Research Article HYBRID CELLS DIFFERENTIATE to HEPATIC
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Collection of Texts Celebrating Joss Whedon and His Works Krista Silva University of Puget Sound, [email protected]
Student Research and Creative Works Book Collecting Contest Essays University of Puget Sound Year 2015 The Wonderful World of Whedon: A Collection of Texts Celebrating Joss Whedon and His Works Krista Silva University of Puget Sound, [email protected] This paper is posted at Sound Ideas. http://soundideas.pugetsound.edu/book collecting essays/6 Krista Silva The Wonderful World of Whedon: A Collection of Texts Celebrating Joss Whedon and His Works I am an inhabitant of the Whedonverse. When I say this, I don’t just mean that I am a fan of Joss Whedon. I am sincere. I live and breathe his works, the ever-expanding universe— sometimes funny, sometimes scary, and often heartbreaking—that he has created. A multi- talented writer, director and creator, Joss is responsible for television series such as Buffy the Vampire Slayer , Firefly , Angel , and Dollhouse . In 2012 he collaborated with Drew Goddard, writer for Buffy and Angel , to bring us the satirical horror film The Cabin in the Woods . Most recently he has been integrated into the Marvel cinematic universe as the director of The Avengers franchise, as well as earning a creative credit for Agents of S.H.I.E.L.D. My love for Joss Whedon began in 1998. I was only eleven years old, and through an incredible moment of happenstance, and a bit of boredom, I turned the television channel to the WB and encountered my first episode of Buffy the Vampire Slayer . I was instantly smitten with Buffy Summers. She defied the rules and regulations of my conservative southern upbringing. -
![Archons (Commanders) [NOTICE: They Are NOT Anlien Parasites], and Then, in a Mirror Image of the Great Emanations of the Pleroma, Hundreds of Lesser Angels](https://docslib.b-cdn.net/cover/8862/archons-commanders-notice-they-are-not-anlien-parasites-and-then-in-a-mirror-image-of-the-great-emanations-of-the-pleroma-hundreds-of-lesser-angels-438862.webp)
Archons (Commanders) [NOTICE: They Are NOT Anlien Parasites], and Then, in a Mirror Image of the Great Emanations of the Pleroma, Hundreds of Lesser Angels
A R C H O N S HIDDEN RULERS THROUGH THE AGES A R C H O N S HIDDEN RULERS THROUGH THE AGES WATCH THIS IMPORTANT VIDEO UFOs, Aliens, and the Question of Contact MUST-SEE THE OCCULT REASON FOR PSYCHOPATHY Organic Portals: Aliens and Psychopaths KNOWLEDGE THROUGH GNOSIS Boris Mouravieff - GNOSIS IN THE BEGINNING ...1 The Gnostic core belief was a strong dualism: that the world of matter was deadening and inferior to a remote nonphysical home, to which an interior divine spark in most humans aspired to return after death. This led them to an absorption with the Jewish creation myths in Genesis, which they obsessively reinterpreted to formulate allegorical explanations of how humans ended up trapped in the world of matter. The basic Gnostic story, which varied in details from teacher to teacher, was this: In the beginning there was an unknowable, immaterial, and invisible God, sometimes called the Father of All and sometimes by other names. “He” was neither male nor female, and was composed of an implicitly finite amount of a living nonphysical substance. Surrounding this God was a great empty region called the Pleroma (the fullness). Beyond the Pleroma lay empty space. The God acted to fill the Pleroma through a series of emanations, a squeezing off of small portions of his/its nonphysical energetic divine material. In most accounts there are thirty emanations in fifteen complementary pairs, each getting slightly less of the divine material and therefore being slightly weaker. The emanations are called Aeons (eternities) and are mostly named personifications in Greek of abstract ideas. -

Surgical Technique Variety of Orthopaedic Applications
™ The ELEOS Limb Salvage System offers ELEOS Limb options for patients with significant bone loss due to cancer, trauma, or previous Salvage System surgical procedures. The locking taper design has a history of clinical use in a Surgical Technique variety of orthopaedic applications. With an array of options in a multitude of Total Femoral Replacement sizes, the ELEOS system provides the surgeon the ability to meet a variety of patient needs. ELEOS Limb Salvage System ELEOS Limb Salvage System TOTAL FEMORAL REPLACEMENT TABLE OF CONTENTS: PRODUCT DESCRIPTION SURGICAL TECHNIQUE STEPS TIBIAL PREPARATION o TIBIAL REAMING o TIBIAL RESECTION o TIBIAL STEM EXTENSION (OPTIONAL) TIBIAL BASEPLATE PREPARATION o TIBIAL BASEPLATE REAMING o TIBIAL BASEPLATE KEEL PUNCH ACETABULAR PREPARATION FEMORAL COMPONENT SIZING TRIALING o TRIAL ASSEMBLY o TRIAL REDUCTION COMPONENT ASSEMBLY o FEMORAL COMPONENT o TIBIAL COMPONENT CEMENT PREPARATION COMPONENT INSERTION o TIBIAL COMPONENT o FEMORAL COMPONENT o FEMORAL HEAD ASSEMBLY TIBIAL HINGE ASSEMBLY PATELLA RECONSTRUCTION (OPTIONAL) BLOCK AUGMENTS (OPTIONAL) COMPONENT DISASSEMBLY EXPLANTATION INFORMATION IMPLANT PART NUMBERS INSTRUMENT PART NUMBERS Proper surgical procedures and techniques are the responsibility of the medical professional. The following guidelines are furnished for informational purposes only. Each surgeon must evaluate the appropriateness of the procedures based on his or her personal medical training, experience and patient condition. Prior to the use of the system, the surgeon should refer to the product package insert for additional warnings, precautions, indications, contraindications and adverse effects. Instruction for use package inserts are also available at www.onkossurgical/ELEOS/IFU. 2 ELEOS Limb Salvage System PRODUCT DESCRIPTION The ELEOS Total Femoral System consists of ten components: Proximal Femur, Midsection(s), Distal Femur, Tibial Baseplate, Tibial Polyethylene Spacer, Tibial Hinge Component, Axial Pin, Optional Stem Extension and Femoral Head. -

Learning Lineage and the Problem of Authenticity in Ozark Folk Music
University of Mississippi eGrove Electronic Theses and Dissertations Graduate School 1-1-2020 Learning Lineage And The Problem Of Authenticity In Ozark Folk Music Kevin Lyle Tharp Follow this and additional works at: https://egrove.olemiss.edu/etd Recommended Citation Tharp, Kevin Lyle, "Learning Lineage And The Problem Of Authenticity In Ozark Folk Music" (2020). Electronic Theses and Dissertations. 1829. https://egrove.olemiss.edu/etd/1829 This Dissertation is brought to you for free and open access by the Graduate School at eGrove. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of eGrove. For more information, please contact [email protected]. LEARNING LINEAGE AND THE PROBLEM OF AUTHENTICITY IN OZARK FOLK MUSIC A Dissertation presented in partial fulfillment of requirements for the degree of Doctor of Philosophy in the Department of Music The University of Mississippi by KEVIN L. THARP May 2020 Copyright Kevin L. Tharp 2020 ALL RIGHTS RESERVED ABSTRACT Thorough examination of the existing research and the content of ballad and folk song collections reveals a lack of information regarding the methods by which folk musicians learn the music they perform. The centuries-old practice of folk song and ballad performance is well- documented. Many Child ballads and other folk songs have been passed down through the generations. Oral tradition is the principal method of transmission in Ozark folk music. The variants this method produces are considered evidence of authenticity. Although alteration is a distinguishing characteristic of songs passed down in the oral tradition, many ballad variants have persisted in the folk record for great lengths of time without being altered beyond recognition. -

Slayage, Number 16
Roz Kaveney A Sense of the Ending: Schrödinger's Angel This essay will be included in Stacey Abbott's Reading Angel: The TV Spinoff with a Soul, to be published by I. B. Tauris and appears here with the permission of the author, the editor, and the publisher. Go here to order the book from Amazon. (1) Joss Whedon has often stated that each year of Buffy the Vampire Slayer was planned to end in such a way that, were the show not renewed, the finale would act as an apt summation of the series so far. This was obviously truer of some years than others – generally speaking, the odd-numbered years were far more clearly possible endings than the even ones, offering definitive closure of a phase in Buffy’s career rather than a slingshot into another phase. Both Season Five and Season Seven were particularly planned as artistically satisfying conclusions, albeit with very different messages – Season Five arguing that Buffy’s situation can only be relieved by her heroic death, Season Seven allowing her to share, and thus entirely alleviate, slayerhood. Being the Chosen One is a fatal burden; being one of the Chosen Several Thousand is something a young woman might live with. (2) It has never been the case that endings in Angel were so clear-cut and each year culminated in a slingshot ending, an attention-grabber that kept viewers interested by allowing them to speculate on where things were going. Season One ended with the revelation that Angel might, at some stage, expect redemption and rehumanization – the Shanshu of the souled vampire – as the reward for his labours, and with the resurrection of his vampiric sire and lover, Darla, by the law firm of Wolfram & Hart and its demonic masters (‘To Shanshu in LA’, 1022). -
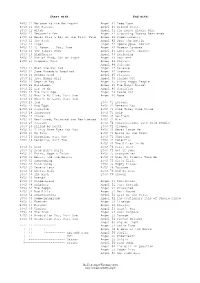
Buffy & Angel Watching Order
Start with: End with: BtVS 11 Welcome to the Hellmouth Angel 41 Deep Down BtVS 11 The Harvest Angel 41 Ground State BtVS 11 Witch Angel 41 The House Always Wins BtVS 11 Teacher's Pet Angel 41 Slouching Toward Bethlehem BtVS 12 Never Kill a Boy on the First Date Angel 42 Supersymmetry BtVS 12 The Pack Angel 42 Spin the Bottle BtVS 12 Angel Angel 42 Apocalypse, Nowish BtVS 12 I, Robot... You, Jane Angel 42 Habeas Corpses BtVS 13 The Puppet Show Angel 43 Long Day's Journey BtVS 13 Nightmares Angel 43 Awakening BtVS 13 Out of Mind, Out of Sight Angel 43 Soulless BtVS 13 Prophecy Girl Angel 44 Calvary Angel 44 Salvage BtVS 21 When She Was Bad Angel 44 Release BtVS 21 Some Assembly Required Angel 44 Orpheus BtVS 21 School Hard Angel 45 Players BtVS 21 Inca Mummy Girl Angel 45 Inside Out BtVS 22 Reptile Boy Angel 45 Shiny Happy People BtVS 22 Halloween Angel 45 The Magic Bullet BtVS 22 Lie to Me Angel 46 Sacrifice BtVS 22 The Dark Age Angel 46 Peace Out BtVS 23 What's My Line, Part One Angel 46 Home BtVS 23 What's My Line, Part Two BtVS 23 Ted BtVS 71 Lessons BtVS 23 Bad Eggs BtVS 71 Beneath You BtVS 24 Surprise BtVS 71 Same Time, Same Place BtVS 24 Innocence BtVS 71 Help BtVS 24 Phases BtVS 72 Selfless BtVS 24 Bewitched, Bothered and Bewildered BtVS 72 Him BtVS 25 Passion BtVS 72 Conversations with Dead People BtVS 25 Killed by Death BtVS 72 Sleeper BtVS 25 I Only Have Eyes for You BtVS 73 Never Leave Me BtVS 25 Go Fish BtVS 73 Bring on the Night BtVS 26 Becoming, Part One BtVS 73 Showtime BtVS 26 Becoming, Part Two BtVS 74 Potential BtVS 74 -
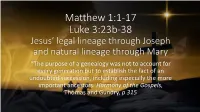
Matthew 1:1-17 Luke 3:23B-38
Matthew 1:1-17 Luke 3:23b-38 Jesus’ legal lineage through Joseph and natural lineage through Mary “The purpose of a genealogy was not to account for every generation but to establish the fact of an undoubted succession, including especially the more important ancestors. Harmony of the Gospels, Thomas and Gundry, p 315 Matthew 1:1-17 Luke 3:23b-38 Jesus’ legal lineage through Joseph and natural lineage through Mary Genealogies used to: Show identity and duty Demonstrate credentials for power and property Structure history Indicate one’s character Matthew 1:1-17 Luke 3:23b-38 Jesus’ legal lineage through Joseph and natural lineage through Mary Comparison and Contrast between Matthew and Luke: Inverted End at different places in the past Different names Converge at David Matthew includes women Matthew 1:1-17 Luke 3:23b-38 Jesus’ legal lineage through Joseph and natural lineage through Mary The differences can be explained as Matthew offers Joseph’s genealogy and Luke offers Mary’s. Both show that Jesus is a descendant of David as promised in scripture Matthew 1:1-17 Luke 3:23b-38 Jesus’ legal lineage through Joseph and natural lineage through Mary Matthew’s purpose is to show Jesus as the fulfillment of the promise of a Messiah through God’s chosen people. Luke’s purpose is to reveal the Savior to all of mankind. John’s birth foretold to Zechariah Luke 1:5-25 • Verse 5 is typical of Luke’s use of details in his writing. • Verses 6 and 7 give a stark contrast to the assessment of Zechariah and Elizabeth by God and what the people of their day would think of them. -

FY14 Fatalities and Catastrophes to Date
FY14 Fatalities and Catastrophes To Date Date of Incident Company, City, State, ZIP Preliminary Description of Incident Fatality or Inspection # Catastrophe 9/30/2014 City of Covina Police Department, Covina, CA Worker killed in vehicle collision. Fatality 91728 9/30/2014 Precision Fabricators Inc., Tulsa, OK 74127 Worker struck and killed by falling load when Fatality crane bolt broke. 9/30/2014 Wise Recycling East 1 Inc., Charlotte, NC 28216 Worker killed when forklift tipped over. Fatality 9/29/2014 All Star Metals, Brownsville, TX 78521 Worker fatally crushed between metal sections of Fatality vessel during dismantling. 9/29/2014 Central States Environmental LLC, Freeport, PA Worker killed in fall from bed of truck. Fatality 15352 9/29/2014 Mayflower RV, Mayflower, AR 72106 Worker killed when loader overturned. Fatality 9/29/2014 Philadelphia Zoo, Philadelphia, PA 19104 Worker fatally crushed when golf cart fell off jack Fatality stands during maintenance. 9/27/2014 Lash Paving Company, Quaker City, OH 43773 Worker fatally crushed by tire compactor. Fatality 9/27/2014 Pittman Construction Company, Conyers, GA Worker struck and killed by dump truck. Fatality 30013 9/26/2014 Evergreen Lawn & Tree Care Inc., Spokane, WA Worker killed on fall from tree. Fatality 99203 9/26/2014 Miranda Trucking, Hereford, TX 79045 Employee struck and killed by truck. Fatality 9/26/2014 Redneck Services, Amarillo, TX 79102 Oil company worker caught and killed by drill Fatality blade. 9/26/2014 Santigo E. Monge, Lincoln University, PA 19352 Worker killed in fall from tree. Fatality 9/25/2014 Arends-Awe Inc., Winchester, IL 62694 Worker fatally crushed by combine. -

MONTEVERDI's OPERA HEROES the Vocal Writing for Orpheus And
MONTEVERDI’S OPERA HEROES The Vocal Writing for Orpheus and Ulysses Gustavo Steiner Neves, M.M. Lecture Recital Dissertation Submitted to the Graduate Faculty of Texas Tech University in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF MUSICAL ARTS Karl Dent Chair of Committee Quinn Patrick Ankrum, D.M.A. John S. Hollins, D.M.A. Mark Sheridan, Ph.D. Dean of the Graduate School May, 2017 © 2017 Gustavo Steiner Neves Texas Tech University, Gustavo Steiner Neves, May 2017 TABLE OF CONTENTS ABSTRACT iii LIST OF MUSICAL EXAMPLES iv LIST OF TABLES iv CHAPTER I: INTRODUCTION 1 Thesis Statement 3 Methodology 3 CHAPTER II: THE SECOND PRACTICE AND MONTEVERDI’S OPERAS 5 Mantua and La Favola d’Orfeo 7 Venice and Il Ritorno d’Ulisse in Patria 13 Connections Between Monteverdi’s Genres 17 CHAPTER III: THE VOICES OF ORPHEUS AND ULYSSES 21 The Singers of the Early Seventeenth Century 21 Pitch Considerations 27 Monteverdi in the Twentieth and Twenty-First Centuries 30 Historical Recordings and Performances 32 Voice Casting Considerations 35 CHAPTER IV: THE VOCAL WRITING FOR ORPHEUS AND ULYSSES 37 The Mistress of the Harmony 39 Tempo 45 Recitatives 47 Arias 50 Ornaments and Agility 51 Range and Tessitura 56 CHAPTER V: CONCLUSIONS 60 BIBLIOGRAPHY 63 ii Texas Tech University, Gustavo Steiner Neves, May 2017 ABSTRACT The operas of Monteverdi and his contemporaries helped shape music history. Of his three surviving operas, two of them have heroes assigned to the tenor voice in the title roles: L’Orfeo and Il Ritorno d’Ulisse in Patria. -
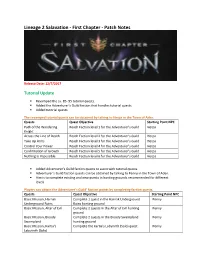
Lineage 2 Salavation - First Chapter - Patch Notes
Lineage 2 Salavation - First Chapter - Patch Notes Release Date: 12/7/2017 Tutorial Update . Revamped the Lv. 85- 95 tutorial quests. Added the Adventurer’s Guild faction that handles tutorial quests. Added tutorial quests. The revamped tutorial quests can be obtained by talking to Herpa in the Town of Aden. Quests Quest Objective Starting Point NPC Path of the Wandering Reach Faction level 1 for the Adventurer’s Guild Herpa Knight Across the Line of Death Reach Faction level 2 for the Adventurer’s Guild Herpa Take Up Arms Reach Faction level 3 for the Adventurer’s Guild Herpa Control Your Power Reach Faction level 4 for the Adventurer’s Guild Herpa Confirmation of Growth Reach Faction level 5 for the Adventurer’s Guild Herpa Nothing is Impossible Reach Faction level 6 for the Adventurer’s Guild Herpa . Added Adventurer’s Guild faction quests to assist with tutorial quests. Adventurer’s Guild faction quests can be obtained by talking to Penny in the Town of Aden. Aim is to complete existing and new quests in hunting grounds recommended for different levels. Players can obtain the Adventurer’s Guild’ faction points by completing faction quests. Quests Quest Objective Starting Point NPC Basic Mission, Harnak Complete 1 quest in the Harnak Underground Penny Underground Ruins Ruins hunting ground Basic Mission, Altar of Evil Complete 2 quests in the Altar of Evil hunting Penny ground Basic Mission, Bloody Complete 2 quests in the Bloody Swampland Penny Swampland hunting ground Basic Mission, Kartia's Complete the Kartia's Labyrinth (Solo) -

Interaction Between Neurons and the Oligodendroglial Lineage in Multiple Sclerosis and Its Preclinical Models
life Review Interaction between Neurons and the Oligodendroglial Lineage in Multiple Sclerosis and Its Preclinical Models Vasiliki Pantazou 1,2 , Thomas Roux 1,3, Vanessa Oliveira Moreira 1, Catherine Lubetzki 1,3,† and Anne Desmazières 1,*,† 1 Paris Brain Institute (ICM), Sorbonne Université, CNRS, Inserm, GH Pitié-Salpêtrière, 47 boulevard de l’Hôpital, 75013 Paris, France; [email protected] (V.P.); [email protected] (T.R.); [email protected] (V.O.M.); [email protected] (C.L.) 2 Service de Neurologie, Centre Hospitalier Universitaire Vaudois, 46 Rue du Bugnon, 1011 Lausanne, Switzerland 3 Assistance Publique-Hôpitaux de Paris, Neurology Department, Pitié Salpêtrière University Hospital, 75013 Paris, France * Correspondence: [email protected] † These authors contributed equally to this work. Abstract: Multiple sclerosis (MS) is a complex central nervous system inflammatory disease leading to demyelination and associated functional deficits. Though endogenous remyelination exists, it is only partial and, with time, patients can enter a progressive phase of the disease, with neurodegeneration as a hallmark. Though major therapeutic advances have been made, with immunotherapies reducing relapse rate during the inflammatory phase of MS, there is presently no therapy available which significantly impacts disease progression. Remyelination has been shown to favor neuroprotection, and it is thus of major importance to better understand remyelination mechanisms in order to promote them and hence preserve neurons. A crucial point is how this process is regulated through Citation: Pantazou, V.; Roux, T.; the neuronal crosstalk with the oligodendroglial lineage. In this review, we present the current Oliveira Moreira, V.; Lubetzki, C.; knowledge on neuron interaction with the oligodendroglial lineage, in physiological context as well Desmazières, A. -

“A Lineage of Dullards” Zen Master Toju Reiso and His Associates
Japanese Journal of Religious Studies 1998 25/1-2 “A Lineage of Dullards” Zen Master Toju Reiso and His Associates Kato Shoshun This study concentrates on the relatively unknown Rinzai Mino line to illustrate the liveliness of Rinzai Zen practice in Meiji Japan. Even as struggles over the precepts and politics were being waged within the Zen denominations, some clerics attempted to carry on with their quest for awakening in relative isolation. Through a study of three monks, Toju Reiso, Tairyu Bun % and Seishu Shusetsu, strategies employed to preserve Rinzai Zen ^ spiritual legacy in the face of the turmoil of Meiji are high lighted. This article illustrates how these monks did their best to continue their eremetic existence and to pick up the pieces left by the widespread destruction of Buddhist temples and monasteries in early Meiji Japan. Among those familiar w ith Japanese Rinzai Zen it is a well-known fact that the lineage of Hakuin Ekaku 白 隱 慧 鶴 (1686-1769)— the lineage to which all contemporary Rinzai Zen masters belong— presently con sists of two branches, the Inzan 隠、山 branch and the Takuju 卓洲 branch. These were founded, respectively, by Inzan Ien 隱山惟琰 (1751-1814) and Takuju Kosen 卓 洲 胡 傳 (1760-1833),two of the fore most disciples of Hakuin,s immediate successor Gasan Jito 峨山慈棹 (1727-1797). Less well known, however, is the subdivision of the Inzan line into two separate currents: that of Torin Somo 呆 林 宗 侯 (P-1837)1 and Settan Shohaku S 潭 紹 璞 (1801-1873),2 and that of Taigen Shigen This essay is a translation of Gudon no keifu: Toju Reiso to sono shuhen 愚鈍の系譜一 洞宗令聡とその周辺,published in Meiji no Zensho明治の禅匠,Zenbunka henshubu禅文化編集部 e d .(1981, Kyoto: Zenbunka Kenkyusho, pp.