The Cataract Blindness Challenge Innovations Case Discussion: Aravind Eye Care System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Jan Mishra - PP158" - "Incidence of Endophthalmitis After Intravitreal Injections: Risk Factors, Microbiology Profile and Clinical Outcomes from a Tertiary Centre."
8/9/2019 Newsletter Inside Editorial AWARDS AND ACCOLADES NEWS AND EVENTS The month of December was special for Aravind as three of its senior most leaders won prestigious awards at various forums. Several doctors also participated in CONFERENCES ATTENDED ELSEWHERE different conferences and brought laurels to the organization. LAICO HAPPENINGS Retreats for the staff of Glaucoma and Cataract Clinics across Aravind Eye Hospitals TRAINING PROGRAMMES were organized to come up with a roadmap and action plan to improve the services PUBLICATIONS at Aravind. Various practical aspects of patient care, research and training were discussed and debated. AUROLAB NEWS MONTHLY PATIENT STATISTICS Outreach eye camps still remain to be the mainstay of Aravind’s high-volume patient care. To a great extent this is possible because of the wholehearted support from the sponsors. To acknowledge this, every two year Aravind brings in sponsors on a Aravind News Team common platform to felicitate them and to have them share their inputs. Last month, Archives Aravind-Salem organised Sponsors Day to congratulate its camp sponsors. Hit Counter 1 News about these and many more feature in this issue. Quote Steady efforts always bring great results - the Mother AWARDS AND ACCOLADES Naanayam Vikatan’s – Business Star Award for Dr. P. Namperumalsamy Chennai, December 22, 2017 Dr. P. Namperumalsamy, Chairman Emeritus, Aravind Eye Care System was honoured with Naanayam Vikatan’s – Business Star Award under the Category - Social Consciousness at the function held Hyatt Regency, Chennai. During the function, it was highlighted that Aravind Eye Hospital provides high quality of eye care service to all the people in the community and handled over 52 million outpatients and performed 5.9 million sight-restoring surgeries in which 60 percent of them either free or highly subsidized. -

Hospital Master
S.No HOSPITALNAME STREET CITYDESC STATEDESC PINCODE 1 Highway Hospital Dev Ashish Jeen Hath Naka, Maarathon Circle Mumbai and Maharashtra 400601 Suburb 2 PADMAVATI MATERNITY AND 215/216- Oswal Oronote, 2nd Thane Maharashtra 401105 NURSING HOME 3 Jai Kamal Eye Hospital Opp Sandhu Colony G.T.Road, Chheharta, Amritsar Amritsar Punjab 143001 4 APOLLO SPECIALITY HOSPITAL Chennai By-Pass Road, Tiruchy TamilNadu 620010 5 Khanna Hospital C2/396,Janakpuri New Delhi Delhi 110058 6 B.M Gupta Nursing Home H-11-15 Arya Samaj Road,Uttam Nagar New Delhi Delhi 110059 Pvt.Ltd. 7 Divakar Global Hospital No. 220, Second Phase, J.P.Nagar, Bengaluru Karnataka 560078 8 Anmay Eye Hospital - Dr Off. C.G. Road , Nr. President Hotel,Opp. Mahalya Ahmedabad Gujarat 380009 Raminder Singh Building, Navrangpura 9 Tilak Hospital Near Ramlila Ground,Gurgaon Road,Pataudi,Gurgaon-Gurugram Haryana 122503 122503 10 GLOBAL 5 Health Care F-2, D-2, Sector9, Main Road, Vashi, Navi Mumbai Mumbai and Maharashtra 400703 Suburb 11 S B Eye Care Hospital Anmol Nagar, Old Tanda Road, Tanda By-Pass, Hoshiarpur Punjab 146001 Hoshiarpur 12 Dhir Eye Hospital Old Court Road Rajpura Punjab 140401 13 Bilal Hospital Icu Ryal Garden,A wing,Nr.Shimla Thane Maharashtra 401201 Park,Kausa,Mumbra,Thane 14 Renuka Eye Institute 25/3,Jessre road,Dakbanglow Kolkata West Bengal 700127 More,Rathala,Barsat,Kolkatta 15 Pardi Hospital Nh No-8, Killa Pardi, Opp. Renbasera HotelPardi Valsad Gujarat 396001 16 Jagat Hospital Raibaraily Road, Naka Chungi, Faizabad Faizabad Uttar Pradesh 224001 17 SANT DNYANESHWAR Sant Nagar, Plot no-1/1, Sec No-4, Moshi Pune Maharashtra 412105 HOSPITAL PRIVATE LIMITED Pradhikaran,Pune-Nashik Highway, Spine Road 18 Lotus Hospital #389/3, Prem Nagar, Mata Road-122001 Gurugram Haryana 122001 19 Samyak Hospital BM-7 East Shalimar Bagh New Delhi Delhi 110088 20 Bristlecone Hospitals Pvt. -

2012 - March 2013
1 2 One force shall be your mover and your guide, One light shall be around you and within; Hand in strong hand confront Heaven’s question, life: Challenge the ordeal of the immense disguise. Ascend from Nature to divinity’s heights; Face the high gods, crowned with felicity, Then meet a greater god, thy self beyond Time.” This word was seed of all the thing to be: A hand from some Greatness opened her heart’s locked doors And showed the work for which her strength was born. - “Savitri” by Sri Aurobindo - Book IV, Canto III 1 3 CONTENTS ACTIVITY REPORT APRIL 2012 - MARCH 2013 Highlights 1 Patient Care 7 Education and Training 21 Consultancy and Capacity Building 39 Research 49 Ophthalmic Supplies 57 Central Functions 61 Awards and Accolades 66 Partners in Service 70 Trustees and Staff 72 Photo Credits Mohan, Aravind–Tirunelveli Mike Myers, USA Iruthayaraj, Aravind–Pondicherry Rajkumar, Aravind–Madurai Sasipriya, LAICO–Madurai Senthil Kumar, Aravind–Coimbatore 2 4 6$373Y9R[3J[ All across South India every morning in front of each home, patterns are drawn on the ground with steady streams of white powder (traditionally made from rice flour) released between thumb and forefinger, weaving in continuous curving lines around a pattern of small dots.They are called Kolams and their variations are infinite and fascinating…in many ways they remind us of the beautiful patterns that emerge in our lives merely by connecting-the-dots….for in a finished kolam not a single dot is left un-embraced. Aravind has become a pattern-unto-itself and the ideas, inspirations and individuals who weave in and out of its work for sight continue to create powerful connections. -

Equitable Healthcare Access Consortium Sixth Quarterly Meeting
EQUITABLE HEALTHCARE ACCESS CONSORTIUM SIXTH QUARTERLY MEETING in collaboration with Date: 6th and 7th December 2019 Venue: Aravind Eye Hospital, Chennai VERSION 2 DATED 3 DEC 2019 Equitable Healthcare Access Consortium is grateful to Dr. Aravind S. Director – Projects, Aravind Eye Care System Chief Medical Officer, Aravind Eye Hospital, Chennai for sponsoring the 6th Quarterly Meeting and his unstinted support to making this meeting a success Our heartfelt gratitude to the entire team at Aravind Eye Hospital who has collaborated and worked hard to make this event possible THANK YOU 2 Table of Contents Practical Information .............................................................................................................. 6 Address of the Venue ............................................................................................................. 6 Distance from the Airport ...................................................................................................... 6 Contacts.................................................................................................................................. 6 The Meeting Venue................................................................................................................ 6 Catering .................................................................................................................................. 7 Lodging Arrangements .......................................................................................................... 7 Transport -
Overview of Aravind Educational Programs
There is a Power within that knows beyond Our knowings; we are greater than our thoughts, And sometimes earth unveils that vision here. To live, to love are signs of infinite things, Love is a glory from eternity’s spheres. Abased, disfigured, mocked by baser mights That steal his name and shape and ecstasy, He is still the godhead by which all can change. A mystery wakes in our inconscient stuff, A bliss is born that can remake our life. — Sri Aurobindo ‘Savitri’ Book Five, Canto Two Aravind Eye Care System Eye Care Facilities Aravind Eye Hospitals Madurai, Theni, Tirunelveli, Coimbatore & Pondicherry Lions Aravind Institute of Community Outreach Community Ophthalmology Programmes (LAICO) MISSION: To eliminate Education and Training needless blindness Aurolab Aravind Postgraduate Institute of by providing Making appropriate Ophthalmology compassionate technology affordable and high quality eye care to all Telemedicines Aravind Medical Research Foundation Rotary Aravind International Eye Bank 2 From the Director Aravind Eye Hospitals were started with a mission to eliminate needless blindness. Over the last 30 years, Aravind has contributed extensively to prevention of blindness in the country. In 2005, 1, 91,158 surgical procedures were performed. In view of the existing backlog of cataract and other causes of blindness, India requires many more institutions of this kind. Aravind Eye Hospitals has gained national and international reputation for its ser- vice orientation, modern ophthalmic techniques and its community-based outreach ac- tivities which deliver quality eye care to the rural masses. Its operational research has practical applications in the formulation of effective blindness prevention programmes. To take on the challenge of blindness, Aravind has recognised the need to develop human resource - ophthalmologists, paramedics and support service personnel. -

Do Frugal Innovations Lead to Frugal Outcomes? a Case Study of Healthcare in India
University of Pennsylvania ScholarlyCommons Wharton Research Scholars Wharton Undergraduate Research 5-2015 Do Frugal Innovations Lead to Frugal Outcomes? A Case Study of Healthcare in India Leah Davidson University of Pennsylvania Follow this and additional works at: https://repository.upenn.edu/wharton_research_scholars Part of the Business Commons Davidson, Leah, "Do Frugal Innovations Lead to Frugal Outcomes? A Case Study of Healthcare in India" (2015). Wharton Research Scholars. 127. https://repository.upenn.edu/wharton_research_scholars/127 This paper is posted at ScholarlyCommons. https://repository.upenn.edu/wharton_research_scholars/127 For more information, please contact [email protected]. Do Frugal Innovations Lead to Frugal Outcomes? A Case Study of Healthcare in India Disciplines Business This thesis or dissertation is available at ScholarlyCommons: https://repository.upenn.edu/ wharton_research_scholars/127 Do Frugal Innovations Lead to Frugal Outcomes? A Case Study of Healthcare in India By Leah Davidson Faculty Mentor: Prof. Devesh Kapur WH299: Wharton Research Scholars Thesis May 2015 In the early 1970s, Professor P.K. Sethi, an orthopedics professor in Jaipur, India, realized that the prevalent prosthesis design for lower-limb amputees was poorly suited to India’s sitting culture. He developed a waterproof, lightweight rubber-based prosthetic leg for less than 1% of the manufacturing cost in the US. The nonprofit Bhagwan Mahaveer Viklang Sahayata Samiti (BMVSS) began distributing the Jaipur Foot internationally, selling not only to amputees, but also fitting war victims and polio patients. To date, the Jaipur Foot has reached over 1.3 million people and BMVSS has held artificial limb fitment camps in 26 countries across Africa, Latin America, and Asia. -

Trichy SRM Medical College Hospital and Research Centre, Tiruchirapalli
Trichy SRM Medical College Hospital and Research Centre, Tiruchirapalli Eminent faculty and researchers had visited the institution and delivered talks on advanced topics & held discussion with faculty, scholars & students S. Name of the Affiliation Date of visit Topic discussed No. Guest 1 Dr. Padmavathy Nodal Officer, MET, Sri 10.08.2021 – Medical Education Ramachandra Medical College, 12.08.2021 Technology Chennai 2 Dr. Sowmya Nodal Officer, MET, Sri 08.04.2021 – Medical Education Ramachandra Medical College, 10.04.2021 Technology Chennai 3 Dr. Mohan Associate Dean of Primary 21.01.2020 Exploring global medical Kumar Medical Care Education, Wigan education and Preston 4 Dr. Guru T. Specialist Physician, Hamad 21.01.2020 Exploring global medical Arun Medical Corporation, Qatar and education Consultant Radiologist, Qutar 5 Dr. J. Yuvaraj Scientist G, National Institute of 21.01.2020 Exploring global medical Epidemiology, ICMR, Chennai education 6 Mr. P. Prabahar Regional Transport Officer, 24.01.2020 Road Safety Srirangam, Trichy 7 Dr. Guru T. Specialist Physician, Hamad 20.01.2020 Emotional Intelligence Arun Medical Corporation, Qatar and Consultant Radiologist, Qutar 8 Dr. Christhu Raj Assistant Professor, SRM Centre 07.01.2020 E-lab, E-circuit, E-skill, for Applied Research in E-lock and E-verify Education 9 Prof. Rajeev Senior Advisor and Head, SRM 07.01.2020 E-lab, E-circuit, E-skill, Sukumaran Centre for Applied Research in E-lock and E-verify Education 10 Dr. R. Professor of Statistics, 19.12.2019 Statistics Muthukrishnan Bharathiar University, Coimbatore 11 Dr. Sitanshu Addl. Professor of Preventive 20.12.2019 Sampling techniques Sekhar Kar and Social Medicine, Jawaharlal Institute of Postgraduate Medical Education and Research (JIPMER), Puducherry 12 Dr. -

(CSR) Policy Strives to Transform India Into a Risk-Aware Society from Being a Risk-Averse Society
Our Corporate Social Responsibility (CSR) policy strives to transform India into a risk-aware society from being a risk-averse society. We aim to integrate social, environmental and health concerns of the Indian society into Corporation’s CSR policy and programmes. Our CSR activities have focused on capacity building, empowerment of communities, inclusive socio-economic growth, environment protection, promotion of green and energy efficient technologies, development of backward regions, and uplifting the marginalized and under- privileged sections of the society. Nowadays CSR goes beyond charity and requires the company to act beyond its legal obligations. It rests on the ideology of give and take. Companies take resources in the form of raw materials, human resources etc. from the society. By performing the task of CSR activities, the companies are giving something back to the society. In the changing business environment, doing well (profit) and doing good (caring) are not mutually exclusive but mutually reinforcing. There has been a paradigm shift from the way business was done earlier to how it should be done today. It's no longer a question if companies should engage in CSR, it’s now a question of to what extent will they do so, and how they will create and communicate real and meaningful impact. REPORT ON CSR ACTIVITIES IN FY 2019-20 1. Aravind Eye Hospitals – The Govel Trust. a non-profit organization is running the Aravind Eye Hospitals at Madurai, Theni, Tirunelveli, Coimbatore, Coimbatore City centre, Pondicherry, Tuticorin, Tirupur, Udumalpet, Dindigul, Salem, Chennai and Tirupati. It was founded in 1976 by Dr. G. -
CSBL Unpaid Dividend, Refund Consolidated As on 22.09.2015.Xlsx
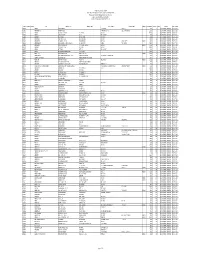
The Catholic Syrian Bank Limited Regd. Office, "CSB Bhavan", St. Mary's College Road, Thrissur 680020 Phone: 0487 -2333020, 6451640, eMail: [email protected] List of Unpaid Dividend as on 22.09.2015 (Dividend for the periods 2007-08 to 2013-14) FOLIO / DEMAT ID INITLS NAME ADDRESS LINE 1 ADDRESS LINE 2 ADDRESS LINE 3 ADDRESS LINE 4 PINCOD DIV.AMOUNT DWNO MICR PERIOD IEPF. TR. DATE A00350 ANTONY PALLANS HOUSE KURIACHARA TRICHUR, 30.00 0 2007-08 UNPAID DIVIDEND 25-OCT-2015 A00385 ANNAMMA P X AKKARA HOUSE PANAMKUTTICHIRA OLLUR, TRICHUR DIST 150.00 5 2007-08 UNPAID DIVIDEND 25-OCT-2015 A00398 ANTONY KUTTENCHERY HOUSE HIGH ROAD TRICHUR 1020.00 0 2007-08 UNPAID DIVIDEND 25-OCT-2015 A00406 ANTONY KALLIATH HOUSE OLLUR TRICHUR DIST 27.00 9 2007-08 UNPAID DIVIDEND 25-OCT-2015 A00409 ANTHONY PLOT NO 143 NEHRU NAGAR TRICHUR-6 120.00 0 2007-08 UNPAID DIVIDEND 25-OCT-2015 A00643 ANTHAPPAN PADIKKALA HOUSE EAST FORT GATE TRICHUR 540.00 12 2007-08 UNPAID DIVIDEND 25-OCT-2015 A00647 ANTHONY O K OLAKKENGAL HOUSE LOURDEPURAM TRICHUR - KERALA STATE. 680005 180.00 13 2007-08 UNPAID DIVIDEND 25-OCT-2015 A00668 ANTHONISWAMI C/O INASIMUTHU MUDALIAR SONS 55 NEW STREET KARUR TAMILNADU 2100.00 14 2007-08 UNPAID DIVIDEND 25-OCT-2015 A00822 ANNA JACOB C/O J S MANAVALAN 5 V R NAGAR ADAYAR MADRAS - 600020 210.00 18 2007-08 UNPAID DIVIDEND 25-OCT-2015 A01072 ANTHONY VI/62 PALACE VIEW EAST FORT TRICHUR 4200.00 0 2007-08 UNPAID DIVIDEND 25-OCT-2015 A01077 ANTONY KOTTEKAD KUTTUR TRICHUR DIST 30.00 0 2007-08 UNPAID DIVIDEND 25-OCT-2015 A01103 ANTONY ELUVATHINGAL CHERUVATHERI -

Patron-In-Chief Honorary Fellows Founder Fellows
Patron-in-Chief 1. Dr. Rajendra Prasad 2. Dr. S. Radhakrishnan 3. Dr. Zakir Husain 4. Shri V.V. Giri 5. Shri Fakhruddin Ali Ahmed 6. Shri Giani Zail Singh Honorary Fellows 1. Shri Jawahar Lal Nehru 2. Dr. B.C. Roy 3. Major Genl. S.L. Bhatia 4. Col. R.N. Chopra 5. Dr. H.M. Lazarus 6. Dr. Jivaraj N. Mehta 7. Dr. A. Lakshamanswami Mudaliar 8. Dr. N.A. Purandare 9. Major Genl. S.S. Sokey 10. Dr. A.C. Ukil 11. Dr. Sushila Nayar 12. Smt. Indira Gandhi 13. Dr. V.T.H. Gunaratne 14. Dr. Dharmendra 15. Shri P.V. Narasimha Rao Founder Fellows 1. Dr. Madan Lal Aggarwal 2. Dr. B.K. Aikat 3. Dr. S.T. Achar 4. Dr. (Col.) Amir Chand 5. Dr. A.A. Ayer 6. Dr. Santokh Singh Anand 7. Dr. R.B. Arora 8. Dr. L.H. Athle 9. Dr. A.V. Baliga 10. Dr. Baldev Singh 11. Dr. Bankat Chandra 12. Dr. A.K. Basu 13. Dr. B.B. Bhatia 14. Dr. T.N. Banerjee 15. Dr. Bimal Chandra Bose 16. Dr. J.C. Banerjee 17. Dr. E.J. Borges 18. Dr. P.V. Cherian 19. Dr. R.N. Chaudhuri 20. Dr. G. Coelho 21. Dr. R.A.F. Cooper 22. Dr. (Lt.Genl.) D.N. Chakravarti 23. Dr. L.W. Chacko 24. Dr. M.K.K. Menon 25. Dr. Subodh Mitra 26. Dr. (Capt) P.B. Mukherjee 27. Dr. S.R. Mukherjee 28. Dr. B. Mukhopadhaya 29. Dr. M. Naidu 30. Dr. B. Narayana 31. Dr. C.G. -

2017 RESEARCH Secondary Eye Care Centres - 6 Aravind Medical Research Foundation (Cataract Services, Speciality Diagnosis) Dr
1 DR. G. VENKATASWAMY 1918 - 2006 The genius of the man was in using an adjective,‘needless’ to give a context to the scourge of blindness. It gave energy, hope and inspiration to scores of ophthalmologists to combat it. And for that and much more, we celebrate his life. Dr. G. Venkataswamy, Aravind’s Founder Chairman was born on October 1,1918 . The year 2018 marks his birth centenary. As we take stock of the achievements Aravind has made in the last year, we reminisce the great visionary’s life - how from simple beginnings, he developed Aravind into a sophisticated system dedicated to compassionate service. Several of Dr. V’s photographs are interspersed throughout this report to remind and inspire all those who have dedicated their lives to his mission of eliminating needless blindness. 2 What now we see is a shadow of what must come. The earth’s uplook to a remote Unknown Is a preface only of the epic climb `.%I:JQ%C``QI1 : V:` .C7 : V To the discovery of a greater self And the far gleam of an eternal Light. This world is a beginning and a base Where Life and Mind erect their structured dreams; An unborn Power must build reality. RV: .GQ%JRC1CVJV1JQ :CC1V:`V7 IIQ` :CQ%``Q`$QVJ0: JVV Await discovery in our summit selves; Unmeasured breadths and depths of being are ours. - Sri Aurobindo, from Savitri, Book I, Canto IV 3 CONTENTS Highlights 8 Patient Care 14 - Eye Hospitals - Vision Centres - Community Outreach - Aravind Integrated Eye Bank Services Education and Training 32 Consultancy and Capacity Building 56 Research 62 Manufacturing -

India Abroad Person of the Year Awards Honor the Community's Star Achievers
ADVERTISEMENT PERIODICAL Friday, March 19, 2010 Vol. XL No.25 www.rediff.com (Nasdaq: REDF) $1 International Weekly Newspaper Chicago/Dallas Los Angeles NY/NJ/CT New York Toronto PERIODICAL INDEX Letters to the Editor..........................................A2 People...................................................................A4 Immigration.....................................................A30 Business............................................................A24 Community.......................................................A34 Magazine..........................................................M1 Sports................................................................A32 Pages: 52+24=76 Friday, March 19, 2010 Vol. XL No.25 www.rediff.com (Nasdaq: REDF) NEW YORK EDITION $1 International Weekly Newspaper Chicago/Dallas Los Angeles NY/NJ/CT New York Toronto Winners All SUMAN GUHA MOZUMDER The India Abroad Person of the Year awards honor the community's star achievers To subscribe 1-8877-IINDIA-AABROAD (1-877-463-4222) www.indiaabroad.com/subscribe ADVERTISEMENT The International Weekly Newspaper founded in 1970. Member, Audit Bureau of Circulation A225 India Abroad March 19, 2010 INDIA ABROAD (ISSN 0046 8932) is published every Friday by India Abroad LETTERS Publications, Inc. 42 Broadway, 18th floor, New York, NY 10004. Annual subscription in United States: $32. Canada $26. India $32 INTERNATIONAL: By Regular Mail: South America, the Caribbean, Europe, Africa, Australia & Middle East: $90. By Airmail: South America, the Caribbean,