Traumatic Glaucoma Mimicking Primary Open Angle Glaucoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Long Term Follow-Up of Limbal Transplantation for Unilateral Chemical Injuries: 1997-2014 Nikolaos S
perim Ex en l & ta a l ic O Tsiklis et al., J Clin Exp Ophthalmol 2016, 7:6 p in l h t C h f Journal of Clinical & Experimental a o DOI: 10.4172/2155-9570.1000621 l m l a o n l o r g u y o J Ophthalmology ISSN: 2155-9570 ResearchResearch Article Article Open Access Long Term Follow-up of Limbal Transplantation for Unilateral Chemical Injuries: 1997-2014 Nikolaos S. Tsiklis1, Dimitrios S. Siganos2, Ahmed Lubbad3, Vassilios P. Kozobolis4 and Charalambos S. Siganos1,3* 1Department of Ophthalmology, Heraklion University Hospital, Greece 2Heraklion, Crete, Vlemma Eye Institute of Athens, Greece 3Laboratory of Vision and Optics, School of Medicine, University of Crete, Greece 4Eye Institute of Thrace, Democritus University, Alexandroupolis, Greece Abstract Purpose: To evaluate the long term results of limbal transplantation (LT) in patients with unilateral total limbal stem cell deficiency (LSCD) after chemical injury. Methods: The study includes 22 eyes of 22 consecutive patients (20 males and 2 females) who presented with total LSCD after unilateral chemical burns and underwent Limbal transplantation (LT) in the Cornea Service of the Depart- ment of Ophthalmology at the Heraklion University Hospital in Crete during the period from 1997 to 2014. All 22 cases underwent Conjunctival Limbal autogaft (CLAU) while in 14 surgeries it was combined with amniotic membrane trans- plantation (AMT). A second stage penetrating keratoplasty (PKP) was performed in 11 cases for visual rehabilitation. The healing time, the changes in VA and the stability of epithelial ocular surface integrity were looked for. Results: One case failed within 3 months of surgery, while the rest 21 eyes after CLAU maintained ocular surface epithelial integrity during the follow up period (7.8 ± 3.5 years), and showed improvement partially or totally in corneal neovascularization, symblepharon and ocular motility. -

Acute Management of Penetrating Eye Injury and Ruptured Globe
Acute management of penetrating eye injury and ruptured globe Disclaimer SEE ALSO: Endophthalmitis, Hyphaema, Peri- and post-operative Management of Penetrating Eye Injury and Ruptured Globe, Procedure for Management of Eye Trauma DESCRIPTION – The immediate management of penetrating eye injury (PEI), with or without intra-ocular foreign body (IOFB), and ruptured globe to maximise outcome. HOW TO ASSESS Red Flags: Immediate Advanced Trauma Life Support (ATLS) assessment: Airway, Breathing, Circulation, Disability, Exposure (ABCDE) Establish mechanism of injury to exclude other injuries which may require management at a general hospital, e.g. cervical spine, head injury Open globe should be examined carefully to avoid extrusion of intraocular contents Consider occult injury if mechanism suggestive Shield at all times (do not pad) Early referral for pre-anaesthetic assessment and medical review (if needed), to assess pre-existing or new medical issues and the patient’s suitability for management at RVEEH. Preoperative bloods, ECG and imaging as indicated. EXPECTED PATIENT Refer to and complete the ‘Emergency Expect Form’ (MR 37) in the Emergency Department. Make sure patient’s contact details (mobile) are recorded. Do not accept patients who have injuries other than ocular i.e. multi-trauma or who are medically unstable. Children under the age of 6 months should be referred directly to the Royal Children’s Hospital. Children aged from 6 months to 2 years with significant co-morbidities may not be appropriate to be managed at RVEEH. 1 Penetrating eye injury and ruptured globe CPG v4 19092017 All paediatric patients which may need referral to RCH, must be discussed with RCH Ophthalmology registrar or Consultant PRIOR to referral in order to confirm specialty coverage and operating theatre availability should surgery be required. -

CAUSES, COMPLICATIONS &TREATMENT of A“RED EYE”
CAUSES, COMPLICATIONS & TREATMENT of a “RED EYE” 8 Most cases of “red eye” seen in general practice are likely to be conjunctivitis or a superficial corneal injury, however, red eye can also indicate a serious eye condition such as acute angle glaucoma, iritis, keratitis or scleritis. Features such as significant pain, photophobia, reduced visual acuity and a unilateral presentation are “red flags” that a sight-threatening condition may be present. In the absence of specialised eye examination equipment, such as a slit lamp, General Practitioners must rely on identifying these key features to know which patients require referral to an Ophthalmologist for further assessment. Is it conjunctivitis or is it something more Iritis is also known as anterior uveitis; posterior uveitis is serious? inflammation of the choroid (choroiditis). Complications include glaucoma, cataract and macular oedema. The most likely cause of a red eye in patients who present to 4. Scleritis is inflammation of the sclera. This is a very rare general practice is conjunctivitis. However, red eye can also be presentation, usually associated with autoimmune a feature of a more serious eye condition, in which a delay in disease, e.g. rheumatoid arthritis. treatment due to a missed diagnosis can result in permanent 5. Penetrating eye injury or embedded foreign body; red visual loss. In addition, the inappropriate use of antibacterial eye is not always a feature topical eye preparations contributes to antimicrobial 6. Acid or alkali burn to the eye resistance. The patient history will usually identify a penetrating eye injury Most general practice clinics will not have access to specialised or chemical burn to the eye, but further assessment may be equipment for eye examination, e.g. -

Visual Outcomes of Hyphema in Closed Globe Injury, Managed at a Tertiary Care Institute
Jebmh.com Original Research Article Visual Outcomes of Hyphema in Closed Globe Injury, Managed at a Tertiary Care Institute Prasanta Kumar Nanda1, Jayaram Meher2, Bishnuprasad Rath3 1Professor and HOD, Department of Ophthalmology, SCB Medical College and Hospital, Cuttack, Odisha. 2Postgraduate Resident, Department of Ophthalmology, SCB Medical College and Hospital, Cuttack, Odisha. 3Postgraduate Resident, Department of Ophthalmology, SCB Medical College and Hospital, Cuttack, Odisha. ABSTRACT BACKGROUND An accumulation of blood in the anterior chamber is known as hyphema. An injury Corresponding Author: to the eye or its surrounding tissue, constitutes most of the calls for emergency in Dr. Jayaram Meher, SR Hostel, Room No. 166, ophthalmology. This study aims to determine the causes and visual outcome SCB Medical College and Hospital, following treatment in patients with hyphema following closed globe injury. Cuttack, Odisha. E-mail: [email protected] METHODS DOI: 10.18410/jebmh/2020/15 This is a prospective study involving 76 patients which done from February 2019 to September 2019 in the Department Of Ophthalmology. Detailed history was Financial or Other Competing Interests: None. taken regarding the type, mode of injury, duration of injury and the eye affected. Lid and adnexal injuries, visual acuity at the time of admission were recorded. How to Cite This Article: Detailed anterior segment evaluation on slit lamp was done. Appropriate treatment Nanda PK, Meher J, Rath B. Visual was given. The patients were followed after 1 week, and at the end of 6 weeks. outcomes of hyphema in closed globe injury, managed at a tertiary care RESULTS institute. J. Evid. Based Med. Healthc. 2020; 7(2), 68-72. -

SEEING Beyond Abuse
SEEING Beyond Abuse By Jessica L. Young, O.D. Pennsylvania Optometric Association’s 2010 Young Optometrist of the Year Many may think that visiting an eye doctor would be the last place for an abuse victim to go. After reading this article, you may disagree. One day, a 49 year- old woman came to see me for a routine eye examination. Her vision was getting a little worse and she thought, "Maybe I need a new pair of glasses." During the examination, I noticed a tear in the iris of her right eye. Upon checking her eye pressure I found that it was elevated in her right eye. I asked the woman if she had ever sustained any injuries to her eyes. She confirmed that she had in fact been hit many times in her eyes and face years ago by a former boyfriend. I explained how the trauma had damaged her eye and the increased eye pressure could lead to optic nerve damage and vision loss if left untreated. We decided to begin medicated eye drops to lower the eye pressure. So far the drops are successfully keeping the pressure down, reducing her chances of vision loss. This woman very well may have lost her eyesight had she not happened to come for a regular eye exam. Physical assault resulting in trauma to the eye can have both immediate and lasting effects. If trauma to the eye occurs, urgent medical attention should be sought to treat any immediate damage. Visiting an eye doctor is prudent for anyone who has ever sustained trauma to the eye at any time. -

Posterior Vitreous Detachment (PVD) and Retinal Tears
Posterior Vitreous Detachment (PVD) and Retinal Tears The space between your eye lens and your retina is filled with a clear, gel-like fluid called the vitreous. The vitreous is attached to your retina. As you age, the vitreous thins and may separate from the back of your eye. This is known as posterior vitreous detachment (PVD). PVD is usually harmless and causes floaters or flashes in the eye. PVD is very common and its incidence increases greatly with advancing age. In some cases, the tugging on the retina by the detached vitreous may cause the retina to tear. A tear in the retina can allow fluids to seep underneath the retina, causing the retina's sensory and pigment layers to separate and detach. This condition can cause great damage to your vision if it is not treated. A retinal detachment or retinal tear is considered an emergency and requires immediate medical attention. There are three types of retinal detachments… The most common type occurs when there is a break in the sensory layer of the retina, and fluid seeps underneath, causing the layers of the retina to separate. The second most common type occurs when the vitreous or scar tissue creates traction on the retina and pulls it loose. The third type is less common and happens when fluid collects underneath the layers of the retina and separates it from the back wall of the eye. Symptoms The symptoms most often associated with retinal detachment include… Flashes of light Vision that appears wavy or watery Vision obstructed as if by a veil or curtain Spots, called floaters, that look like bugs or spider webs and move as your eye moves Sudden change in your peripheral (side) vision Sudden decrease of vision If you experience any of these symptoms, call us immediately for an appointment. -

Understanding and Living with Glaucoma
Understanding and Living with Glaucoma Betty hopes future generations won’t have to live with glaucoma. Dr. Goldberg’s breakthrough research could mean they won’t have to. Understanding and Living with Glaucoma C SUPPORTED BY AN EDUCATIONAL GRANT FROM AERIE PHARMACEUTICALS, INC. Glaucoma is an eye disease that gradually steals your vision. Usually, glaucoma has no symptoms in its early stages. But without proper treatment glaucoma can lead to blindness. The good news is that with regular eye exams, early detection, and treatment, you can preserve your sight. This guide will give you a complete introduction to the facts about glaucoma. D Glaucoma Research Foundation 2 INTRODUCTION 3 UNDERSTANDING GLAUCOMA 3 Understand the Eye to Understand Glaucoma 4 How Glaucoma Affects the Eye 6 Who Gets Glaucoma? 7 Are There Symptoms? 7 When Should You Get Your Eyes Checked for Glaucoma? 8 DIFFERENT TYPES OF GLAUCOMA 8 Primary Open-Angle or Open-Angle Glaucoma 9 Primary Angle-Closure or Angle-Closure Glaucoma or Narrow-Angle Glaucoma 10 Other Types of Glaucoma 10 • Normal-Tension Glaucoma 10 • Secondary Glaucoma 12 DETECTING GLAUCOMA 12 How Is Glaucoma Diagnosed? 12 What To Expect During Glaucoma Examinations 12 • Tonometry 12 • Ophthalmoscopy 15 • Perimetry 16 • Gonioscopy 16 • Pachymetry 17 TREATING GLAUCOMA 17 Treatment of Primary Open-Angle Glaucoma 17 • Selective Laser Trabeculoplasty 18 • Glaucoma Medications 21 • Incisional Surgeries 25 • Unapproved Treatments 25 Treatment of Primary Angle-Closure Glaucoma 26 Treatment of Other Types of Glaucoma 28 FREQUENTLY ASKED QUESTIONS 30 LIVING WITH GLAUCOMA 30 Working with Your Doctor 32 Responding to Vision Changes Due to Glaucoma 32 Questions For Your Doctor 34 Your Lifestyle Counts 35 Looking Ahead 36 APPENDIX 36 A Guide To Glaucoma Medications 38 Glossary Understanding and Living with Glaucoma 1 Introduction If you have been diagnosed with glaucoma, or are a glaucoma suspect, you probably have a lot of questions and some concerns. -

Trauma-Induced Glaucoma
TRAUMA-INDUCED GLAUCOMA How to approach these patients. BY ADAM BOTWINICK, MD, AND REENA GARG, MD CASE PRESENTATION A 26-year-old man presented with pain and decreased vision in his right eye following blunt SPARKING CHANGE SPARKING head trauma. The patient’s BCVA was 20/80 OD and 20/20 OS, and IOP measured 30 mm Hg OD and 12 mm Hg OS via Goldman applanation tonometry. The exam showed a 2-mm hyphema in the right eye. Gonioscopy revealed angle recession superiorly and nasally; the view inferiorly was obstructed by the hyphema. A dilated fundus exam showed a 0.2 cup-to-disc ratio in both eyes. The patient started therapy with topical timolol and brimonidine. His IOP improved to 16 mm Hg. The hyphema resolved after 1 week with conservative therapy. He currently does not have glaucoma but will be monitored closely, given the degree of angle recession. BACKGROUND IRIS/ANGLE TRAUMA Ocular trauma is frequently seen in the emergency room Types of Injury setting.1 Often, the patient is a young man who sustained The most common injuries after blunt ocular trauma are injury during a sporting or domestic accident. Glaucoma is iridodialysis, cyclodialysis, and angle recession. a feared complication.2 The 6-month incidence of develop- Iridodialysis is disinsertion of the iris root, resulting in ing posttraumatic glaucoma can be as high as 3.4% and 2.7% corectopia and possibly associated angle damage. If there after blunt and penetrating ocular trauma, respectively.3,4 is accompanying angle damage, the IOP may be low or Traumatic glaucoma can be related to iris/angle trauma or high, depending on the extent of aqueous outflow and the hyphema in the anterior segment. -

Eye Injury As a Result of Coat Toggle Trauma
Eye (2007) 21, 94–95 & 2007 Nature Publishing Group All rights reserved 0950-222X/07 $30.00 www.nature.com/eye CASE SERIES Eye injury as a result CJ Vize, V Gauba and PL Atkinson of coat toggle trauma Abstract elasticated cord recoiled and struck him in the right eye. On initial examination, the patient had a Purpose To report the severity of ocular visual acuity of hand movements and a traumatic injury in three adults with blunt ocular trauma hyphaema of 1 mm depth with a poor fundal resulting from elastic corded coat toggles. view. The intraocular pressure was 14 mmHg. The Design Observational case series. hyphaema cleared over the next few weeks and Methods We retrospectively reviewed the revealed an underlying anterior subcapsular lens case records of all patients (n ¼ 3) with blunt opacity (Figure 2). His visual acuity by this stage ocular trauma secondary to elastic corded coat had improved to 6/18 (20/60) unaided, 6/5 toggles that presented to our department. (20/15) with a pinhole. Gonioscopy and fundal Results Injuries included traumatic exam were normal. The patient declined cataract hyphaema, cataract, angle recession, vitreous surgery and is under review. haemorrhage and retinal tears. Conclusions Significant ocular injury can result from elasticated coat toggles. The Case 2 general ophthalmologist should be aware of this new method of potentially sight A 67-year-old gentleman similarly suffered threatening trauma. injury to his right eye when trying to free his Eye (2007) 21, 94–95. doi:10.1038/sj.eye.6702181; coat toggle from the seatbelt mechanism in the published online 25 November 2005 back seat of a car. -
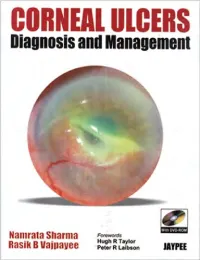
CORNEAL ULCERS Diagnosis and Management
CORNEAL ULCERS Diagnosis and Management System requirement: • Windows XP or above • Power DVD player (Software) • Windows Media Player 10.0 version or above • Quick time player version 6.5 or above Accompanying DVD ROM is playable only in Computer and not in DVD player. Kindly wait for few seconds for DVD to autorun. If it does not autorun then please do the following: • Click on my computer • Click the drive labelled JAYPEE and after opening the drive, kindly double click the file Jaypee CORNEAL ULCERS Diagnosis and Management Namrata Sharma MD DNB MNAMS Associate Professor of Ophthalmology Cornea, Cataract and Refractive Surgery Services Dr. Rajendra Prasad Centre for Ophthalmic Sciences All India Institute of Medical Sciences, New Delhi India Rasik B Vajpayee MS FRCSEd FRANZCO Head, Corneal and Cataract Surgery Centre for Eye Research Australia Royal Victorian Eye and Ear Hospital University of Melbourne Australia Forewords Hugh R Taylor Peter R Laibson ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD New Delhi • Ahmedabad • Bengaluru • Chennai • Hyderabad • Kochi • Kolkata • Lucknow • Mumbai • Nagpur Published by Jitendar P Vij Jaypee Brothers Medical Publishers (P) Ltd B-3 EMCA House, 23/23B Ansari Road, Daryaganj New Delhi 110 002, India Phones: +91-11-23272143, +91-11-23272703, +91-11-23282021, +91-11-23245672 Rel: +91-11-32558559, Fax: +91-11-23276490, +91-11-23245683 e-mail: [email protected] Visit our website: www.jaypeebrothers.com Branches • 2/B, Akruti Society, Jodhpur Gam Road Satellite Ahmedabad 380 015, Phones: +91-79-26926233, -

Traumatic Eye Injury in a 14-Year-Old Male
Osteopathic Family Physician (2017) 27 - 29 27 CLINICAL IMAGES Traumatic Eye Injury in a 14-Year-Old Male Lisa J. Hrushka, OMS-IV1 & Eric S. Wernsman, DO, FACOEP2 1 VCOM–Carolinas, Spartanburg, South Carolina 2 Clinical Faculty, VCOM–Carolinas, Spartanburg, South Carolina A 14-year-old caucasian male presents to the emergency department after being struck by a baseball to the left side of his face. The pa- tient reports that while playing the outfeld, he was hit by a line drive to the eye after losing the ball in the sun. He denies wearing glasses or contacts at the time of the injury. He complains of left eye pain and blurry vision but denies loss of consciousness or loss of vision after the accident. He also denies any nausea or vomiting. The patient describes his pain as throbbing which is made worse by eye-opening and bright lights. The patient has no other reported medical history. On physical examination, the patient is normocephalic with left periorbital ecchymosis and swelling to the left upper eyelid. Pupils are equal and reactive to light, and extraocular muscles are intact. A dark red fuid line is noted in the inferior anterior chamber of the left eye (Figure 1). The fuid line extends horizontally across the bottom third of the iris, almost to the level of the pupil. There is a distinct contrast in color to the iris; the natural green color is only visible above the level of the dark red fuid. There is no involvement of the sclera. The neck exam reveals no tenderness and the remainder of the physical exam is unremarkable. -

Retinal Detachment
Retinal Detachment: Background: Treatment: Usually, the vitreous moves away from the The retina is the layer of tis- • Floaters due to posterior vitreous de- retina without causing problems. However, sue in the back of the eye tachment are harmless, and usually sometimes it pulls hard enough to tear the that receives light and fade over time. retina in one or more places. communicates directly with • These do not require treatment and Fluid can pass through the the brain to form images. A surgery is rarely indicated. retinal tear, lifting the reti- healthy, intact retina gives • Vitamin therapy will not cure float- na off the back of the eye, you clear vision. ers. in what is referred to as ret- • If they annoy you, try to get them inal detachment. out of your field of vision by looking Vitreous is a clear gel up and down. Retinal Detachment poses a very serious that fills the middle of the threat to vision. In the rare case where surgery is neces- eye. Sometimes, tiny sary, a vitrectomy will be performed, Risks: clumps of gel cast shad- where the vitreous fluid will be re- ows on the retina, caus- placed with a salt solution. There is a • Nearsightedness; ing floaters, which you low risk of complications, such as: • Previous cataract, glaucoma or other may see as small dots, specks or clouds • Detached retina eye surgery; moving in your field of vision. These floaters • Cataracts may be annoying, but they should not inter- • Glaucoma medications that make the • Torn retina fere with your sight. pupil small (like pilocarpine) • Severe eye injury; Floaters can also be a sign of retinal A large floater, in certain types of light, can tear, which, if left untreated, can lead • Previous retinal detachment in the oth- cast a slight shadow over your vision.