Chapter 4 Prevention of Trichinella Infection in the Domestic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
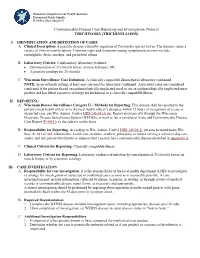
Trichinosis (Trichinellosis) Case Reporting and Investigation Protocol
Wisconsin Department of Health Services Division of Public Health P-01912 (Rev 08/2017) Communicable Disease Case Reporting and Investigation Protocol TRICHINOSIS (TRICHINELLOSIS) I. IDENTIFICATION AND DEFINITION OF CASES A. Clinical Description: A parasitic disease caused by ingestion of Trichinella species larvae. The disease causes a variety of clinical manifestations. Common signs and symptoms among symptomatic persons include eosinophilia, fever, myalgia, and periorbital edema. B. Laboratory Criteria: Confirmatory laboratory evidence: • Demonstration of Trichinella larvae on muscle biopsy, OR • A positive serology for Trichinella. C. Wisconsin Surveillance Case Definition: A clinically compatible illness that is laboratory confirmed. NOTE: In an outbreak setting, at least one case must be laboratory confirmed. Associated cases are considered confirmed if the patient shared an epidemiologically implicated meal or ate an epidemiologically implicated meat product and has either a positive serology for trichinosis or a clinically compatible illness. II. REPORTING A. Wisconsin Disease Surveillance Category II – Methods for Reporting: This disease shall be reported to the patient’s local health officer or to the local health officer’s designee within 72 hours of recognition of a case or suspected case, per Wis. Admin. Code § DHS 145.04 (3) (b). Report electronically through the Wisconsin Electronic Disease Surveillance System (WEDSS), or mail or fax a completed Acute and Communicable Disease Case Report (F-44151) to the address on the form. B. Responsibility for Reporting: According to Wis. Admin. Code § DHS 145.04(1), persons licensed under Wis. Stat. ch. 441 or 448, laboratories, health care facilities, teachers, principals, or nurses serving a school or day care center, and any person who knows or suspects that a person has a communicable disease identified in Appendix A. -

November 2016 NEMSN Newsletter
Vol. Vol. 26 No.No. 1 1 The National Eosinophilia-Myalgia Syndrome Network, Inc. November Page 2016 1 Friends Supporting Friends National EMS Network NEMSN National Eosinophilia-Myalgia Syndrome Network, Inc. http:www.nemsn.org Newsletter Points of interest ………………..……………... NEMSN is extremely pleased to announce that Stephen Naylor, • Your continued do- Ph.D. has joined our Medical Advisory Panel as NEMSN's nations have kept Science Advisor. Welcome, Dr. Naylor. this Newsletter and NEMSN alive. Dr. Stephen Naylor is one of only a handful of distin- Please keep those guished scientists who have devoted years of research in donations coming an attempt to achieve a complete explanation of EMS. no matter how Known as a chemist, biochemist, toxicologist and business large or small. Our originator, he has co-authored hundreds of scientific re- thanks. search papers and book chapters while delivering un- ………………………………….. counted presentations at universities and medical centers • We are interested worldwide. In the 1990s he and NEMSN advisor Gerald J. in your story. Please Gleich, M.D. partnered at the Mayo Clinic in Rochester, take the time to MN to undertake definitive EMS and L-tryptophan re- write it and send to search. Naylor and Gleich received NIH and WHO grants us for our newslet- and co-authored a number of scholarly papers during that period. ter. …………………………………... Stephen Naylor received his Ph.D. from the University of Cambridge (UK) in Biochem- • If you have not seen istry. He completed postdoctoral work at the Massachusetts Institute of Technology our web site yet, it where he later became a visiting faculty member in the Division of Biological Engineer- is very informative. -

Day 1 Review
Day 1 Review • All food service establishments must have a current and valid permit issued by the New York City Health Department. • Health inspectors have the right to inspect any operating food service or food processing establishment. Inspectors must be given access to all areas of the establishment during an inspection. • According to the New York City Health Code, supervisors of all food service establishments must have a Food Protection Certificate. • Food is any edible substance, ice, beverage or ingredient used or sold for human consumption. • Potentially Hazardous Foods (PHFs) are foods which support rapid growth of microorganisms. • Examples of PHFs include all raw and cooked meats, poultry, milk and milk products, fish, shellfish, tofu, cooked rice, pasta, beans, potatoes and garlic in oil. • The Temperature Danger Zone is between 41°F and 140°F. Within this range, most harmful microorganisms reproduce rapidly. • The three types of thermometers that can be used for measuring food temperatures are: bimetallic stem (range from 0°F to 220°F), thermocouple and thermistor (digital). The use of glass thermometers in a food service establishment is prohibited by law. • Meat inspected by the Unites States Department of Agriculture (USDA) must have a USDA inspection stamp. • Smoked fish must be held at or below 38°F to prevent the growth of the bacteria Clostridium botulinum. • Shellfish must be received with shellfish tags. These tags must be kept on file for at least 90 days after the product is used. • Milk and milk products must either be pasteurized, with sell-by dates of 9 days, or ultra-pasteurized, with sell-by dates of 45 days. -

2016 New Jersey Reportable Communicable Disease Report (January 3, 2016 to December 31, 2016) (Excl
10:34 Friday, June 30, 2017 1 2016 New Jersey Reportable Communicable Disease Report (January 3, 2016 to December 31, 2016) (excl. Sexually Transmitted Diseases, HIV/AIDS and Tuberculosis) (Refer to Technical Notes for Reporting Criteria) Case Jurisdiction Disease Counts STATE TOTAL AMOEBIASIS 98 STATE TOTAL ANTHRAX 0 STATE TOTAL ANTHRAX - CUTANEOUS 0 STATE TOTAL ANTHRAX - INHALATION 0 STATE TOTAL ANTHRAX - INTESTINAL 0 STATE TOTAL ANTHRAX - OROPHARYNGEAL 0 STATE TOTAL BABESIOSIS 174 STATE TOTAL BOTULISM - FOODBORNE 0 STATE TOTAL BOTULISM - INFANT 10 STATE TOTAL BOTULISM - OTHER, UNSPECIFIED 0 STATE TOTAL BOTULISM - WOUND 1 STATE TOTAL BRUCELLOSIS 1 STATE TOTAL CALIFORNIA ENCEPHALITIS(CE) 0 STATE TOTAL CAMPYLOBACTERIOSIS 1907 STATE TOTAL CHIKUNGUNYA 11 STATE TOTAL CHOLERA - O1 0 STATE TOTAL CHOLERA - O139 0 STATE TOTAL CREUTZFELDT-JAKOB DISEASE 4 STATE TOTAL CREUTZFELDT-JAKOB DISEASE - FAMILIAL 0 STATE TOTAL CREUTZFELDT-JAKOB DISEASE - IATROGENIC 0 STATE TOTAL CREUTZFELDT-JAKOB DISEASE - NEW VARIANT 0 STATE TOTAL CREUTZFELDT-JAKOB DISEASE - SPORADIC 2 STATE TOTAL CREUTZFELDT-JAKOB DISEASE - UNKNOWN 1 STATE TOTAL CRYPTOSPORIDIOSIS 198 STATE TOTAL CYCLOSPORIASIS 29 STATE TOTAL DENGUE FEVER - DENGUE 43 STATE TOTAL DENGUE FEVER - DENGUE-LIKE ILLNESS 3 STATE TOTAL DENGUE FEVER - SEVERE DENGUE 4 STATE TOTAL DIPHTHERIA 0 STATE TOTAL EASTERN EQUINE ENCEPHALITIS(EEE) 1 STATE TOTAL EBOLA 0 STATE TOTAL EHRLICHIOSIS/ANAPLASMOSIS - ANAPLASMA PHAGOCYTOPHILUM (PREVIOUSLY HGE) 109 STATE TOTAL EHRLICHIOSIS/ANAPLASMOSIS - EHRLICHIA CHAFFEENSIS (PREVIOUSLY -

Onchocerciasis
11 ONCHOCERCIASIS ADRIAN HOPKINS AND BOAKYE A. BOATIN 11.1 INTRODUCTION the infection is actually much reduced and elimination of transmission in some areas has been achieved. Differences Onchocerciasis (or river blindness) is a parasitic disease in the vectors in different regions of Africa, and differences in cause by the filarial worm, Onchocerca volvulus. Man is the the parasite between its savannah and forest forms led to only known animal reservoir. The vector is a small black fly different presentations of the disease in different areas. of the Simulium species. The black fly breeds in well- It is probable that the disease in the Americas was brought oxygenated water and is therefore mostly associated with across from Africa by infected people during the slave trade rivers where there is fast-flowing water, broken up by catar- and found different Simulium flies, but ones still able to acts or vegetation. All populations are exposed if they live transmit the disease (3). Around 500,000 people were at risk near the breeding sites and the clinical signs of the disease in the Americas in 13 different foci, although the disease has are related to the amount of exposure and the length of time recently been eliminated from some of these foci, and there is the population is exposed. In areas of high prevalence first an ambitious target of eliminating the transmission of the signs are in the skin, with chronic itching leading to infection disease in the Americas by 2012. and chronic skin changes. Blindness begins slowly with Host factors may also play a major role in the severe skin increasingly impaired vision often leading to total loss of form of the disease called Sowda, which is found mostly in vision in young adults, in their early thirties, when they northern Sudan and in Yemen. -
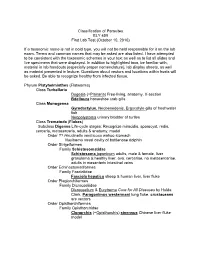
Classification of Parasites BLY 459 First Lab Test (October 10, 2010)
Classification of Parasites BLY 459 First Lab Test (October 10, 2010) If a taxonomic name is not in bold type, you will not be held responsible for it on the lab exam. Terms and common names that may be asked are also listed. I have attempted to be consistent with the taxonomic schemes in your text as well as to list all slides and live specimens that were displayed. In addition to highlighted taxa, be familiar with, material in lab handouts (especially proper nomenclature), lab display sheets, as well as material presented in lecture. Questions about vectors and locations within hosts will be asked. Be able to recognize healthy from infected tissue. Phylum Platyhelminthes (Flatworms) Class Turbellaria Dugesia (=Planaria ) Free-living, anatomy, X-section Bdelloura horseshoe crab gills Class Monogenea Gyrodactylus , Neobenedenis, Ergocotyle gills of freshwater fish Neopolystoma urinary bladder of turtles Class Trematoda ( Flukes ) Subclass Digenea Life-cycle stages: Recognize miracidia, sporocyst, redia, cercaria , metacercaria, adults & anatomy, model Order ?? Hirudinella ventricosa wahoo stomach Nasitrema nasal cavity of bottlenose dolphin Order Strigeiformes Family Schistosomatidae Schistosoma japonicum adults, male & female, liver granuloma & healthy liver, ova, cercariae, no metacercariae, adults in mesenteric intestinal veins Order Echinostomatiformes Family Fasciolidae Fasciola hepatica sheep & human liver, liver fluke Order Plagiorchiformes Family Dicrocoeliidae Dicrocoelium & Eurytrema Cure for All Diseases by Hulda Clark, Paragonimus -

Tissue Nematode: Trichenella Spiralis
Tissue nematode: Trichenella spiralis Introduction Trichinella spiralis is a viviparous nematode parasite, occurring in pigs, rodents, bears, hyenas and humans, and is liable for the disease trichinosis. It is occasionally referred to as the "pork worm" as it is characteristically encountered in undercooked pork foodstuffs. It should not be perplexed with the distantly related pork tapeworm. Trichinella species, the small nematode parasite of individuals, have an abnormal lifecycle, and are one of the most extensive and clinically significant parasites in the whole world. The adult worms attain maturity in the small intestine of a definitive host, such as pig. Each adult female gives rise to batches of live larvae, which bore across the intestinal wall, enter the blood stream (to feed on it) and lymphatic system, and are passed to striated muscle. Once reaching to the muscle, they encyst, or become enclosed in a capsule. Humans can become infected by eating contaminated pork, horse meat, or wild carnivorus animals such as cat, fox, or bear. Epidemology Trichinosis is a disease caused by the worm. It occurs around most parts of the world, and infects majority of humans. It ranges from North America and Europe, to Japan, China and Tropical Africa. Morphology Males of T. spiralis measure about1.4 and 1.6 mm long, and are more flat at anterior end than posterior end. The anus is seen in the terminal position, and they have a large copulatory pseudobursa on both the side. The females of T. spiralis are nearly twice the size of the males, and have an anal aperture situated terminally. -

Lecture 5: Emerging Parasitic Helminths Part 2: Tissue Nematodes
Readings-Nematodes • Ch. 11 (pp. 290, 291-93, 295 [box 11.1], 304 [box 11.2]) • Lecture 5: Emerging Parasitic Ch.14 (p. 375, 367 [table 14.1]) Helminths part 2: Tissue Nematodes Matt Tucker, M.S., MSPH [email protected] HSC4933 Emerging Infectious Diseases HSC4933. Emerging Infectious Diseases 2 Monsters Inside Me Learning Objectives • Toxocariasis, larva migrans (Toxocara canis, dog hookworm): • Understand how visceral larval migrans, cutaneous larval migrans, and ocular larval migrans can occur Background: • Know basic attributes of tissue nematodes and be able to distinguish http://animal.discovery.com/invertebrates/monsters-inside- these nematodes from each other and also from other types of me/toxocariasis-toxocara-roundworm/ nematodes • Understand life cycles of tissue nematodes, noting similarities and Videos: http://animal.discovery.com/videos/monsters-inside- significant difference me-toxocariasis.html • Know infective stages, various hosts involved in a particular cycle • Be familiar with diagnostic criteria, epidemiology, pathogenicity, http://animal.discovery.com/videos/monsters-inside-me- &treatment toxocara-parasite.html • Identify locations in world where certain parasites exist • Note drugs (always available) that are used to treat parasites • Describe factors of tissue nematodes that can make them emerging infectious diseases • Be familiar with Dracunculiasis and status of eradication HSC4933. Emerging Infectious Diseases 3 HSC4933. Emerging Infectious Diseases 4 Lecture 5: On the Menu Problems with other hookworms • Cutaneous larva migrans or Visceral Tissue Nematodes larva migrans • Hookworms of other animals • Cutaneous Larva Migrans frequently fail to penetrate the human dermis (and beyond). • Visceral Larva Migrans – Ancylostoma braziliense (most common- in Gulf Coast and tropics), • Gnathostoma spp. Ancylostoma caninum, Ancylostoma “creeping eruption” ceylanicum, • Trichinella spiralis • They migrate through the epidermis leaving typical tracks • Dracunculus medinensis • Eosinophilic enteritis-emerging problem in Australia HSC4933. -

STUDY of PARASITIC INFESTATION and ITS EFFECT on the HEALTH STATUS of PRIMARY SCHOOL CHILDREN in TANTA CITY Nour Abd El Azize Mohammed Mealy, Prof
STUDY OF PARASITIC INFESTATION AND ITS EFFECT ON THE HEALTH STATUS OF PRIMARY SCHOOL CHILDREN IN TANTA CITY Nour Abd El Azize Mohammed Mealy, Prof. Dr. Nadia Yahia Ismaiel, Prof. Dr. Hassan Saad Abu Saif, Prof. Dr. Wael Refaat Hablas STUDY OF PARASITIC INFESTATION AND ITS EFFECT ON THE HEALTH STATUS OF PRIMARY SCHOOL CHILDREN IN TANTA CITY By Nour Abd El Azize Mohammed Mealy, Prof. Dr. Nadia Yahia Ismaiel*, Prof. Dr. Hassan Saad Abu Saif*, Prof. Dr. Wael Refaat Hablas** Pediatric*& Clinical Pathology** Depts. Al-Azhar University- Faculty of Medicine ABSTRACT Background: School age children are one of the groups at high-risk for intestinal parasitic infestations. Factors like poor developments of hygienic habits, immune system and over-crowding contributes for infestation. The adverse effects of intestinal parasites among children are diverse and alarming. Intestinal parasitic infestations have detrimental effects on the survival, appetite, growth and physical fitness, school attendance and cognitive performance of school age children (Alemu et al., 2011). Objectives: We aimed to 1. Assess the prevalence of parasitic infestation and its effect on the health status of primary school children in Tanta City (5 schools from 3 areas at Tanta city) 2. Determine the prevalence of intestinal parasitic infestation among primary school children in some urban communities of Tanta City 3. Identify associated risk factors of school children for parasitic infestations in some urban communities of Tanta City. Design: This is descriptive cross sectional study that was carried out on 1000 students (boys &girls) at governmental primary schools at Tanta rural areas. This research was continued until fulfillment of the study from April 2017 to May 2018. -

Anti-Trichinella Antibodies in Breeding Pigs Farmed Under Controlled
Pozio et al. Parasites Vectors (2021) 14:417 https://doi.org/10.1186/s13071-021-04920-1 Parasites & Vectors RESEARCH Open Access Animal welfare and zoonosis risk: anti-Trichinella antibodies in breeding pigs farmed under controlled housing conditions Edoardo Pozio1, Mario Celli2, Alessandra Ludovisi1, Maria Interisano1, Marco Amati1 and Maria Angeles Gómez‑Morales1* Abstract Background: Domesticated pigs are the main source of Trichinella sp. infections for humans, particularly when reared in backyards or free‑ranging. In temperate areas of southern Europe, most pigs are farmed under controlled housing conditions, but sows and sometimes fattening pigs have access to outdoors to improve animal welfare. The aim of the present study was to investigate whether outdoor access of breeding pigs farmed under controlled housing conditions can represent a risk for Trichinella sp. transmission when the farm is located in an agricultural area interspersed with wooded areas and badlands, where Trichinella spp. could be present in wildlife. Methods: Serum samples were collected from 63 breeding sows and one boar before and after their access to an open fenced area for 2 months and from 84 pigs that never had outdoor access. Samples were screened for anti‑Trich- inella antibodies by ELISA, and positive sera were confrmed using Western blot (Wb) excretory/secretory antigens. To detect Trichinella sp. larvae, muscle tissues from serologically positive and negative pigs were tested by artifcial digestion. Results: Thirteen (20.6%) sows and one boar tested positive with both ELISA and Wb. No larvae were detected in muscle samples of serologically positive and serologically negative pigs. Positive serum samples were then tested by Wb using crude worm extract as antigens. -

New Aspects of Human Trichinellosis: the Impact of New Trichinella Species F Bruschi, K D Murrell
15 REVIEW Postgrad Med J: first published as 10.1136/pmj.78.915.15 on 1 January 2002. Downloaded from New aspects of human trichinellosis: the impact of new Trichinella species F Bruschi, K D Murrell ............................................................................................................................. Postgrad Med J 2002;78:15–22 Trichinellosis is a re-emerging zoonosis and more on anti-inflammatory drugs and antihelminthics clinical awareness is needed. In particular, the such as mebendazole and albendazole; the use of these drugs is now aided by greater clinical description of new Trichinella species such as T papuae experience with trichinellosis associated with the and T murrelli and the occurrence of human cases increased number of outbreaks. caused by T pseudospiralis, until very recently thought to The description of new Trichinella species, such as T murrelli and T papuae, as well as the occur only in animals, requires changes in our handling occurrence of outbreaks caused by species not of clinical trichinellosis, because existing knowledge is previously recognised as infective for humans, based mostly on cases due to classical T spiralis such as T pseudospiralis, now render the clinical picture of trichinellosis potentially more compli- infection. The aim of the present review is to integrate cated. Clinicians and particularly infectious dis- the experiences derived from different outbreaks around ease specialists should consider the issues dis- the world, caused by different Trichinella species, in cussed in this review when making a diagnosis and choosing treatment. order to provide a more comprehensive approach to diagnosis and treatment. SYSTEMATICS .......................................................................... Trichinellosis results from infection by a parasitic nematode belonging to the genus trichinella. -

From Lisheen Stud Lord Gayle Sir Gaylord Sticky Case Lord Americo Hynictus Val De Loir Hypavia Roselier Misti IV Peace Rose QUAR
From Lisheen Stud 1 1 Sir Gaylord Lord Gayle Sticky Case Lord Americo Val de Loir QUARRYFIELD LASS Hynictus (IRE) Hypavia (1998) Misti IV Right Then Roselier Bay Mare Peace Rose Rosie (IRE) No Argument (1991) Right Then Esplanade 1st dam RIGHT THEN ROSIE (IRE): placed in a point-to-point; dam of 6 foals; 3 runners; 3 winners: Quarryfield Lass (IRE) (f. by Lord Americo): see below. Graduand (IRE) (g. by Executive Perk): winner of a N.H. Flat Race and placed twice; also placed over hurdles. Steve Capall (IRE) (g. by Dushyantor (USA)): winner of a N.H. Flat Race at 5, 2008 and placed twice. 2nd dam RIGHT THEN: ran 3 times over hurdles; dam of 8 foals; 5 runners; a winner: Midsummer Glen (IRE): winner over fences; also winner of a point-to-point. Big Polly: unraced; dam of winners inc.: Stagalier (IRE): 4 wins viz. 3 wins over hurdles and placed 3 times inc. 3rd Brown Lad H. Hurdle, L. and winner over fences. Wyatt (IRE): 2 wins viz. placed; also winner over hurdles and placed 5 times and winner over fences, 2nd Naas Novice Steeplechase, Gr.3. 3rd dam ESPLANADE (by Escart III): winner at 5 and placed; also placed twice over jumps; dam of 5 foals; 5 runners; 3 winners inc.: Ballymac Lad: 4 wins viz. placed at 5; also winner of a N.H. Flat Race and placed 4 times; also 2 wins over hurdles, 2nd Celbridge Extended H. Hurdle, L. and Coral Golden EBF Stayers Ext H'cp Hurdle, L. and winner over fences.