sudden acquired retinal degeneration syndrome Food intake is controlled by a variety of factors, including gas- (SARDS), and hyperadrenocorticism (HAC), lead to weight trointestinal, environmental, and CNS phenomena. The CNS, gain. Physiologic polyphagia can result in weight gain (e.g., mainly the hypothalamus, controls eating behavior.The lateral pregnancy, growth) or maintenance of weight (e.g., lactation, hypothalamic nuclei represent the “feeding center”; their cold environment, increased exercise). -

Sudden Death in Eating Disorders
Vascular Health and Risk Management Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Sudden death in eating disorders Beatriz Jáuregui-Garrido1 Abstract: Eating disorders are usually associated with an increased risk of premature death Ignacio Jáuregui-Lobera2,3 with a wide range of rates and causes of mortality. “Sudden death” has been defined as the abrupt and unexpected occurrence of fatality for which no satisfactory explanation of the 1Department of Cardiology, University Hospital Virgen del Rocío, 2Behavioral cause can be ascertained. In many cases of sudden death, autopsies do not clarify the main Sciences Institute, 3Pablo de Olavide cause. Cardiovascular complications are usually involved in these deaths. The purpose of University, Seville, Spain this review was to report an update of the existing literature data on the main findings with respect to sudden death in eating disorders by means of a search conducted in PubMed. The most relevant conclusion of this review seems to be that the main causes of sudden death in eating disorders are those related to cardiovascular complications. The predictive value of the For personal use only. increased QT interval dispersion as a marker of sudden acute ventricular arrhythmia and death has been demonstrated. Eating disorder patients with severe cardiovascular symptoms should be hospitalized. In general, with respect to sudden death in eating disorders, some findings (eg, long-term eating disorders, chronic hypokalemia, chronically low plasma albumin, and QT intervals .600 milliseconds) must be taken into account, and it must be highlighted that during refeeding, the adverse effects of hypophosphatemia include cardiac failure. -

Megaesophagus in Congenital Diaphragmatic Hernia
Megaesophagus in congenital diaphragmatic hernia M. Prakash, Z. Ninan1, V. Avirat1, N. Madhavan1, J. S. Mohammed1 Neonatal Intensive Care Unit, and 1Department of Paediatric Surgery, Royal Hospital, Muscat, Oman For correspondence: Dr. P. Manikoth, Neonatal Intensive Care Unit, Royal Hospital, Muscat, Oman. E-mail: [email protected] ABSTRACT A newborn with megaesophagus associated with a left sided congenital diaphragmatic hernia is reported. This is an under recognized condition associated with herniation of the stomach into the chest and results in chronic morbidity with impairment of growth due to severe gastro esophageal reflux and feed intolerance. The infant was treated successfully by repair of the diaphragmatic hernia and subsequently Case Report Case Report Case Report Case Report Case Report by fundoplication. The megaesophagus associated with diaphragmatic hernia may not require surgical correction in the absence of severe symptoms. Key words: Congenital diaphragmatic hernia, megaesophagus How to cite this article: Prakash M, Ninan Z, Avirat V, Madhavan N, Mohammed JS. Megaesophagus in congenital diaphragmatic hernia. Indian J Surg 2005;67:327-9. Congenital diaphragmatic hernia (CDH) com- neonate immediately intubated and ventilated. His monly occurs through the posterolateral de- vital signs improved dramatically with positive pres- fect of Bochdalek and left sided hernias are sure ventilation and he received antibiotics, sedation, more common than right. The incidence and muscle paralysis and inotropes to stabilize his gener- variety of associated malformations are high- al condition. A plain radiograph of the chest and ab- ly variable and may be related to the side of domen revealed a left sided diaphragmatic hernia herniation. The association of CDH with meg- with the stomach and intestines located in the left aesophagus has been described earlier and hemithorax (Figure 1). -

Hyponatremia in Hepatic Cirrhosis Following Paracentesis
HYPONATREMIA IN HEPATIC CIRRHOSIS FOLLOWING PARACENTESIS William P. Nelson III, … , Jack D. Rosenbaum, Maurice B. Strauss J Clin Invest. 1951;30(7):738-744. https://doi.org/10.1172/JCI102487. Research Article Find the latest version: https://jci.me/102487/pdf HYPONATREMIA IN HEPATIC CIRRHOSIS FOLLOWING PARACENTESIS 1 By WILLIAM P. NELSON, III, JACK D. ROSENBAUM, AND MAURICE B. STRAUSS (From the Medical Service, Cushing Veterans Administration Hospital, Framingham, Mass.) (Submitted for publication January 15, 1951; accepted April 23, 1951) The retention of water without a physiologically modification of the Folin procedure (14); non-protein equivalent amount of sodium following abdominal nitrogen by micro-Kjeldahl with Nesslerization (15); and sodium and potassium by means of the Barclay internal paracentesis has been studied in two patients with standard flame photometer. Except where otherwise advanced cirrhosis of the liver. In each there de- noted, urine was collected over 24 hour periods and was veloped manifestations considered characteristic analyzed for chloride by the Volhard-Harvey method of sodium deficit, although there was no change in (16), for total nitrogen by the micro-Kjeldahl procedure the total body sodium at the time these appeared. (11), and for creatinine, sodium, and potassium by the methods employed for serum. Change in total body water Such retention of water in excess of salt, regularly (liters) was taken to equal change in weight (kilograms). observed when large external losses of salt and water are replaced with water alone (1-3), has CASE REPORTS AND RESULTS been noted in certain cases of heart failure and chronic renal disease (4-6) as well as in decom- Case I. -
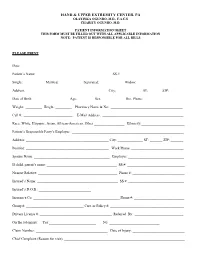
Patient Information Sheet This Form Must Be Filled out with All Applicable Information Note: Patient Is Responsible for All Bills
HAND & UPPER EXTREMITY CENTER, PA OLAYINKA OGUNRO, M.D., F.A.C.S CHARITY OGUNRO, M.D. PATIENT INFORMATION SHEET THIS FORM MUST BE FILLED OUT WITH ALL APPLICABLE INFORMATION NOTE: PATIENT IS RESPONSIBLE FOR ALL BILLS PLEASE PRINT Date: ________________________________________ Patient’s Name: _________________________________________ SS #: __________________________________ Single: __________ Married: ___________ Separated: ___________ Widow: ____________ Address: _____________________________________________ City: _____________ ST: ______ ZIP:________ Date of Birth: ___________________ Age:_________ Sex: ____________ Hm. Phone: ______________________ Weight: _________ Height: _________ Pharmacy Name & No: ________________________________________ Cell #: ___________________________ E-Mail Address: _____________________________________________ Race: White, Hispanic, Asian, African-American, Other _________________ Ethnicity:________________________ Patient’s Responsible Party’s Employer: ______________________________________________________________ Address: ______________________________________________ City: ______________ ST: _______ ZIP: _______ Position: ______________________________________________ Work Phone: _____________________________ Spouse Name: __________________________________________ Employer: _______________________________ If child, parent’s name: _______________________________________ SS #: ________________________________ Nearest Relative: ____________________________________________ Phone #: _____________________________