Achilles Tendon Repair with Graft Jacket
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ankle Sprains Paediatric Management Advice Leaflet
Ankle Sprains Paediatric Management Advice Leaflet What is a sprained ankle? Ankle sprains occur when the ligaments around the foot and ankle are overstretched during an injury such as sudden twisting, which may cause some fibres to tear. The severity of the sprain will differ depending on how much stretch has occurred. What are the symptoms of a sprain? Pain around the joint. Swelling. Bruising. Pain when walking or moving. Pain relief Consult your GP or local pharmacist for advice as to which medication is suitable for your hil to take. Important signs and symptoms to look out for If your child experiences any of the following symptoms, please seek further urgent medical advice: Significant swelling Worsening, severe pain in the foot and ankle Severe night pain Night sweats Loss of sensation or persistent pins and needles/numbness in the foot/ankle/toes Abnormal weakness in the foot i.e. foot drop Altered colour or unusual sweating of the foot/ ankle Constant giving way or unable to weight bear through the foot/ankle Only continue to read if you have none of the above symptoms Paeds/Ankle sprain/ April 2020/ Page 1 of 4 Recovery and Rehabilitation Healing times Ankle sprains will usually heal within a few weeks with conservative management. Swelling and bruising may still be present for up to 10 days. Normal activity levels are usually restored after 6-8 weeks. The risk of re-injury is higher in the first 4-6 weeks. As your child completes the exercises provided they may notice some swelling and aching. -

Ankle Sprain
ANKLE SPRAIN What Is an Ankle Sprain? n ankle sprain is an injury to Anterior talofibular one or more ligaments in the Posterior A ligament ankle, usually on the outside of the talofibular ligament ankle. Ligaments are bands of tissue—like rubber bands—that Calcaneofibular ligament connect one bone to another and bind the joints together. In the ankle joint, ligaments provide stability by shoes, or walking or running on an surgeon for an appointment as limiting side-to-side movement. uneven surface. soon as possible. In the meantime, Some ankle sprains are much Sometimes ankle sprains occur immediately begin using the “R.I.C.E.” worse than others. The severity of because of weak ankles, a condition method—Rest, Ice, Compression, an ankle sprain depends on whether that some people are born with. and Elevation—to help reduce the ligament is stretched, partially Previous ankle or foot injuries can also swelling, pain, and further injury. torn, or completely torn, as well as on weaken the ankle and lead to sprains. the number of ligaments involved. Why Prompt Medical Ankle sprains are not the same as Signs and Symptoms Attention Is Needed strains, which affect muscles rather The signs and symptoms of ankle There are four key reasons why an than ligaments. sprains may include: ankle sprain should be promptly •Pain or soreness evaluated and treated by a foot and What Causes a •Swelling ankle surgeon: Sprained Ankle? • Bruising • First, an untreated ankle sprain Sprained ankles often result from a • Difficulty walking may lead to chronic ankle fall, a sudden twist, or a blow that • Stiffness in the joint instability,a condition marked by forces the ankle joint out of its persistent discomfort and a “giving normal position. -

Ankle Sprain Department Health • Care • People Fact Sheets
Emergency SeizureAnkle sprain Department health • care • people fact sheets www.health.qld.gov.au/emergency What is an ankle sprain? • Elevation - When resting, raise your foot so it is above the level of your heart. Ankle sprains happen to people of all ages. They occur when you ‘roll your ankle’, which over-stretches the liga- Avoid ‘HARM’ ments (the fibrous bands that hold the ankle together). • Heat - Increases blood flow and swelling • Alcohol - Increases blood flow and swelling, and can What are the symptoms? make you less aware of aggravating your injury When ligaments are damaged, there is pain, swelling and sometimes bruising. Too much swelling can slow the heal- • Reinjury - Protect your joint until it has healed ad- ing process. Pain is usually worst in the first two to three equately days. • Massage - Promotes blood flow and swelling. Massage can increase damage if begun too early. Treatment You may require an x-ray to determine if you have a bro- After 2-3 days ken bone (fracture). Your ankle should not swell or bruise further, but it will stay stiff and painful unless you gradually start to use it Significant injuries may require an ankle brace, or even a and exercise it. The following exercises will help. These plaster cast to allow ligaments to heal properly. exercises should be done twice a day or as often as your health care professional states: Some people who have repeated ankle sprains may need surgery to stabilize the weakened ligaments. Weight Bearing If you have pain, medications such as paracetamol (Pan- Start to walk as normally as possible without causing un- adol, Panamax), codeine, or a combination of both (pana- due pain (heel hits floor first, then toes; step forwards over deine) may help. -

Ankle Sprains: Assessment
Adopted: 2/1/16 Ankle Sprains: Assessment Background Ankle sprains are among the most common musculoskeletal injuries seen by health care providers. It is estimated that in the United States one in every 10,000 people sprains an ankle every hour, totaling nearly 30,000 ankle sprains per day. The incidence rates of ankle sprain range from 2.15 per 1000 person-years in the general population to 58.4 per 1000 person- years in physically active populations. They account for up to 40% of all athletic injuries and over half of the injuries occurring in basketball alone. Ankle sprains are also commonly seen in athletes participating in soccer, football, running and dance. (Prado 2014, Chan 2011, Waterman 2010) Despite the high prevalence and severity of lifestyle-limiting symptoms that follow the injury, ankle sprains are often regarded as benign injuries that will resolve on their own and therefore many people who suffer ankle sprains do not seek treatment from a healthcare provider. The incidence of residual symptoms following an acute ankle sprain varies, but has been reported with rates of between 40% and 50%. It is also reported that as many as 20% of acute ankle sprains develop chronic ankle instability (Chan, 2011). Ankle sprains in sport may result in varying degrees of debilitation including decreased performance, absence from competition and adverse psychological effects. Ankle sprains also have high economic costs associated with the diagnosis and treatment of the injury and loss of work productivity. It has been reported that one quarter of all people who sustain an ankle sprain are unable to attend school or work for more than 7 days following the initial injury . -

Ortho Symptoms Chart
3688 Veterans Memorial Dr. Hattiesburg, MS 39401 appointments, referrals & 2nd opinions: 601-554-7400 Online encyclopedia about orthopedics and spine care at: SouthernBoneandJoint.com UNDERSTANDING JOINT PAIN SYMPTOMS & WHEN YOU NEED TO SEE THE DOCTOR TRAUMA, FALL, FRACTURE: TRAUMA: Any time there is trauma (fall, impact, car accident) HAND: along with pain, a bone or joint could have fractured. NUMBNESS/WEAKNESS IN ARM / HAND: X-rays will be needed to check for broken bones. See an Numbness or weakness in the arm or hand can orthopedic specialist or an Emergency Room. be an emergency symptom related to a herniated disc in the neck. Left untreated, the symptom can become permanent. You should see a spine SHOULDER: specialist within 3 days. FROZEN SHOULDER can develop from NUMB FINGERS: Numbness in the tips of the overuse or inflammation. fingers can relate to Carpal Tunnel Syndrome. BURSITIS can make it difficult to raise the Watchful waiting with the use of a brace can be arm with twinges of pain. tried for a couple months. Numbness, if ignored TENDONITIS is inflammation of the over several months, can become permanent tendon which connects muscle to bone. and lifelong, along with weakness in grip. Self care for all three can include anti- Treatment can include a 30-minute surgery to inflammatories and R-I-C-E: Rest, Ice, relieve the tightness in the wrist. Compression & Elevation. Rest your shoulder for a day or so, using ice for 10 HIP PAIN not linked to dislocation due to trauma, fall or car minutes at a time. Compress the shoulder accident, is often linked to bursitis (inflammation of the joint) snugly with an elastic band (not tightly) or degeneration of the hip joint due to arthritis which damages and lie down with the shoulder elevated. -
Sports-Related Injuries Can Occur As the Result of a Single Traumatic Event, Such As an Impact Or Fall, Or from Repeated Overuse
COMMON SPORTS INJURIES Sports-related injuries can occur as the result of a single traumatic event, such as an impact or fall, or from repeated overuse and strain on muscles, tendons, and/or ligaments. Here are a few of the most common sports injuries. BICEPS FEMORIS (LONG HEAD) PULLING YOUR LEG Strains and sprains make up the bulk of sports injuries. Strains happen when muscles or SEMITENDINOSUS tendons are overstretched or torn - if someone has a pulled muscle, that means they have a muscle strain. The most commonly strained muscles are the hamstrings. SEMIMEMBRANOSUS Strains are best prevented by proper stretching, strengthening, and proper warm-ups before athletic activity. 2 SPRAIN, SPRAIN GO AWAY ANTERIOR TALOFIBULAR LIGAMENT Sprains happen when ligaments (PARTIALLY TORN) are overstretched or torn. Sprained ankles often happen when a fall or awkward landing from a jump forces the ankle joint to move in an unusual way, stressing or possibly tearing the ligaments surrounding it. Walking, running, or jumping on an uneven surface can also cause a sprained ankle. Stretching, strengthening, and balance exercises (as well as supportive footwear) can help reduce the risk of ankle sprains. 3 YOU’RE FEMUR TEARING ME APART! Many other muscles, tendons, and ligaments frequently tear. ACL (anterior cruciate ligament tears tend to happen in sports that put stress on the knees through jumping, sudden stops, and rapid changes in direction. Keeping the strength of hamstring PATELLA and quadriceps muscles balanced and (KNEECAP) TIBIA practicing safe landing and pivoting techniques can help prevent ACL tears. Factoid! Around 55% of sports-related injuries involve the knees. -

Foot and Ankle Injury After Hours Telephone Triage Protocols | Adult | 2017
Foot and Ankle Injury After Hours Telephone Triage Protocols | Adult | 2017 DEFINITION ⦁ Injuries to a bone, muscle, joint, or ligament of the ankle and foot ⦁ Associated skin and soft tissue injuries are also included INITIAL ASSESSMENT QUESTIONS 1. MECHANISM: "How did the injury happen?" (e.g., twisting injury, direct blow) 2. ONSET: "When did the injury happen?" (Minutes or hours ago) 3. LOCATION: "Where is the injury located?" 4. APPEARANCE of INJURY: "What does the injury look like?" 5. WEIGHT-BEARING: "Can you put weight on that foot?" "Can you walk (four steps or more)?" 6. SIZE: For cuts, bruises, or swelling, ask: "How large is it?" (e.g., inches or centimeters; entire joint) 7. PAIN: "Is there pain?" If so, ask: "How bad is the pain?" (e.g., Scale 1-10; or mild, moderate, severe) 8. TETANUS: For any breaks in the skin, ask: "When was the last tetanus booster?" 9. OTHER SYMPTOMS: "Do you have any other symptoms?" 10. PREGNANCY: "Is there any chance you are pregnant?" "When was your last menstrual period?" TRIAGE ASSESSMENT QUESTIONS Call EMS 911 Now Serious injury with multiple fractures CA: 40, 1 [1] Major bleeding (e.g., actively dripping or spurting) AND [2] can't be stopped FIRST AID: Apply direct pressure to the entire wound with a clean cloth. CA: 40, 13, 1 Amputation FIRST AID: Apply direct pressure to the entire wound with a clean cloth. CA: 40, 13, 20, 1 Looks like a dislocated joint (very crooked or deformed) Reason: If dislocated, adult will be unable to walk at all. -

Rotator Cuff Tendinitis Shoulder Joint Replacement Mallet Finger Low
We would like to thank you for choosing Campbell Clinic to care for you or your family member during this time. We believe that one of the best ways to ensure quality care and minimize reoccurrences is through educating our patients on their injuries or diseases. Based on the information obtained from today's visit and the course of treatment your physician has discussed with you, the following educational materials are recommended for additional information: Shoulder, Arm, & Elbow Hand & Wrist Spine & Neck Fractures Tears & Injuries Fractures Diseases & Syndromes Fractures & Other Injuries Diseases & Syndromes Adult Forearm Biceps Tear Distal Radius Carpal Tunnel Syndrome Cervical Fracture Chordoma Children Forearm Rotator Cuff Tear Finger Compartment Syndrome Thoracic & Lumbar Spine Lumbar Spine Stenosis Clavicle Shoulder Joint Tear Hand Arthritis of Hand Osteoporosis & Spinal Fx Congenital Scoliosis Distal Humerus Burners & Stingers Scaphoid Fx of Wrist Dupuytren's Comtracture Spondylolysis Congenital Torticollis Shoulder Blade Elbow Dislocation Thumb Arthritis of Wrist Spondylolisthesis Kyphosis of the Spine Adult Elbow Erb's Palsy Sprains, Strains & Other Injuries Kienböck's Disease Lumbar Disk Herniation Scoliosis Children Elbow Shoulder Dislocation Sprained Thumb Ganglion Cyst of the Wrist Neck Sprain Scoliosis in Children Diseases & Syndromes Surgical Treatments Wrist Sprains Arthritis of Thumb Herniated Disk Pack Pain in Children Compartment Syndrome Total Shoulder Replacement Fingertip Injuries Boutonnière Deformity Treatment -

ANKLE SPRAIN Home Exercises
ANKLE SPRAIN Home Exercises An ankle sprain occurs when the strong ligaments that support the ankle stretch beyond their limits and tear. Ankle sprains are common injuries that occur among people of all ages. They range from mild to severe, depending on how much damage there is to the ligament(s). Most sprains are minor injuries that heal with home treatments, like rest and applying ice. However, if your ankle is very swollen and painful to walk on, or if you are having trouble putting weight on your ankle at all, be sure to see your doctor. Without proper treatment and rehabilitation, a more severe sprain can weaken your ankle—making it more likely that you will injure it again. Repeated ankle sprains can lead to long-term problems, including chronic ankle pain, arthritis, and ongoing instability. Normal anatomy of the foot and ankle An ankle sprain is an injury to one or more of the ligaments that stabilize the ankle. A twisting force to the lower leg or foot can cause a sprain. The lateral ligaments on the outside of the ankle are injured most frequently. Description Ligaments are strong, fibrous tissues that connect bones to other bones. The ligaments in the ankle help to keep the bones in proper position and stabilize the joint. Sprains can range from tiny tears in the fibers that make up the ligament to complete tears through the tissue. If there is a complete tear of the ligament, the ankle may become unstable after the initial injury phase passes. Over time, this instability can result in damage to the bones and cartilage of the ankle joint. -

Sprained Ankle Introduction
Sprained Ankle Introduction A sprain occurs when a ligament connecting bones or cartilage is ruptured or torn. Quick and proper care can ensure the road to a safe and moderately quick return to activity without chronic setbacks. Signs and Symptoms A first-degree sprain has minimal swelling and discoloration. Ligaments are stretched but not torn. A second-degree sprain involves partial tearing of the ligament, increased pain, swelling, discoloration, and instability. A third-degree sprain indicates that the fibers are torn completely, causing gross instability of the ankle as well as discoloration, pain, and much swelling. Treatment Mild sprains may be treated at home by following the “RICE” procedure. Rest: It is important to stay off the ankle as much as possible to allow it to heal. Ice: The ankle needs to be iced for 15 to 20 minutes using crushed ice cubes or a package of frozen vegetables. A layer of material may be used between the ice and the ankle. Use ice for 20 minutes and then off for 45 minutes until bedtime. Resume ice on the second day as needed. Compression: Remove ice and wrap ankle with elastic ace bandage. Elevation: Keep the ankle above the heart when resting at home. Avoid use of the injured ankle by using crutches as soon as possible. Taking time to let your sprained ankle heal will help prevent further pain and injury. You can walk on the ankle as soon as it feels comfortable. More severe sprains should be seen by a physician or nurse practitioner. You may be referred to a physical therapist where they will implement progressive exercises. -
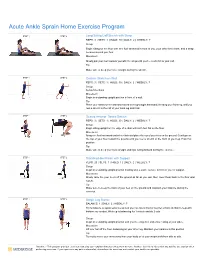
Acute Ankle Sprain Home Exercise Program
Acute Ankle Sprain Home Exercise Program STEP 1 STEP 2 Long Sitting Calf Stretch with Strap REPS: 3 | SETS: 1 | HOLD: 30 | DAILY: 2 | WEEKLY: 7 Setup Begin sitting on the floor with one foot stretched in front of you, your other knee bent, and a strap secured around your foot. Movement Slowly pull your foot towards you with the strap until you feel a stretch in your calf. Tip Make sure to keep your knee straight during the stretch. STEP 1 STEP 2 Gastroc Stretch on Wall REPS: 3 | SETS: 1 | HOLD: 30 | DAILY: 2 | WEEKLY: 7 Setup Setup Directions Movement Begin in a standing upright position in front of a wall. Tip Place your hands on the wall and extend one leg straight backward, bending your front leg, until you feel a stretch in the calf of your back leg and hold. STEP 1 STEP 2 Seated Anterior Tibialis Stretch REPS: 3 | SETS: 1 | HOLD: 30 | DAILY: 2 | WEEKLY: 7 Setup Begin sitting upright on the edge of a chair with both feet flat on the floor. Movement Bring one foot backward under the chair and place the top of your toes on the ground. Gently press the top of your foot toward the ground until you feel a stretch in the front of your leg. Hold this position. Tip Make sure to keep your back straight and hips facing forward during the exercise. STEP 1 STEP 2 Standing Heel Raise with Support REPS: 20 | SETS: 1 | HOLD: 1 | DAILY: 2 | WEEKLY: 7 Setup Begin in a standing upright position holding onto a stable surface in front of you for support. -

Ankle Sprains Ankle Sprains Occur When One Or More of the Ankle Ligaments Is Stretched Or Torn
Ankle Sprains Ankle sprains occur when one or more of the ankle ligaments is stretched or torn. Ligaments are the strong bands that connect the bones of the ankle. A sprain can range from a mild injury involving only stretched ligaments to a serious injury where ligaments or bone chips can be torn away. Generally, you can judge the seriousness of the problem by the ankle’s response to home treatment. Pain and swelling are the most common symptoms of a sprained ankle. The swelling is generally followed in a few days by bruising. The best way to prevent ankle sprains is by wearing comfortable, well-fitted shoes that provide good ankle support, and making sure that you can always see where you’re going. High-heeled shoes are not recommended. If you think you have sprained your ankle, start the R-I-C-E, or R.I.C.E., treatment immediately. R.I.C.E. stands for Rest, Ice, Compression, and Elevation. Let’s take each one of these in turn but slightly out of order: · Rest. Do not walk or put weight on the injured ankle if you can’t walk without pain in a proper heel- toe fashion with your toe pointing straight ahead. When it’s like this, your ankle needs total rest for one or two days. Use crutches if necessary. · Ice. Apply an ice or a cold pack to the injured area for ten minutes every hour for the first 72 hours. After that, apply ice for 15 or 20 minutes three times a day until all the swelling and pain is gone.