The Relationship of Psychological Trauma with Trichotillomania and Skin Picking
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hair's the Question*
Hair Transplant Forum International www.ISHRS.org March/April 2015 Hair’s the Question* Sara Wasserbauer, MD, FISHRS Walnut Creek, California, USA [email protected] *The questions presented by the author are not taken from the ABHRS item pool and accordingly will not be found on the ABHRS Certifying Examination. I got a new toy a few Christmases ago—a magnifier for my iPhone camera. I have to tell you: I LOVE this thing! For diagnositic usefulness during a consult, you cannot beat magnification (Dr. Nicole Rogers even won the poster competition in Alaska with a little device like this)! If you are not already using it for your patients, having a camera like this (or a video microscope) enables instant analysis and feedback for your patient. They will love it and you will, too. Now let’s test your skills for diagnosing some of these commonly seen photomicrographs of the scalp. 1. This patient has been: 4. The following microscopic photo is an example of: A. Shaving his hair recently A. An ingrown hair B. Plucking out his own hair B. Diffuse folliculitis C. Using keratin hair fibers (aka Toppik®, etc.) C. Donor area 6 months post FUE hair surgery D. Getting regular “Brazilian blowouts” D. Follicular plugging 2. This patient shows evidence of: 5. What recently happened to the hairs in this photo? A. Exclamation point hairs indicating trichotillomania A. They were recently backcombed as evidenced by their B. Alopecia areata ruffled cuticle. C. Loss of follicular openings B. They were recently cut as shown by their blunt (i.e., not D. -

(In)Determinable: Race in Brazil and the United States
Michigan Journal of Race and Law Volume 14 2009 Determining the (In)Determinable: Race in Brazil and the United States D. Wendy Greene Cumberland School fo Law at Samford University Follow this and additional works at: https://repository.law.umich.edu/mjrl Part of the Comparative and Foreign Law Commons, Education Law Commons, Law and Race Commons, and the Law and Society Commons Recommended Citation D. W. Greene, Determining the (In)Determinable: Race in Brazil and the United States, 14 MICH. J. RACE & L. 143 (2009). Available at: https://repository.law.umich.edu/mjrl/vol14/iss2/1 This Article is brought to you for free and open access by the Journals at University of Michigan Law School Scholarship Repository. It has been accepted for inclusion in Michigan Journal of Race and Law by an authorized editor of University of Michigan Law School Scholarship Repository. For more information, please contact [email protected]. DETERMINING THE (IN)DETERMINABLE: RACE IN BRAZIL AND THE UNITED STATES D. Wendy Greene* In recent years, the Brazilian states of Rio de Janeiro, So Paulo, and Mato Grasso du Sol have implemented race-conscious affirmative action programs in higher education. These states established admissions quotas in public universities '' for Afro-Brazilians or afrodescendentes. As a result, determining who is "Black has become a complex yet important undertaking in Brazil. Scholars and the general public alike have claimed that the determination of Blackness in Brazil is different than in the United States; determining Blackness in the United States is allegedly a simpler task than in Brazil. In Brazil it is widely acknowledged that most Brazilians are descendants of Aficans in light of the pervasive miscegenation that occurred during and after the Portuguese and Brazilian enslavement of * Assistant Professor of Law, Cumberland School of Law at Samford University. -

A Case Report
J Psychiatrists’ Association of Nepal Vol .4, No.1, 2015 CASE REPORT ARTICLE Childhood Trichotilomania with Atypical Treatment Response: A Case Report Das M1, Kaur A2 1. Assistant Professor, Department of Psychiatry, Government Medical College, Haldwani, Nainital (Uttarakhand) 2. Assistant Professor, Department of Community Medicine, Government Medical College, Haldwani, Nainital (Uttarakhand). E-mail *Corresponding author: [email protected] Abstract Trichotillomania once was considered as a rare disorder but now it is recognized as a psychiatric illness that is not as rare as previously thought. Standard treatment guideline of this disorder, especially for children is not available till the present date. In this report, a case of childhood trichotillomania, its various diagnostic possibilities and successful treatment with Risperidone in a child has been described. Keywords: Trichotillomania, Childhood Onset, Risperidone INTRODUCTION in infants though it is more often seen in the first French dermatologist, François Henri two decades of life, especially in female Hallopeau was the first to describe a case of self- adolescents. inflicted depilation of scalp and he coined the ICD 10 (International Classification of term Trichotillomania in 1989. This word is Diseases 10th revision) 5 has classified derived from Greek words: tricho- (hair), tillo trichotillomania in habit and impulse disorder (pull), and mania (madness). The term whereas DSM-V (Diagnostic and Statistical trichotillomania is misleading because the suffix Manual of Mental Disorders, Fifth Edition) 4 puts "mania" implies the presence of a serious it under obsessive compulsive and related psychiatric disorder. Even after 100 years of disorders. Meyer and Haag6 reported recognising the disease, etiology, natural history trichotillomania's association with stressful and treatment is not fully clear. -

Trichotillomania: an Impulsion Beyond Hair Pulling (A Case Report)
Iqbal MM, et al., J Clin Stud Med Case Rep 2019, 6: 70 DOI: 10.24966/CSMC-8801/100070 HSOA Journal of Clinical Studies and Medical Case Reports Case Report Trichotillomania: An Impulsion Introduction Trichotillomania evolves as an impulse control disorder in the lit- beyond Hair Pulling erature where hair puling ultimately leads to achievement of mental satisfaction and pleasure. Although rare, it has been reported in the (A Case Report) literature previously where adolescents and children between ages 9 -13 years have been frequently targeted by this psycho dermatologic morbidity [1]. Frequent misdiagnosis of trichotillomania with alope- Muhammad Mashood Iqbal*, Muhammad Ishaq Ghauri, Mohammad Shariq Mukarram, Mohammad Faisal Iftikhar and cia areata appears to be common according to studies and hence a Uzzam Ahmed Khawaja challenging task lies to clinically diagnose the former accurately [1- 3]. Trichotillomania repeatedly appears to be linked with depression, Department of Medicine, Jinnah Medical College Hospital, Karachi, Sindh, obsessive compulsive disorder, low self-esteem, poor social function- Pakistan ing and self-image [1,4]. Patients who clinically present with such psychiatric abnormalities should be evaluated for mental and behav- ioral disorders where they tend to carry out anomalous tasks in order Abstract to relieve anxiety. Introduction: Trichotillomania is a psycho dermatologic disorder Clinical interventions to precisely evaluate and further manage that has been identified as a common morbidity in children and ado- trichotillomanics require large scale studies with positive outcomes. lescents having a positive correlation with depression and Obsessive Most successful behavioral modifications and therapies such as habit Compulsive Disorder (OCD). Very few cases have been reported in reversal tend to outweigh the pharmacological approach where the the 20-30 age groups, therefore, we intend on reporting this case. -

Trichotillomania in Childhood: Case Series and Review
Trichotillomania in Childhood: Case Series and Review Yong-Kwang Tay, MD*; Moise L. Levy, MD‡§; and Denise W. Metry, MD‡§ ABSTRACT. Trichotillomania is a relatively common seen over a 2-year period and reviews the literature cause of childhood alopecia. We report our observations on TTM in children. of 10 children with trichotillomania seen over a 2-year period at Texas Children’s Hospital. Patient ages ranged PATIENTS AND METHODS from 9 to 14 years (mean: 11.3 years) with an equal gender This was a retrospective chart review of children diagnosed ratio. The duration of hair-pulling ranged from 1 month with TTM between April 1999 and March 2001 in the dermatology to 10 years (median: 4.6 months). The scalp alone was service at Texas Children’s Hospital. Demographic data and the affected in 8 cases, the scalp and eyelashes in 1 case, and following specifics were collected: duration of hair-pulling, site(s) the eyelashes alone in 1 case. The frontal scalp and vertex of hair loss, potential triggering factors and associated psychopa- were the most common sites affected. Associated find- thology, and treatment rendered. ings included nail-biting in 2 cases, “picking” of the skin in 1 case, and headaches in another case. Noted precipi- RESULTS tating factors in 3 patients included “stress” at home and A total of 10 children, ranging from 9 to 14 years school. Associated psychopathology included major de- old (mean: 11.3 years) with an equal gender ratio, pression in 1 case, attention-deficit/hyperactivity disor- der in 1 case, and an “anxious and nervous personality” were diagnosed with TTM over a 2-year period (Ta- in 1 case. -

Hair Removal & Skin Rejuvenation Machine
Hair Removal & Skin Rejuvenation Machine IPL Hair Removal IPL laser hair removal is a very popular method of hair removal. An IPL laser uses “intense pulsed light” to gently and safely removes hair on the face, legs, back, and bikini/pubic areas. The pulses of light focus their heat on the hair follicles, destroying them without burning or damaging the skin. IPL laser hair removal is quick and veritably painless. Side effects are few, but may include redness or swelling of the treated area; this should disappear rapidly. Good candidates for IPL laser hair removal will have lighter skin and darker hair, since IPL targets pigment in the hair follicles. Many people have experienced permanent hair removal with this method; if hair does grow back, it is often sparse and finer in texture. Laser Hair removal. Laser hair removal is a gentle and effective way to permanently reduce unwanted hair from virtually any area of the body. Locate a laser hair removal clinic in your area and acquire information on the latest laser hair removal options for men and women by reading the sections below. Laser Hair Removal Procedure Laser hair removal is most effective when hair is in the growth stage. Because hair grows in cycles, laser hair removal patients typically require a series of four to six sessions spaced approximately one month apart for maximum results. www.globalclinic.co During Laser Hair Removal Treatment Typically, the areas to be treated are shaved a few days prior to the laser hair removal treatment. On the day of the procedure, an anesthetic cream may be applied, although this step is not necessary. -

Trichotillomania: an Important Psychocutaneous Disorder
PEDIATRIC DERMATOLOGY Series Editor: Camila K. Janniger, MD Trichotillomania: An Important Psychocutaneous Disorder Alexander M. Witkowski; Robert A. Schwartz, MD, MPH; Camila K. Janniger, MD Trichotillomania (TTM) is a type of alopecia due Epidemiology to a psychocutaneous disorder, a self-induced An exact statistical representation of the number of illness classified as an impulse control disorder individuals with TTM in the general population is but with features of both obsessive-compulsive not available.8,9 A number of these patients avoid disorder (OCD) and addictive disorders. Although visiting their physicians and going into public places most common in children, this repetitive pulling where their disorder would be revealed.9-11 In addi- out of one’s own hair can occur at any age. The tion, adults may conceal their plucking habit with target usually is hair of the scalp, eyebrows, eye- wigs, hats, and makeup. The prevalence has been lashes, and pubic area using fingers, brushes, noted to be 0.6% to 3.4% of the total population, combs, and tweezers. Therapy for TTM can with a female to male ratio of 2 to 1.12-14 The inci- be challenging. CUTISdence of TTM appears to be higher in children than Cutis. 2010;86:12-16. in adolescents and adults.15 A small percentage of patients have first-degree family members with the same disorder as well as a history of OCD, depres- richotillomania (TTM) is an unusual type sion, and alcohol and drug abuse.16-20 of alopecia classified as an impulse control T disorder but with features of both obsessive- -

The Use of Habit Reversal to Treat Trichotillomania Following
The Use of Habit Reversal to Treat Trichotillomania Following the Surgical Removal of a Trichobezoar Jody Lieske, MA and Nancy Foster, PhD Munroe-Meyer Institute at the University of Nebraska Medical Center Results (continued) INTRODUCTION Procedure (continued) • Trichotillomania is rare condition that affects 1-4% of the population. In some • Self Awareness: Subject was trained to 1) look in the mirror while String and Clothing Pulling/Swallowing pretending to engage in hair/string pulling and nail biting while focusing on instances, trichophagia, or mouthing of the hair, can lead to the formation of 4 Self- how her body moved and the muscles that were used while the habit was Baseline Self-Awareness/ + trichobezoars (hairballs). Awareness/ + Competing 3.5 Competing Response + being performed; 2) identify times that she started the habit by saying “that Response + Parent/Teacher Parent/Teacher Support + Support Relaxation • Five to 18% of patients with trichotillomania also show trichophagia and was one;” and 3) record each occurrence on a 3x5 index card. 3 approximately 37.5% are at risk for forming a trichobezoar. 2.5 • Practice the Competing Response Daily: Competing responses to hair/string 2 • Trichobezoars account for 55% of all bezoars, 90% which occur in adolescent pulling and swallowing and nail biting/swallowing were generated and Per Week females. include: sitting on hands, holding a stress ball, chewing gum, and sucking 1.5 on hard candy. Frequency 1 • Behavioral interventions have been shown to be effective with treating 0.5 patients with this trichotillomania. However, additional research is needed on • The subject was encouraged to use the competing responses 1) in front of a treatments for trichotillomania when trichophagia is present. -

Puberty Changes in Boys
PUBERTY CHANGES IN BOYS The changes of puberty in boys include growth of testes, growth of the penis, growth of pubic hair, voice change, and height spurt. An individual boy may begin his changes at a time different from his peers. TESTES DEVELOPMENT Growth of testes is usually the first change for boys. The scrotum lengthens and becomes a darker color. These changes begin between 9 ½ and 13 ½ years of age. PENIS DEVELOPMENT Growth of the penis occurs between ages 10 and 14. PUBIC HAIR Pubic hair and underarm hair appear between the ages of 10 and 14. At first the hair is fine and thin but becomes curly and coarse over time. GROWTH SPURT Increased height and change in body shape with broadening shoulders begin between the ages of 11 and 16. The voice also deepens. During this time, a boy may notice some temporary breast enlargement. This is completely normal, very common, and is no cause for concern. It will disappear with time. FACIAL AND CHEST HAIR Facial and chest hair appear at around age 17. The thickness of the beard is quite variable and depends on genes. Some men have little or no chest hair and very light beards, while others have dense growth. The amount of hair is unrelated to masculinity. ERECTIONS / EJACULATIONS Erections occur more often during puberty; sometimes a boy will have an erection for no apparent reason – this is common and normal. Ejaculation, the release of semen from the penis, begins during puberty. Like erections, ejaculation can occur for no obvious reason, especially during sleep. -

Loose Anagen Syndrome in a 2-Year-Old Female: a Case Report and Review of the Literature
Loose Anagen Syndrome in a 2-year-old Female: A Case Report and Review of the Literature Mathew Koehler, DO,* Anne Nguyen, MS,** Navid Nami, DO*** * Dermatology Resident, 2nd year, Opti-West/College Medical Center, Long Beach, CA ** Medical Student, 4th Year, Western University of Health Sciences, College of Osteopathic Medicine, Pomona, CA *** Dermatology Residency Program Director, Opti-West/College Medical Center, Long Beach, CA Abstract Loose anagen syndrome is a rare condition of abnormal hair cornification leading to excessive and painless loss of anagen hairs from the scalp. The condition most commonly affects young females with blonde hair, but males and those with darker hair colors can be affected. Patients are known to have short, sparse hair that does not need cutting, and hairs are easily and painlessly plucked from the scalp. No known treatment exists for this rare disorder, but many patients improve with age. Case Report neck line. The patient had no notable medical Discussion We present the case of a 27-month-old female history and took no daily medicines. An older Loose anagen syndrome is an uncommon presenting to the clinic with a chief complaint brother and sister had no similar findings. She condition characterized by loosely attached hairs of diffuse hair loss for the last five months. The was growing well and meeting all developmental of the scalp leading to diffuse thinning with poor mother stated that she began finding large clumps milestones. The mother denied any major growth, thus requiring few haircuts. It was first of hair throughout the house, most notably in the traumas, psychologically stressful periods or any described in 1984 by Zaun, who called it “syndrome child’s play area. -

Does Materialism Predict Body Hair Removal Among Undergraduate Males and Females? Brianna Ballew Grand Valley State University, [email protected]
Grand Valley State University ScholarWorks@GVSU Honors Projects Undergraduate Research and Creative Practice 4-2016 Does Materialism Predict Body Hair Removal Among Undergraduate Males and Females? Brianna Ballew Grand Valley State University, [email protected] Follow this and additional works at: http://scholarworks.gvsu.edu/honorsprojects Part of the Arts and Humanities Commons Recommended Citation Ballew, Brianna, "Does Materialism Predict Body Hair Removal Among Undergraduate Males and Females?" (2016). Honors Projects. 576. http://scholarworks.gvsu.edu/honorsprojects/576 This Open Access is brought to you for free and open access by the Undergraduate Research and Creative Practice at ScholarWorks@GVSU. It has been accepted for inclusion in Honors Projects by an authorized administrator of ScholarWorks@GVSU. For more information, please contact [email protected]. Materialist Values and Body Hair Removal 1 Running head: Materialist Values and Body Hair Removal Does Materialism Predict Body Hair Removal Among Undergraduate Males and Females? Brianna Ballew Grand Valley State University Faculty Advisor: Donna Henderson-King Ph.D. – Psychology Department 499 Honors Senior Project April, 2016 Materialist Values and Body Hair Removal 2 Abstract Previous research indicates that materialistic women are more likely to want to alter their bodies (Henderson-King & Brooks, 2009). This study focuses specifically on the relationship between materialism and body hair removal. We collected information about the frequency of body hair removal, reasons for hair removal, and materialism (Richins & Dawson, 1992). Findings indicate that males and females do not significantly differ on materialist values. Correlational analyses reveal that for women, materialism is related to frequency of hair removal for several body sites; for men, however, materialism was related to body hair removal for only a single site. -
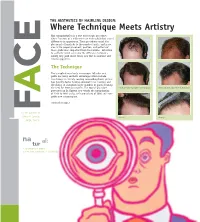
Where Technique Meets Artistry Hair Transplantation Is a True Microscopic Procedure, Where Fractions of a Millimeter Can Make Subtle but Critical
THE AESTHETICS OF HAIRLINE DESIGN: Where Technique Meets Artistry Hair transplantation is a true microscopic procedure, where fractions of a millimeter can make subtle but critical E differences in appearance. These procedures entail the placement of hundreds to thousands of grafts, and in no area is the proper placement, position, and pattern of these grafts more important than the hairline. Attention to aesthetic detail can make the difference between a merely very good result versus one that is excellent and natural appearing. C The Technique The transplanting of only microscopic follicular unit grafts has many aesthetic advantages which include: less damage to already existing surrounding hairs; greater hair density; faster healing; minimal to no scarring; and the ability to transplant larger numbers of grafts meaning the need for fewer procedures. The typical procedure Before and after a procedure of 2400 grafts Before and after a procedure of 2500 grafts performed by Dr. Epstein now entails the transplanting A of 2200 to 2400 grafts, with procedures of 3000 and more grafts now commonplace. continued on page 2 F For the patients of Jeffrey S. Epstein, Close-up Close-up M. D., F.A .C.S. na al: tur 1. As existing in nature 2. Free from pretension or artificiality WORDS FROM THE DOCTOR THE AESTHETICS OF HAIRLINE DESIGN (cont.) Since 1993, I have been fortunate to participate in the evolution The Aesthetics of the specialties of surgical hair The transplanted hairlines on this page all restoration and facial plastic demonstrate different aesthetic aspects of a natural a surgery. Few other surgical appearing hairline.