2013 Lowitja O'donoghue Oration Ms Olga Havnen, CEO, Danila Dilba
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

In Mt Druitt
Losing Ground? Issues of Autonomy in an Urban Indigenous Organisation Elise Katharine Adams School of Archaeology and Anthropology, The Australian National University Submitted March 2014 A thesis submitted for the degree of Doctor of Philosophy of The Australian National University I certify that this thesis is a product of my own original work and has not been published elsewhere. All data collection, analysis and writing, except where cited in the text, has been undertaken and completed solely by the author. _____________________________ Elise Adams School of Archaeology and Anthropology The Australian National University, Canberra Abstract This thesis offers an ethnographic study of one urban Aboriginal organisation, Winanga-Li Aboriginal Corporation; a successful human services agency struggling against the socioeconomic disadvantage faced by Aboriginal Australians. The thesis argues that the difficulties faced by Winanga-Li stem not from Indigenous incapacity, but rather from government policies that maintain Indigenous oppression. Three interwoven theoretical strands serve to explicate this thesis: those of post- colonialism, identity politics, and neoliberalism within contemporary government bureaucracies. Essential to this theoretical framework is the exploration of power relationships between Indigenous Australians and the State. These power relationships not only bear upon Indigenous interactions with other Australians and each other, but also upon both Aboriginal and non-Aboriginal peoples’ constructions of Indigenous culture, -
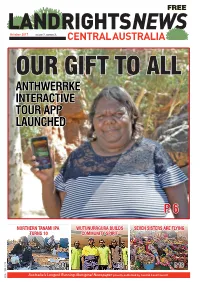
P. 6 Anthwerrke Interactive Tour App Launched
FREE October 2017 VOLUME 7. NUMBER 3. OUR GIFT TO ALL ANTHWERRKE INTERACTIVE TOUR APP LAUNCHED P. 6 NORTHERN TANAMI IPA WUTUNURRGURA BUILDS SEVEN SISTERS ARE FLYING TURNS 10 COMMUNITY SPIRIT P. 14 PG. # P. 4 PG. # P. 19 ISSN 1839-5279ISSN NEWS EDITORIAL Land Rights News Central Bush tenants need NT rental policy overhaul Australia is published by the THE TERRITORY’S Aboriginal Central Land Council three peak organisations have called times a year. on the NT Government to The Central Land Council review its rental policy in remote communities and 27 Stuart Hwy come clean on tenants’ alleged Alice Springs debts following a test case NT 0870 in the Supreme Court that tel: 89516211 highlighted rental payment chaos. www.clc.org.au At stake is whether remote email [email protected] community tenants will have Contributions are welcome to pay millions of dollars worth of rental debts. APO NT’s comments The housing department is pursuing Santa Teresa tenants over rental debts they didn’t know they owed. respond to the test case and SUBSCRIPTIONS reports since at least 2012 that several changes of landlord. half the Santa Teresa tenants that their houses be repaired, the NT Housing Department The department countersued owe an estimated $1 million in that they tell them about all Land Rights News Central has trouble working out who 70 of Santa Teresa’s 100 unpaid rent. this debt. It’s disgraceful.” Australia subscriptions are has paid what rent and when, households who took it to the When Justice Southwood With over 6000 houses $22 per year. -

Bush Schools Should Focus Still Low (10 Per Cent)
= FREE May 2014 VOLUME 4. NUMBER 1. SHARING THE KNOWLEDGE PG. 25 BUSH BUDGET CRICKET SCHOOLS TROUBLES CULTURE PG. 4-5 PG. 2 PG. 32 ISSN 1839-5279ISSN NEWS EDITORIAL Oil and work in full flow Land Rights News Central TRADITIONAL owners Australia is published by the from Kintore and other Central Land Council three western communities are times a year. getting ready for a new set of jobs in the oil industry. The Central Land Council Exploration began in 2007 27 Stuart Hwy after the signing of an exploration agreement. Alice Springs Oil was discovered NT 0870 by Central Petroleum in the Surprise well, 83 km tel: 89516211 southeast of Kintore, in www.clc.org.au early 2012. The oil flowed email [email protected] under its own pressure from about 2,600 m deep Contributions are welcome up to the land surface at about 400 barrels a day. In late 2013 the CLC concluded negotiations with the company for a production agreement SUBSCRIPTIONS under the Land Rights Land Rights News Central Act. In February 2014 the NT Government granted Australia subscriptions are the production licence. It $20 per annum. was one of the quickest ABOVE: Kintore men meet with the oil company and employment contractor at Surprise Oil Well to discuss LRNCA is distributed free negotiations for a mining employment possibilities. to Aboriginal organisations or production agreement in CLC’s history. Port Augusta for refining into diesel and 2011 and are hoping for ongoing work and communities in Central Now, about 2 or 3 oil tankers leave the other products. -

Message from Our Chairperson
July 2018 March 2015 Become a member Message from our Danila Dilba is a community Chairperson controlled organisation, In the absence of our CEO Olga Havnen this which means we have a month for a well deserved break it is great to Board elected by members of see how our Darwin General Manager the Biluru (Aboriginal and Malcolm Darling has stepped up as acting Torres Strait Islander) CEO and other managers have stepped up community in the Yilli Rreung to take senior leadership roles. This has (greater Darwin) region. provided a great opportunity for career Danila Dilba Chairperson development for our clinic management team Carol Stanislaus. Our Board and members are who are 100% Aboriginal and Torres Strait Islander. This essential to guiding the services experience will set them up well for the future and demonstrates we provide to the community. the depth of experience we have within Danila Dilba. As well as our clinics, we continue to work in the community at community Please visit our website or events and advocating for our people in regards to the findings phone us if you are an from the NT Royal Commission into the protection and detention of children in the NT. In this area, we have held extensive Aboriginal or Torres Strait consultations across the NT and with the support of AMSANT Islander person living in the Yilli and Territory Families, are looking into the development of Rreung region and would like a Aboriginal out of home care services and providers. Eventually, membership form. we are hoping this will put care of our children back in the hands of Aboriginal and Torres Strait Islander organisations that www.ddhs.org.au provide culturally appropriate services with a holistic approach. -

Data Linkage Study of Northern Territory Children: a to Inform Policy and Practice in Health, Family Services and Education
Lessons learnt – data linkage study of Northern Territory children: a to inform policy and practice in health, family services and education Presented by A/Professor Stefanie Schurer School of Economics | Charles Perkins Centre www.stefanie-schurer.com The University of Sydney Page 1 Overview Question How do we know whether a specific policy was effective in helping vulnerable (here: Indigenous) children to thrive? RCTs? Yes-gold standard (JPAL MIT, UChicago Urban Lab) What if RCTs are not available? Solution 1. Policy Evaluation Methods: Quasi-experimental methods, natural experiments. 2. Data: Linked administrative data financed through an NHMRC Partnership Project, NHMRC Targeted Call, NHMRC CRE 3. Examples 3.1 Standard early-life health care (special care nursery admission) 3.2 Income management The University of Sydney Page 2 Policies may have positive and negative spill-over effects + - Policy Lever The University of Sydney Page 3 WHAT ARE NATURAL EXPERIMENTS? The University of Sydney Page 4 Major external shocks Epidemics, famines, economic crises or individual-specific shocks to study causes of disease Institutional decision rules Admission to SCN or An elite school using a score threshold Gradual roll-out of a program Income management SNAP (US Food Stamps) The University of Sydney Page 5 Provocative Question 1 Are neonatal intensive care units or special care nurseries cost- effective investments into Indigenous children’s health and wellbeing? The University of Sydney Page 6 NICU/SCN Admission (AIHW, 2011) The University of Sydney Page 7 SPN 3,000$-NICU 4,000$ up to 200,000$ until the baby leaves hospital The University of Sydney Page 8 Provocative Question 2 Did income management under the NTER (2007-2008) lead to better health, developmental, and education outcomes for Indigenous children? The University of Sydney Page 9 Income management locations today Source: Department of Social Services, www.dss.gov.au. -

1 Aboriginal Peak Organisations (NT) Submission to the Select Committee
Aboriginal Peak Organisations (NT) submission to the Select Committee into the Abbott Government’s Budget Cuts 19 September 2014 1 APO NT Submission on the proposed Abbott Budget Cuts | 16 September 2014 SUBMISSION FROM APO NT TO THE SELECT COMMITTEE SECRETARIAT INTO THE ABBOTT GOVERNMENT’S BUDGET CUTS 1. INTRODUCTION Aboriginal Peak Organisations Northern Territory (APO NT) welcomes the opportunity to make a submission to the Select Committee inquiry into the effect of the Abbott Government Budget Cuts. This submission reiterates many of the views and recommendations provided in APO NT’s submission to the Community Affairs Legislation Committee inquiry into the Social Services Bills as well as the concerns raised by the National Aboriginal and Torres Strait Islander Legal Services and Australian Council of Social Services submissions to the Select Committee on the Abbott Government Budget Cuts. APO NT contends that the Government's proposed changes to the Aboriginal legal services, access to health services and to the welfare system will have a significant, detrimental impact on Aboriginal people in the Northern Territory. Such budget cuts run counter to Australia’s efforts to Close the Gap on Indigenous disadvantage, particularly in areas with weak labour markets and a lack of job opportunities. This is of serious concern especially considering there appears to be an enormous impact on people that are not in the labour force, this includes the elderly, students and those engaged in home duties. 2. ABOUT APO NT Formed in October 2010, APO NT is an alliance between the Northern Land Council (NLC), Central Land Council (CLC), Aboriginal Medical Services Alliance Northern Territory (AMSANT), North Australian Aboriginal Justice Agency (NAAJA) and Central Australian Aboriginal Legal Aid Service (CAALAS). -

Public Hearing Darwin 12 August 2014
LEGISLATIVE ASSEMBLY OF THE NORTHERN TERRITORY 12th Assembly Select Committee on Action to Prevent Foetal Alcohol Spectrum Disorder Public Hearing Transcript 9.00 am, Tuesday, 12 August 2014 Litchfield Room, Parliament House Members: The Hon. Kezia Purick, MLA, Chair, Member for Goyder Mr Gary Higgins, MLA, Member for Daly Mr Gerry McCarthy, MLA, Member for Barkly Ms Nicole Manison, MLA, Member for Wanguri Mr Gerry Wood, MLA, Member for Nelson Witnesses: Chamber of Commerce NT Mr Greg Bicknell, Chief Executive Officer via Videoconference Australian Institute of Health and Welfare Dr Al-Yaman, Head, Indigenous and Children’s Group Mr Geoff Neideck, Head, Housing, Homelessness and Drugs Group CatholicCare NT Ms Kim Burns, Senior Manager AOD Ms Milly Hardy, Safe House Coordinator Danila Dilba Health Service Ms Olga Havnen, Chief Executive Officer Ms Joy McLaughlin, Specialist Consultant Dr James Stephen, Senior Medical Officer NT Council of Social Services (NTCOSS) Ms Wendy Morton, executive Director Ms Samantha Bowden, Board Member Ms Nicole Coalter, Board Member Top End Women’s Legal Service Inc Ms Aditi Srinivas, Solicitor First People’s Disability Network Mr Damien Griffis, Chief Executive Officer Select Committee on Action to Prevent Foetal Alcohol Spectrum Disorder, 12 August 2014 Mr Scott Avery, National Policy Officer National Indigenous Drug and Alcohol Committee (NIDAC) Mr Scott Wilson, Deputy Chair via Teleconference Australian Hotels Association (NT Branch) Mr Justin Coleman, President Ms Amy Corcoran, Chief Executive Officer Mr Michael Burns, Board Member 2 Select Committee on Action to Prevent Foetal Alcohol Spectrum Disorder, 12 August 2014 CHAMBER OF COMMERCE NT Madam CHAIR: Welcome, on behalf of the committee, to the public hearing into action to prevent Foetal Alcohol Spectrum Disorder. -
AMSANT-Annual-Report
AMSANT 2019–2020 Annual Report 2019–2020 AMSANT Marthakal Homeland Resource Centre (Galiwin’ku) FORWAARD Balunu Foundation Mala’la Health Danila Dilba Health Service DarwinD Nhulunbuyuy Miwatj Health Council for Aboriginal Alcohol Program SiServices (CAAPS) Jabiru ReRedd LiLillyy Health Board Laynhapuy Homelands Association Katherine West Health Board Katherine Sunrise Health Service Peppimenarti Health Association Wurli Wurlinjang Health Service Tennant Creek Anyinginyi Health Service Ampilatwatja Health Service Urapuntja Health Service Pintupi Homelands Health Service Purple House Alice Springgss Western Aranda Central Australian Aboriginal Health Service (Ntaria) AAlcohol Program Unit (CAAAPU) AAmoonguna Health Service NPY Women’s Council Mpwelerre Health Service ((Santa Teresa) Utju Health Service (Areyonga) Central Australian Aboriginal Congress Mutitjulu Health Service 2 CONTENTS About AMSANT 5 Members 6 Governance 8 Board 10 Strategic Plan 2019–2023 14 Chairperson’s report 18 CEO’s report 20 COVID-19 response 22 Expanding Community Control 26 Member support 30 AMSANT: 25 years of health leadership! 48 Policy and Advocacy 52 Public Health 56 Research 62 Aboriginal Peak Organisations Northern Territory (APO NT) 64 Glossary 68 AMSANT Incorporated Financial Report for the year ended 30 June 2020 70 AMSANT respects Aboriginal and Torres Strait Islander cultures and strives to avoid publishing the names or images of deceased people. AMSANT acknowledges the traditional owners and custodians across the lands on which we live and work, and we pay our respects to elders past and present. Photography © David Hancock. 3 NT ACCHSs service 68% of all clients in Aboriginal Primary Health Care NT AHKPI Report NT ACCHSs service 52,921 clients and 733,314 client interactions NT AHKPI Report 4 ABOUT AMSANT We aim to grow a strong Aboriginal community controlled primary health care sector. -
Index of Indigenous Health Articles in the Sydney Morning Herald
The Media and Indigenous Policy Project Index of Indigenous Health Articles in the Sydney Morning Herald 1988-89, 1994-95, 2002-03 & 2006-07 Compiled by Monica Andrew University of Canberra The articles in this index were collected from the Factiva database. Further information on the methodology for collecting newspaper articles for this project is available at http://www.canberra.edu.au/faculties/arts-design/research/research- centres/news-and-media-research-centre/events/the-media-and-indigenous-policy/the- media-and-indigenous-policy-database © Monica Andrew, 2013 Andrew, Monica (2013), Index of Indigenous Health Articles in the Sydney Morning Herald, 1988-89, 1994-95, 2002-03 & 2006-07, Media and Indigenous Policy Project, University of Canberra. http://www.canberra.edu.au/faculties/arts-design/research/research-centres/news-and-media- research-centre/events/the-media-and-indigenous-policy/the-media-and-indigenous-policy- database Further information about the Media and Indigenous Policy project is available at http://www.canberra.edu.au/faculties/arts-design/research/research-centres/news-and-media- research-centre/events/the-media-and-indigenous-policy The Media and Indigenous Policy project was supported under the Australian Research Council’s Discovery Projects funding scheme (DP0987457), with additional funding supplied by the Faculty of Arts and Design, University of Canberra. Sydney Morning Herald 1988 Title: The year of black protest Publication: Sydney Morning Herald Publication date: Monday, 4 January 1988 Writer(s): News genre: Editorial Page number: 8 Word length: 554 News source: Opinion First spokesperson: Unknown Second spokesperson: Synopsis: Discussion of Aboriginal protests during the Bicentenary year. -

Our Story a Year in Review 2009–2010
Our story a year in review 2009–2010 Our Vision: To improve the lives of vulnerable people in Australia and internationally by mobilising the power of humanity. To be a leading humanitarian Our Mission: organisation in Australia, improving the lives of vulnerable people through programs delivered and promotion of humanitarian laws and values. Contents Priority areas P4 Message from the CEO and Chair P5 Strategy 2015: Working as One P6 August 2009 P7 September 2009 P8 October 2009 P12 November 2009 P14 December 2009 P16 January 2010 P17 February 2010 P22 March 2010 P28 May 2010 P36 June 2010 P38 First Aid P48 Red Cross people snapshot P49 Business partnerships P50 Major government supporters P52 Financial snapshot P53 Fundamental Principles P63 A year in review 2009–2010 Priority areas Strengthening disaster and 1. emergency services. Increasing international aid and 2. development. Championing international 3. humanitarian law. 4. Addressing the impact of migration. Working with Aboriginal and Torres 5. Strait Islander peoples. Overcoming social exclusion by providing 6. bridges back into the community. Tackling entrenched locational 7. disadvantage. 4 A year in review 2009–2010 Message from the Chair and CEO Our story Only six months after Australia’s worst peace time disaster, the Victorian bushfi res, we were again reminded that nature can be unpredictably cruel. A cholera outbreak in Papua New Guinea AusAID continues to support our work in threatened to take thousands of lives, and we Asia Pacifi c particularly. We would again worked alongside Papua New Guinea Red like to thank the Australian Government Cross to fi ght this very preventable disease. -

North-Australian-Aboriginal-Justice
Submissions on Pre- and Post-Detention Royal Commission into the Protection and Detention of Children in the Northern Territory August 2017 NAAJA Submissions on Pre- and Post-Detention About NAAJA The North Australian Aboriginal Justice Agency (NAAJA) provides high quality, culturally appropriate legal aid services for Aboriginal people in the northern region of the Northern Territory in the areas of criminal, civil and family law, prison support and through-care services. NAAJA is active in systemic advocacy and law reform in areas impacting on Aboriginal peoples’ legal rights and access to justice. NAAJA travels to remote communities across the Top End to provide legal advice and advocacy. About these submissions These submissions respond to topics 1–10 identified by the Royal Commission in its call for submissions on pre- and post-detention. We have addressed topic 11 on legislative reform in each of the substantive topic areas. Our submissions are forward looking and aim to assist the Commission to frame practical recommendations that will improve outcomes for Aboriginal children and young people. We have drawn on NAAJA’s unique organisational knowledge, Aboriginal understandings and expertise as a long-term provider of culturally competent legal, therapeutic and social services to Aboriginal young people in Northern Australia. We have been particularly informed by the experiences of our clients, many of whom have bravely come forward to tell their stories to the Commission and share their ideas for change in the hope that the abuse and indignities they endured are never repeated. NAAJA endorses each of the submissions made on behalf of its clients who gave evidence to the Commission. -

What Conditions Will Enable Indigenous-Led Development to Thrive in Australia? 15 November 2013
What conditions will enable Indigenous-led development to thrive in Australia? 15 November 2013 WHAT CONDITIONS WILL ENABLE INDIGENOUS-LED DEVELOPMENT TO THRIVE IN AUSTRALIA? A consolidation of international and domestic evidence and views of stakeholders as a resource for the design of the Indigenous Development Effectiveness Initiative (IDEI). Compiled by the IDEI team A WORK IN PROGRESS 15 November 2013 An initiative supported by: What conditions will enable Indigenous-led development to thrive in Australia? 15 November 2013 EXECUTIVE SUMMARY Summary of project “Without the genuine and active involvement of Aboriginal and Torres Strait Islander people every step of the way in our efforts to close the gap, we risk making only miniscule progress. A business as usual approach will not close the gap.” Mr Mick Gooda, Indigenous Involvement Vital to Close the Gap, 20121 “Surely it’s time to start looking at the evidence of what’s working for many Indigenous peoples and their communities, to understand why it’s working, and then begin developing policy frameworks to build success: creating broader opportunities for public and private investment, intercultural collaborations and problem-solving towards a more sustainable future”. Dr Seán Kerins, A key role for Indigenous peoples in Australia's sustainable future, 20132 The above quotes neatly sum up the purpose of the Indigenous Development Effectiveness Initiative (IDEI). The Australian Government and World Vision Australia have signed a five-year Memorandum of Understanding 2012-2017 (MOU),