Patient Risks & Preparation for a Successful Sedation Or Anesthetic Event
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Zoletil 100 Injectable Anaesthetic/Sedative for Dogs, Cats, Zoo and Wild Animals
Zoletil 100 Injectable Anaesthetic/Sedative for Dogs, Cats, Zoo and Wild Animals Virbac (Australia) Pty Limited Chemwatch Hazard Alert Code: 1 Chemwatch: 6978267 Issue Date: 11/01/2019 Version No: 4.1.16.10 Print Date: 08/31/2021 Safety Data Sheet according to WHS Regulations (Hazardous Chemicals) Amendment 2020 and ADG requirements L.GHS.AUS.EN SECTION 1 Identification of the substance / mixture and of the company / undertaking Product Identifier Product name Zoletil 100 Injectable Anaesthetic/Sedative for Dogs, Cats, Zoo and Wild Animals Chemical Name Not Applicable Synonyms APVMA No.: 38837 Chemical formula Not Applicable Other means of identification Not Available Relevant identified uses of the substance or mixture and uses advised against Relevant identified uses For the anaesthesia and immobilisation of dogs, cats, zoo and wild animals. Details of the supplier of the safety data sheet Registered company name Virbac (Australia) Pty Limited Address 361 Horsley Road Milperra NSW 2214 Australia Telephone 1800 242 100 Fax +61 2 9772 9773 Website au.virbac.com Email [email protected] Emergency telephone number Association / Organisation Poisons Information Centre Emergency telephone 13 11 26 numbers Other emergency telephone Not Available numbers SECTION 2 Hazards identification Classification of the substance or mixture NON-HAZARDOUS CHEMICAL. NON-DANGEROUS GOODS. According to the WHS Regulations and the ADG Code. ChemWatch Hazard Ratings Min Max Flammability 1 Toxicity 1 0 = Minimum Body Contact 1 1 = Low 2 = Moderate Reactivity 1 3 = High Chronic 0 4 = Extreme Poisons Schedule S4 Classification [1] Not Applicable Label elements Hazard pictogram(s) Not Applicable Signal word Not Applicable Hazard statement(s) Not Applicable Precautionary statement(s) Prevention Not Applicable Precautionary statement(s) Response Not Applicable Precautionary statement(s) Storage Page 1 continued.. -
Download Product Insert (PDF)
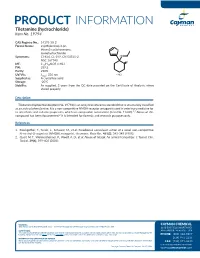
PRODUCT INFORMATION Tiletamine (hydrochloride) Item No. 19794 CAS Registry No.: 14176-50-2 Formal Name: 2-(ethylamino)-2-(2- thienyl)-cyclohexanone, S monohydrochloride Synonyms: CI-634, CL-399, CN 54521-2, HN NSC 167740 O MF: C12H17NOS • HCl FW: 259.8 Purity: ≥98% • HCl UV/Vis.: λmax: 236 nm Supplied as: A crystalline solid Storage: -20°C Stability: As supplied, 2 years from the QC date provided on the Certificate of Analysis, when stored properly Description Tiletamine (hydrochloride) (Item No. 19794) is an analytical reference standard that is structurally classified as an arylcyclohexylamine. It is a non-competitive NMDA receptor antagonist used in veterinary medicine for its anesthetic and sedative properties, which are comparable to ketamine (Item No. 11630).1,2 Abuse of this compound has been documented.2 It is intended for forensic and research purposes only. References 1. Klockgether, T., Turski, L., Schwarz, M., et al. Paradoxical convulsant action of a novel non-competitive N-methyl-D-aspartate (NMDA) antagonist, tiletamine. Brain Res. 461(2), 343-348 (1988). 2. Quail, M. T., Weimersheimer, P., Woolf, A. D., et al. Abuse of telazol: An animal tranquilizer. J. Toxicol. Clin. Toxicol. 39(4), 399-402 (2001). WARNING CAYMAN CHEMICAL THIS PRODUCT IS FOR RESEARCH ONLY - NOT FOR HUMAN OR VETERINARY DIAGNOSTIC OR THERAPEUTIC USE. 1180 EAST ELLSWORTH RD SAFETY DATA ANN ARBOR, MI 48108 · USA This material should be considered hazardous until further information becomes available. Do not ingest, inhale, get in eyes, on skin, or on clothing. Wash thoroughly after handling. Before use, the user must review the complete Safety Data Sheet, which has been sent via email to your institution. -

The Role of the N-Methyl-D-Aspartate Receptors in Social Behavior in Rodents
International Journal of Molecular Sciences Review The Role of the N-Methyl-D-Aspartate Receptors in Social Behavior in Rodents Iulia Zoicas * and Johannes Kornhuber Department of Psychiatry and Psychotherapy, University Hospital, Friedrich-Alexander-University Erlangen-Nuremberg, 91054 Erlangen, Germany; [email protected] * Correspondence: [email protected]; Tel.: +49-9131-85-46005; Fax: +49-9131-85-36381 Received: 8 October 2019; Accepted: 5 November 2019; Published: 9 November 2019 Abstract: The appropriate display of social behaviors is essential for the well-being, reproductive success and survival of an individual. Deficits in social behavior are associated with impaired N-methyl-D-aspartate (NMDA) receptor-mediated neurotransmission. In this review, we describe recent studies using genetically modified mice and pharmacological approaches which link the impaired functioning of the NMDA receptors, especially of the receptor subunits GluN1, GluN2A and GluN2B, to abnormal social behavior. This abnormal social behavior is expressed as impaired social interaction and communication, deficits in social memory, deficits in sexual and maternal behavior, as well as abnormal or heightened aggression. We also describe the positive effects of pharmacological stimulation of the NMDA receptors on these social deficits. Indeed, pharmacological stimulation of the glycine-binding site either by direct stimulation or by elevating the synaptic glycine levels represents a promising strategy for the normalization of genetically-induced, pharmacologically-induced or innate deficits in social behavior. We emphasize on the importance of future studies investigating the role of subunit-selective NMDA receptor ligands on different types of social behavior to provide a better understanding of the underlying mechanisms, which might support the development of selective tools for the optimized treatment of disorders associated with social deficits. -

Anesthetic and Physiologic Effects of Tiletamine, Zolazepam, Ketamine, and Xylazine Combination (TKX) in Feral Cats Undergoing Surgical Sterilization
Journal of Feline Medicine and Surgery (2004) 6, 297e303 www.elsevier.com/locate/jfms Anesthetic and physiologic effects of tiletamine, zolazepam, ketamine, and xylazine combination (TKX) in feral cats undergoing surgical sterilization Alexis M. Cistolaa, Francis J. Golderb, Lisa A. Centonzea, ) Lindsay W. McKaya, Julie K. Levya, aDepartment of Small Animal Clinical Sciences, PO Box 100126, College of Veterinary Medicine, University of Florida, Gainesville, FL 32610, USA bDepartment of Comparative Bioscience, College of Veterinary Medicine, University of Wisconsin, Madison, WI 53706, USA Revised 23 November 2003; accepted 26 November 2003 Summary Tiletamine (12.5 mg), zolazepam (12.5 mg), ketamine (20 mg), and xylazine (5mg)(TKX;0.25ml,IM)combinationwasevaluatedasananestheticin22maleand67 female adult feral cats undergoing sterilization at high-volume sterilization clinics. Cats were not intubated and breathed room air. Oxygen saturation (SpO2), mean blood pres- sure (MBP), heart rate (HR), respiration rate (RR), and core body temperature were re- corded. Yohimbine (0.25 ml, 0.5 mg, IV) was administered at the completion of surgery. TKXproducedrapidonsetoflateralrecumbency(4G1 min) and surgical anesthesia of sufficient duration to complete surgical procedures in 92% of cats. SpO2 measured via a lingual pulse oximeter probe averaged 92G3% in male cats and 90G4% in females. SpO2 fell below 90% at least once in most cats. MBPmeasuredbyoscillometryaveraged 136G30 mm Hg in males and 113G29 mm Hg in females. MBP increased at the onset of surgical stimulation suggesting incomplete anti-nociceptive properties. HR averaged 156G19bpm,andRRaveraged18G8 bpm. Neither parameter varied between males and females or over time. Body temperature decreased significantly over time, declining to 38.0G0.8 (C at the time of reversal in males and 36.6G0.8 (Catthetimeofreversal in females. -

21 CFR Ch. II (4–1–10 Edition) § 1308.12
§ 1308.12 21 CFR Ch. II (4–1–10 Edition) Some trade and other names: N,N- whenever the existence of such salts, Diethyltryptamine; DET isomers, and salts of isomers is possible (18) Dimethyltryptamine ................................................. 7435 Some trade or other names: DMT within the specific chemical designa- (19) 5-methoxy-N,N-diisopropyltryptamine (other tion: name: 5-MeO-DIPT) ................................................... 7439 (1) gamma-hydroxybutyric acid (some other names in- (20) Ibogaine .................................................................. 7260 clude GHB; gamma-hydroxybutyrate; 4- Some trade and other names: 7-Ethyl- hydroxybutyrate; 4-hydroxybutanoic acid; sodium 6,6b,7,8,9,10,12,13-octahydro-2-methoxy-6,9- oxybate; sodium oxybutyrate) .................................... 2010 methano-5H-pyrido [1′, 2′:1,2] azepino [5,4-b] (2) Mecloqualone ........................................................... 2572 indole; Tabernanthe iboga (3) Methaqualone ........................................................... 2565 (21) Lysergic acid diethylamide ..................................... 7315 (22) Marihuana .............................................................. 7360 (f) Stimulants. Unless specifically ex- (23) Mescaline ............................................................... 7381 cepted or unless listed in another (24) Parahexyl—7374; some trade or other names: 3- schedule, any material, compound, Hexyl-1-hydroxy-7,8,9,10-tetrahydro-6,6,9-trimethyl- 6H-dibenzo[b,d]pyran; Synhexyl. mixture, -

Advisory Council on the Misuse of Drugs Chair: Professor Les Iversen Secretary: Rachel Fowler 3Rd Floor Seacole Building 2
ACMD Advisory Council on the Misuse of Drugs Chair: Professor Les Iversen Secretary: Rachel Fowler 3rd Floor Seacole Building 2. Marsham Street London SW1P 4DF 020 7035 0454 Email: [email protected] Rt Hon. Theresa May MP Home Office 2 Marsham Street London SW1P 4DF 18th October 2012 Dear Home Secretary, In March 2012 the ACMD advised that methoxetamine be subject to a temporary class drug order. Methoxetamine was marketed as a legal alternative to ketamine until a temporary class drug order was implemented in April 2012. As is now required, the ACMD has followed its initial assessment with a consideration of methoxetamine in the context of the Misuse of Drugs Act 1971; I enclose the report with this letter. The chemical structure of methoxetamine bears a close resemblance to that of both ketamine and phencyclidine (PCP, „Angel Dust‟, a class A drug), which both produce well- documented and serious adverse effects following both acute and chronic usage. Users report that the effects of methoxetamine are similar to those of ketamine, however, some users report that the effects are of longer duration.The harmful effects reported include severe dissociation, cardiovascular symptoms, paranoid thoughts and unpleasant hallucinations. The first analytically confirmed series reported by Guy‟s and St Thomas‟ NHS Foundation Trust, London in 2011, was of three individuals who presented having self-reported use of methoxetamine. All three presented with a ketamine-like dissociative state, but also had significant stimulant effects with agitation and cardiovascular effects including tachycardia and hypertension. Toxicological screening of serum samples confirmed methoxetamine use in two of the cases. -

Outline for Controlled Substances Program
Environmental Health and Safety Controlled Substances Program Date of Issuance: Review Date: 10/1/2019 (no changes) 10/01/2018 Revision Number: Initial Prepared by: EH&S Table of Contents HEADINGS Introduction Applicability Responsibilities Registration Requirements Authorized Use Ordering/Purchasing Administering and Dispensing Inventory Procedures (Continuing Records) Security Disposal FORMS: Registering or renewing a DEA or state license (CMU) Controlled Substances Authorized users list (CMU) Employee questionnaire for those with access to controlled substances (CMU) Record of Form 222 use (Order form) (CMU) Records of Controlled Substance Purchases (CMU) Record of Controlled Substance Administering and dispensing (CMU) Controlled Substance Physical Inventory (CMU) DEA Registration of Persons doing research or analysis (Form 225) DEA Registration of Dispensers (Form 224) DEA Registration Instructional (Form 224 and 226 to renew) DEA Report of loss or theft (Form 106) DEA Report of drugs surrendered (From 41) DEA SCHEDULES: Schedule I Schedule II Schedule III Schedule IV Schedule V INTRODUCTION State and Federal regulations have been promulgated concerning the use and handling of US Department of Justice Drug Enforcement Administration (DEA) controlled substances. These regulations are in place to address materials which are or have the potential to be addictive or habit forming. These substances have been categorized into “schedules” that have been created by the DEA to reflect their level of concern. The “Carnegie Mellon University DEA Controlled Substances Program” is intended to ensure that Carnegie Mellon University is in compliance with our regulatory requirements. Required activities under the DEA include: 1. Registration of your work with the DEA and with Carnegie Mellon’s Department of Environmental Health and Safety (EH&S). -

Tiletamine-Hcl and the Tranquilizer Zolazepam- S Hcl
788 Reports Investigative Ophthalmology October 1975 CI-744 anesthesia for ophthalmological ex- 0 CH3 CH3 amination and surgery in monkeys. PAUL L. KAUFMAN AND RUDOLPH HAHNEN- C2H5 BERCER. CI-744 is a new agent for chemical restraint H and surgical anesthesia in animals, consisting of equal parts hy weight of the cataleptoid agent tiletamine-HCl and the tranquilizer zolazepam- S HCl. We have used it in the intramuscular dose V of five to ten milligrams per kilogram to anes- thetize 110 cynomolgus ami 10 vervet monkeys a total of 1,500 times for various ophthalmological procedures. At these dosages its characteristics of TILETAMINE 2OLAZEPAM action were rapid onset, thirty to fifty minutes of (Cl 634) (Cl 716) surgical depth anesthesia during which there was excellent muscular relaxation and an absence of Fig. 1. Components of CI-744. CI-744 is a 1:1 mixture by weight of tiletamine-HCl (CI-634) ocular movements, a very gradual emergence, and and zolazepam-HCl (CI-716). no adverse after effects. In these monkey species, we judge CI-744 superior to phencyclidine or methohexital as a short-acting general anesthetic CI-744 (5 mg. per milliliter in 0.9 per cent for most ophthalmological procedures. NaCl) was injected intramuscularly, the groups CI-744 (Parke-Davis), a new short-acting agent receiving, respectively, 3.2, 4.0, and 5.0 mg. per for chemical restraint and surgical anesthesia in kilogram. The monkeys could be safely handled animals, is a 1:1 mixture by weight of tiletamine- without gloves within a few minutes (time not HCl (CI-634, an arylcycloalkylamine analogue of precisely noted) after receiving any of these phencyclidine and ketamine) and zolazepam-HCl doses. -

Appendix-2Final.Pdf 663.7 KB
North West ‘Through the Gate Substance Misuse Services’ Drug Testing Project Appendix 2 – Analytical methodologies Overview Urine samples were analysed using three methodologies. The first methodology (General Screen) was designed to cover a wide range of analytes (drugs) and was used for all analytes other than the synthetic cannabinoid receptor agonists (SCRAs). The analyte coverage included a broad range of commonly prescribed drugs including over the counter medications, commonly misused drugs and metabolites of many of the compounds too. This approach provided a very powerful drug screening tool to investigate drug use/misuse before and whilst in prison. The second methodology (SCRA Screen) was specifically designed for SCRAs and targets only those compounds. This was a very sensitive methodology with a method capability of sub 100pg/ml for over 600 SCRAs and their metabolites. Both methodologies utilised full scan high resolution accurate mass LCMS technologies that allowed a non-targeted approach to data acquisition and the ability to retrospectively review data. The non-targeted approach to data acquisition effectively means that the analyte coverage of the data acquisition was unlimited. The only limiting factors were related to the chemical nature of the analyte being looked for. The analyte must extract in the sample preparation process; it must chromatograph and it must ionise under the conditions used by the mass spectrometer interface. The final limiting factor was presence in the data processing database. The subsequent study of negative MDT samples across the North West and London and the South East used a GCMS methodology for anabolic steroids in addition to the General and SCRA screens. -

Pharmacological Review of Chemicals Used for the Capture of Animals
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Proceedings of the 7th Vertebrate Pest Vertebrate Pest Conference Proceedings Conference (1976) collection March 1976 PHARMACOLOGICAL REVIEW OF CHEMICALS USED FOR THE CAPTURE OF ANIMALS Peter J. Savarie U.S. Fish and Wildlife Service Follow this and additional works at: https://digitalcommons.unl.edu/vpc7 Part of the Environmental Health and Protection Commons Savarie, Peter J., "PHARMACOLOGICAL REVIEW OF CHEMICALS USED FOR THE CAPTURE OF ANIMALS" (1976). Proceedings of the 7th Vertebrate Pest Conference (1976). 41. https://digitalcommons.unl.edu/vpc7/41 This Article is brought to you for free and open access by the Vertebrate Pest Conference Proceedings collection at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Proceedings of the 7th Vertebrate Pest Conference (1976) by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. PHARMACOLOGICAL REVIEW OF CHEMICALS USED FOR THE CAPTURE OF ANIMALS* PETEIR J. SAVARIE, U.S. Fish and Wildlife Service, Building 16, Federal Center, Denver, Colorado 80225 ABSTRACT: A review of the literature reveals that over 60 chemicals have been used for the capture of wi l d animals, but only 30 of the most widely used chemicals are discussed in the present paper. For practical considerations these chemicals can be c l a ssified as being either (l) neuromuscular blocking agents, or (2) central nervous system (CNS) depressants. Some common neuromuscular blocking agents are d-tubocurarine, gallamine, succiny1choline, and nicotine. M99 and its derivatives, phencyclidine, and xylazine are some of the more commonly used CNS depressants. Neuromuscular blocking agents have a relatively rapid onset and short duration of action but they do not possess sedative, analgesic, or anesthetic properties. -

Tiletamine-Zolazepam Anesthesia in North American River Otters (Lutra Canadensis) and Its Partial Antagonism with Flumazenil
]OUf7/U[ (~rZOO and Wild/~re M(>dicine 28(4): 418-423,1997 Copyright 1997 by American Association of Zoo Veterinarians TILETAMINE-ZOLAZEPAM ANESTHESIA IN NORTH AMERICAN RIVER OTTERS (LUTRA CANADENSIS) AND ITS PARTIAL ANTAGONISM WITH FLUMAZENIL Lucy H. Spelman, D.V.M., Perry W. Sumner, M.S., William B. Karesh, D.V.M., and Michael K. Stoskopf, D.V.M., Ph.D. Abstract: North American river otters (Lutra canadensis) were anesthetized with tiletamine-zolazepam or tiletamine zolazepam-flumazenil combinations in cooperation with the North Carolina Wildlife Resources Commission Otter Restoration Project for evaluation of physiologic changes during anesthesia. Sixteen otters received tiletamine-zolaze pam (4 mg/kg combined, i.m.) in 1994. Induction and recovery times were recorded and physiologic data (heart rate and rhythm, respiratory rate, rectal temperature, relative oxyhemoglobin saturation, and mean arterial blood pressure) were collected at 5-min intervals. Respiratory depression developed initially in all otters, and median relative oxyhe moglobin saturation remained below 90% for the first 15 min of anesthesia. Anesthetic induction with tiletamine zolazepam was rapid and smooth, but recovery was prolonged (median = 89 min) and characterized by persistent head motion. In 1995, flumazenil was evaluated as a partial antagonist for tiletamine-zolazepam anesthesia in otters. Sixteen otters were anesthetized with tiletamine-zolazepam (4 mg/kg combined, i.m.) and given flumazenil (I mg per 25 mg of zolazepam) after 20 min. Flumazenil markedly shortened recovery time in all otters anesthetized with tiletamine zolazepam (median = 65 min) with no adverse effects. Key words: River otter, Lutra canadensis, anesthesia, tiletamine-zolazepam, flumazenil. INTRODUCTION ratory depression produced by diazepam and mid 7 9 azolam.4. -

Information Resources on the Care and Welfare of Horses
NATIONAL AGRICULTURAL LIBRARY ARCHIVED FILE Archived files are provided for reference purposes only. This file was current when produced, but is no longer maintained and may now be outdated. Content may not appear in full or in its original format. All links external to the document have been deactivated. For additional information, see http://pubs.nal.usda.gov. United States Information Resources on the Care and Department of Agriculture Welfare of Horses AWIC Resource Series No. 36 Agricultural Research November 2006 Service Updates Housing, Husbandry, and Welfare of Horses, 1994 National Agricultural Library Animal Welfare Information Center Compiled and edited by: Cristin Swords Animal Welfare Information Center National Agricultural Library U.S. Department of Agriculture Published by: U. S. Department of Agriculture Agricultural Research Service National Agricultural Library Animal Welfare Information Center Beltsville, Maryland 20705 Web site: http://awic.nal.usda.gov Published in cooperation with the Virginia-Maryland Regional College of Veterinary Medicine Web Policies and Important Links Contents Forward About this Document Request Library Materials Horse Welfare by D. Mills, University of Lincoln Equine Welfare Issues in the United States: An Introduction by C.L. Stull, University of California, Davis Bibliography Anesthesia and Analgesia Behavior Environmental Enrichment Housing Law and Legislation Nutrition and Feeding Feeding Methods Feeding Restrictions Age Specific Nutrition Concentrates Roughages Vitamins and Supplements Pasture PMU Ranching Safety Training Transportation Web Resources Forward This information resource came to fruition through the diligence of a student employee at the Animal Welfare Information Center. The document contains a comprehensive bibliography and extensive selection of web site resources. Two papers introducing horse care and welfare issues are also included.