James Cook University Murtupuni Centre for Rural and Remote Health 2020 Annual Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cairns to Undara Road Trip
Cairns to Estimated Days 3 Stop Overs 2 Undara Road Trip Via Mareeba and Chillagoe ANCIENT GEOLOGICAL WONDERS EXPERIENCE HIGHLIGHTS DAY ONE DAY THREE Port Douglas Mareeba Heritage Centre Bush Breakfast Camp 64 Dimbulah Archway Explorer Tour CAIRNS Mareeba Chillage-Mungana National Park Pinnarendi Station Café Chillagoe Royal Arch Cave Tour (1.30pm) Innot Hot Springs Atherton Karumba Ancient Aboriginal Rock Art Ravenshoe Bakery Innisfail Accomm: Chillagoe Cabins Cairns Ravenshoe Burketown Normanton Mount Garnet Mount Surprise Doomadgee Croydon Undara DAY TWO Georgetown Experience Sunrise at the Smelters Boodjamulla Einasleigh National Park Cobbold Gorge Donna Cave Tour (9am) Forsayth Swim at Chillagoe Weir Railway Hotel Almaden Australia’s AccessibleBurke and Wills Outback Undara Experience Roadhouse TOWNSVILLE Wildlife at Sunset Tour This three-day journey will take you to some of Australia’s most Accomm: Undara Experience incredible geological wonders from the outback town of Chillagoe to the incredible Undara Volcanic National Park. Charters Towers Julia Creek Hughenden Mt Isa Cloncurry For more information phone (07) 4097 1900 or visit www.undara.com.au Cairns to Undara Roadtrip DAY 1 Cairns to Chillagoe Via Mareeba & the Wheelbarrow Way Highlights: Local Coffee, Country Lunch, Cave Tour & Cultural History Set off early on your journey to Chillagoe-Mungana National Park, 215km or three hours drive west of Cairns, starting point of the Savannah Way, incorporating the Wheelbarrow Way. Once an ancient coral reef, this park on the edge of the outback is rich in natural and cultural heritage. It features spectacular limestone caves, small galleries of Aboriginal rock art, jagged limestone outcrops and an historically significant mining site. -

Tropical North Queensland Tourism Opportunity Plan
Tropical North Queensland Tourism Opportunity Plan 2 0 1 0 - 2 0 2 0 DISCLAIMER – Tourism Tropical North Queensland and Tourism Queensland makes no claim as to the accuracy of the information contained in the Tropical North Queensland Tourism Opportunity Plan. The document is not a prospectus and the information provided is general in nature. The document should not be relied upon as the basis for financial and investment related decision. DISCLAIMER – STATE GOVERNMENT The Queensland Government makes no claim as to the accuracy of the information contained in the Tropical North Queensland Tourism Opportunity Plan. The document is not a prospectus and the information provided is general in nature. The document should not be relied upon as the basis for financial and investment related decisions. This document does not suggest or imply that the Queensland State Government or any other government, agency, organisation or person should be responsible for funding any projects or initiatives identified in this document. Executive Summary Dunk Island Purpose Catalyst Projects The purpose of this Tourism Opportunity Plan (TOP) is to Through the consultation and review process the following provide direction for the sustainable development of tourism in 18 catalyst projects have been identified for the Tropical North the Tropical North Queensland region. Queensland region. These projects are tourism investment or infrastructure projects of regional significance which are The TOP aims to: expected to act as a catalyst to a range of other investment, marketing and product development opportunities. < Identify new and upgraded tourism product that meets future visitor expectations and demands; 1 . Cairns Arts, Cultural and Events Precinct < Identify the need for new investment in infrastructure that 2 . -

Final Milestone Report on the Gulf Reconnaissance Component
Report to Land & Water Australia Ecosystem processes in tropical rivers: conceptual models and future research. Final milestone report on the gulf reconnaissance component August 2005 Prepared by: DR ANDREW BROOKS Centre for Riverine Landscapes, Griffith University Email: [email protected] Project Reference: GRU34 ABSTRACT As part of the developmental phase of the Tropical Rivers and Coastal Knowledge (TRaCK) Program this project was instigated to undertake a reconnaissance of all rivers draining into the Gulf of Carpentaria, as well as collecting baseline data and undertaking regional stakeholder consultation. The primary field component of this project was undertaken during September and October 2004, during which time an aerial reconnaissance was completed along the trunk streams of all major rivers draining into the Gulf of Carpentaria. Global Positioning System (GPS) located videography was successfully trialled in this reconnaissance using a non gyro-stabilised mounting from a twin engine, fixed wing platform. Using this approach, high-resolution imagery (1 – 2m) of the channel and riparian zone was collected along 13500km of river channel over 43 hours of flying time. The imagery collected equates to around 52% of the channel network defined by the 1:5M topographic network, which is the network being used to define the streams being classified in an affiliated project. At around $5.50 per river kilometre, this approach has proved to be an efficient and cost effective method of undertaking reconnaissance of large remote area river systems, which at the same time provides a high quality permanent record of the river channel that can effectively form the baseline inventory for subsequent research. -

The Land Tribunals
Torres Strait Thursday Island Cape York Weipa Coen GREAT GULF OF CARPENTARIA Cooktown Mornington Island REPORTS ON Cairns Burketown Normanton THE OPERATIONS OF CORAL SEA Croydon Georgetown BARRIER Ingham Townsville THE LAND TRIBUNALS SOUTH PACIFIC OCEAN Charters Towers Bowen Proserpine REEF Mount Isa Julia Creek Cloncurry Richmond Hughenden Mackay ESTABLISHED UNDER Winton St Lawrence NORTHERN TERRITORY Boulia THE ABORIGINAL LAND ACTCapella 1991 AND Longreach Barcaldine Emerald Rockhampton Jericho Blackwater THE TORRES STRAIT ISLANDER LAND ACT 1991 Blackall Springsure FOR THE YEAR ENDED 30 JUNE 2010 Bundaberg Eidsvold Maryborough Windorah Taroom Birdsville Gayndah Gympie Charleville Roma Miles Quilpie Mitchell Sunshine Coast Surat Dalby Ipswich BRISBANE Gold Cunnamulla SOUTH AUSTRALIA Thargomindah Coast St George Warwick Goondiwindi Stanthorpe NEW SOUTH WALES REPORT ON THE OPERATIONS OF THE LAND TRIBUNAL ESTABLISHED UNDER THE ABORIGINAL LAND ACT 1991 FOR THE YEAR ENDED 30 JUNE 2010 Table of Contents Report of the Land Tribunal established under the Aboriginal Land Act 1991 Paragraph I INTRODUCTION 1 - 2 II THE LAND TRIBUNAL 3 (a) Membership 4 - 9 (b) Functions 10 - 12 (c) Land claim procedures 13 - 14 III LAND CLAIMS (a) Claimable land and land claims 15 - 17 (b) Tribunal Proceedings 18 - 20 (c) Land claim reports 21 (d) Sale of land claim reports 22 - 23 (e) Status of claims determined by the Land Tribunal 24 - 25 (f) Status of all land claims 26 IV LEGISLATION 27 - 28 V ADMINISTRATIVE MATTERS (a) Staff 29 (b) Relationship with the Land Court and 30 other Tribunals (c) Administrative arrangements 31 - 32 (d) Budget 33 - 35 (e) Accommodation 36 VI CONCLUDING REMARKS 37 Claimant and locality identification Annexure A Advertising venues, parties and hearing dates Annexure B REPORT ON THE OPERATIONS OF THE LAND TRIBUNAL ESTABLISHED UNDER THE ABORIGINAL LAND ACT 1991 FOR THE YEAR ENDED 30 JUNE 2010 I INTRODUCTION 1. -

Socio-Economic Overivew of the Northern Marine Planning Area
Socio-Economic Overview of the Northern Planning Area June 2004 ii iii Contents List of tables iv List of figures viii Summary 1 Introduction 3 Method 4 1 The demographics of the Northern Planning Area 11 population 2 The cultural characteristics of the Northern 17 Planning Area 3 Other social characteristics of the Northern 25 Planning Area 4 The economic characteristics of the Northern 33 Planning Area Conclusion 41 Note on the quality of Indigenous data 49 References 51 Appendix – Results for defining the sub-regions 52 Appendix – Detailed tables 57 Glossary 122 iv List of tables Results for defining the sub-regions 1 Statistical Local Areas and sub-regions by total persons counted, 6 Northern Planning Area, 2001 2 Sub-regions defined by Collection Districts with corresponding 52 Indigenous Locations and Localities, 2001 Demographic tables 3 Estimated Resident Population (ERP) of Statistical Local Areas 58 in the Northern Planning Area, 1998, 2002 and 2003 4 Population by sub-region, Northern Planning Area, 2001 59 5 Number of persons by address 1 year and 5 years before 2001 60 Census by sub-region, Northern Planning Area, 2001 6 Persons by address 1 year and 5 years before 2001 Census by 61 sub-region, Northern Planning Area, 2001 (percentage of total sub-region population) 7 Population by sex by sub-region, Northern Planning Area, 2001 62 8 Population by sex by sub-region, Northern Planning Area, 2001 63 (percentage of the total sub-region population) 9 Population by sex by sub-region, Northern Planning Area, 2001 64 (percentage -
Register of Burials As at 6 December 2019
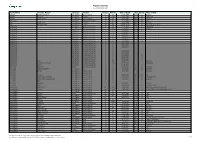
Register of Burials as at 6 December 2019 Family Name Christian Names Cemetery Division Section Plot No Date of Death Age Gender Place of Birth ABBOTT BEATRICE MARY M New Ingham Roman Catholic 36 56 16/02/1989 75 F ST KILDA ABBOTT CHARLES Old Ingham Anglican 0 1,294 12/05/1939 0 M UNKNOWN ABBOTT HENRY TERRY New Ingham Roman Catholic 36 55 8/04/1997 85 M INGHAM ABDOOLAH Old Ingham Mixed Denomination 0 52 12/11/1903 55 M INDIA ABEL ISABEL JANE New Ingham Anglican 17 921 24/06/2008 84 F INGHAM ABEL ROY OSBOURNE New Ingham Anglican 17 922 20/02/2016 88 M Townsville, Queensland ABORIGINAL Old Ingham Mixed Denomination 0 122 17/12/1911 0 F UNKNOWN ABORIGINAL Old Ingham Mixed Denomination 0 529 8/04/1925 0 F INGHAM ABORIGINAL Old Ingham Mixed Denomination 0 0 16/05/1916 0 F ABORIGINAL Old Ingham Mixed Denomination 0 0 26/06/1916 0 M ABORIGINAL Old Ingham Mixed Denomination 0 0 10/03/1917 0 F ABORIGINAL Old Ingham Mixed Denomination 0 0 29/04/1917 0 F ABORIGINAL Old Ingham Mixed Denomination 0 0 28/10/1917 0 M ABORIGINAL Old Ingham Mixed Denomination 0 0 19/07/1919 0 M ABORIGINAL Old Ingham Mixed Denomination 0 0 22/07/1919 0 M ABORIGINAL Old Ingham Mixed Denomination 0 0 30/07/1919 0 ABORIGINAL Old Ingham Mixed Denomination 0 0 4/08/1919 0 ABORIGINAL Old Ingham Mixed Denomination 0 0 0 ABORIGINAL Old Ingham Mixed Denomination 0 0 20/12/1922 0 F ABORIGINAL Old Ingham Mixed Denomination 0 0 25/07/1923 0 F ABORIGINAL Old Ingham Mixed Denomination 0 0 20/11/1923 0 M ABORIGINAL Old Ingham Mixed Denomination 0 0 29/01/1924 0 M ABORIGINAL Old Ingham Mixed Denomination 0 0 12/04/1924 0 M ABORIGINAL BABY Old Ingham Mixed Denomination 0 529 8/04/1925 0 F INGHAM ABORIGINAL No Record - Unknown Old Ingham Mixed Denomination 0 166 24/09/1913 0 UNKNOWN ABORIGINAL ROSIE Old Ingham Mixed Denomination 0 0 14/08/1924 0 F ABRAHAM RICHARD Halifax Mixed Denomination 45 11 10/11/1921 56 M ENGLAND ABRAHAM STANLEY EMMETT New Ingham R.S.L. -

6 Days Savannah Way, Queensland
ITINERARY Savannah Way, Queensland Queensland – Cairns Cairns – Ravenshoe – Georgetown – Normanton – Katherine AT A GLANCE Drive from Cairns, through Queensland’s yourself in the caves of Undara Volcanic lush Tropical Tablelands and historic National Park, the world’s longest lava > Cairns to Atherton (1.5 hours) goldfields, and across the Northern Territory system. Fossick for gold in historic Croydon > Atherton to Georgetown (4 hours) border to Katherine. Walk through World and Georgetown and spot crocodiles in the Heritage-listed rainforest in Kuranda and wetlands around Normantown. Discover > Georgetown to Normanton (5 hours) explore the produce-rich countryside hidden gorges and Aboriginal rock art in > Normanton to Burketown (3 hours) around Mareeba. Visit a century-old Boodjamulla National Park before crossing Chinese temple in Atherton and spend the Central Gulf into the Northern Territory. > Burketown to Borroloola (7 hours) the night in Ravenshoe, Queensland’s From here, the Savannah Way continues > Borroloola to Katherine (9 hours) highest town. Marvel at Millstream Falls, across the outback all the way to Western Australia’s widest waterfalls and lose Australia’s pearling town of Broome. DAY ONE CAIRNS TO ATHERTON Bushwalk and spot rare native birds in wildlife-rich Tolga Scrub into Atherton, in the Mareeba Wetlands and explore the the heart of the scenic Tropical Tablelands. Drive out of tropical Cairns, on the doorstep volcanic rock formations of Granite Gorge. Walk through rainforest and past miniature of north Queensland’s islands, rainforest See Aboriginal rock art galleries in Davies waterfalls for a top-of-the-tablelands view and reef. Bushwalk, visit Barron Falls and Creek National Park or picnic next to the from Halloran’s Hill. -

Allan Rintoul
Productivity Commission Submission - Remote Area Tax Concessions and Payments Submission to: Remote Area Tax Concessions and Payments Review 29 April 2019 Author: Allan Geoffrey Rintoul For over seven years now I have been living in the more remote areas of northern and north western Queensland. These areas include Bamaga, Julia Creek, Aramac, Longreach and now Burketown. Whilst living in these areas can be considered as a “choice”, it has been for work and to assist in still maintaining a family, mortgage and all those other necessities of life. I do believe there needs to be a realistic recognition that living in the more remote areas of the country does require a serious review of its cost not only for those of us presently living in the areas, but to also promote others to move and live in the regions. Assistance with either in the up front costs impacts or as this study drives - at the end or the tax year, will be most beneficial in assisting remote communities, families and workers. In making a submission to the Remote Area Tax Concessions and Payments, I offer the following details regarding the issues associated with the cost of living and living in general in these communities. 1. Distance to major centres – the travel distance to major centres (Cloncurry and Mount Isa) from Burketown is 4.5-6.5 hours dependant of the desire to travel of at best very rough gravel road. Many of which are unfenced and subject to wildlife and live stock as an ongoing hazard. The key issue of these communities is the isolation in the wet season where one can be cut off by road for extended periods. -

North West District April 2016
9 Legend 0 D AURUKUN ABORIGINAL Do Not Cross Structures SHIRE COUNCIL Coen ! Structure Id Rd Number Bridge Structure Id [" 9 Culvert 0 Rd Number C State-controlled road Local Government boundary COOK SHIRE PORMPURAAW COUNCIL PDO District boundary ABORIGINAL SHIRE COUNCIL Pormpuraaw CARPENTARIA HOPE VALE SHIRE ! ABORIGINAL COUNCIL KOWANYAMA SHIRE COUNCIL ABORIGINAL SHIRE COUNCIL Hope Vale Kowanyama 90C Cooktown ³ Laura ! C 050100150 34 90 Km B WUJAL WUJAL ABORIGINAL SHIRE COUNCIL Wujal Wujal B 4 3 DOUGLAS 89B SHIRE COUNCIL 6 5 5 Mossman Craiglie[" 3 3 5 Gununa 4 6 B CARPENTARIA SHIRE Kuranda COUNCIL 34 A A 2 3 MAREEBA Mareeba 8 SHIRE COUNCIL B 2 664 3 DOOMADGEE Dimbulah Tinaroo 6 ABORIGINAL FAR Chilagoe Tolga 89B B SHIRE COUNCIL 9 8 Atherton NORTH 89B 66 3 3 ! 84A 2 Herberton 6 6 6 4 ! 1 ! 7734 ! Karumba Rd 89B Millaa Millaa B 9 Normanton 8 Ravenshoe ! Burketown Mount Garnet" ! D [ 32 92A A 9 Doomadgee 8 BURKE TABLELANDS SHIRE REGIONAL COUNCIL COUNCIL 7 Croydon 8 A C 92 92B ! ! Georgetown 4 0 7 6 CROYDON SHIRE COUNCIL ETHERIDGE 1 SHIRE 0 8 6 COUNCIL A 9 98D 9 A 9 8 98C 7 8A " Burke and Wills Junction ! 7687 1 680 B 9 9 MOUNT 8 9 15C ISA CITY A ! NORTH Camooweal COUNCIL [" 15660 NORTHERN 15633 WEST 1 [" CHARTERS TOWERS 5 B 7732 REGIONAL ! COUNCIL 78 A 7731 RICHMOND N ! SHIRE O 14E Julia Creek COUNCIL R [" 14D B CLONCURRY 9 9 T MOUNT ISA [" 14E 14387 14E [" Richmond H [" 15A 43159 13424 E F 15059 3 9 Hughenden R Rd 14E B 1 14 14 3 C N H MCKINLAY [" SHIRE 13304 T 5 COUNCIL 8 0 E [" 7 3 0 43023 8 R 5 9C " R 9 [ 25978 FLINDERS I 08 T 77 [" 37537 SHIRE O COUNCIL R CLONCURRY 3 Y SHIRE 0 7 1 5 COUNCIL 3H 13G 1 " 0 [ ! 25241 7 Kynuna 5 93F [" 10591 ! Dajarra 1 C 3 9 G 9 9 3 E 99D Winton 13F BOULIA SHIRE WINTON SHIRE 05 COUNCIL 57 COUNCIL 5 72 CENTRAL WEST [" Boulia 99D BARCALDINE REGIONAL COUNCIL Aramac [" Longreach LONGREACH BARCALDINE * Notes: REGIONAL DIAMANTINA COUNCIL SHIRE 1. -
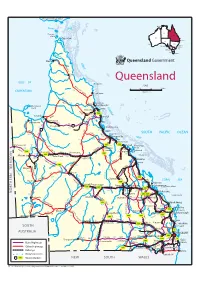
Queensland-Map.Pdf
PAPUA NEW GUINEA Darwin . NT Thursday Island QLD Cape York WA SA . Brisbane Perth . NSW . Sydney Adelaide . VIC Canberra . ACT Melbourne TAS . Hobart Weipa PENINSULA Coen Queensland Lizard Is DEVELOPM SCALE 0 10 20 300km 730 ENT Kilometres AL Cooktown DEV 705 ROAD Mossman Port Douglas Mornington 76 Island 64 Mareeba Cairns ROAD Atherton A 1 88 Karumba HWY Innisfail BURKE DY 116 Normanton NE Burketown GULF Tully DEV RD KEN RD Croydon 1 194 450 Hinchinbrook Is WILLS 1 262 RD Ingham GREGOR 262 BRUCE Magnetic Is DEV Y Townsville DEV 347 352 Ayr Home Hill DE A 1 Camooweal BURKE A 6 130 Bowen Whitsunday 233 Y 188 A Charters HWY Group BARKL 180 RD HIGHW Towers RD Airlie Beach Y A 2 Proserpine Y Cloncurry FLINDERS Richmond 246 A 7 396 R 117 A 6 DEV Brampton Is Mount Isa Julia Creek 256 O HWY Hughenden DEV T LANDSB Mackay I 348 BOWEN R OROUGH HWY Sarina R A 2 215 DIAMANTINA KENNEDY E Dajarra ROAD DOWNS T 481 RD 294 Winton DEV PEAK N 354 174 GREG A 1 R HIGHW Clermont BRUCE E KENNEDY Boulia OR 336 A A 7 H Y Y Yeppoon DEV T Longreach Barcaldine Emerald Blackwater RockhamptonHeron Island R A 2 CAPRICORN A 4 HWY HWY 106 A 4 O RD 306 266 Gladstone N Springsure A 5 A 3 HWY 389 Lady Elliot Is LANDSBOR HWY DAWS Bedourie Blackall ON Biloela 310 Rolleston Moura BURNETT DIAMANTINA OUGH RD A 2 C 352 Bundaberg A 404 R N Theodore 385 DEV A Hervey Bay R 326 Eidsvold A 1 V LEICHHARDT Fraser Is D O Windorah E Taroom N 385 V BRUCE EYRE E Augathella Maryborough L Gayndah RD HWY A 3 O DEV A 7 A 5 HWY Birdsville BIRDSVILLE 241 P M HWY A 2 E N W T ARREGO AL Gympie Quilpie -

Map of Local Government Areas in Queensland
Department of Local Government, Racing and Multicultural Affairs CHERBOURG ! Gympie ABORIGINAL ! SHIRE GYMPIE TORRES STRAIT Cherbourg REGIONAL NOOSA SHIRE ISLAND REGIONAL TORRES ! Tewantin Thursday SHIRE Island ! SOUTH Bamaga BURNETT ! REGIONAL NORTHERN PENINSULA SUNSHINE AREA REGIONAL ! COAST Maroochydore REGIONAL MAPOON ABORIGINAL SHIRE ! Caloundra Mapoon ! WEIPA TOWN AUTHORITY Lockhart SOMERSET River REGIONAL ! MORETON! Caboolture NAPRANUM LOCKHART RIVER BAY ABORIGINAL SHIRE BRISBANE ABORIGINAL REGIONAL CITY SHIRE Aurukun ! ! ! Esk Redcliffe AURUKUN SHIRE COOK SHIRE TOOWOOMBA REGIONAL PORMPURAAW ABORIGINAL ! Brisbane REDLAND CITY SHIRE HOPE VALE ! Cleveland ABORIGINAL ! Toowoomba ! Gatton Pormpuraaw ! SHIRE ! Ipswich ! LOCKYER Logan KOWANYAMA WUJAL WUJAL ABORIGINAL Hope Vale VALLEY IPSWICH CITY ! ABORIGINAL SHIRE SHIRE Kowanyama REGIONAL ! Cooktown ! LOGAN CITY Wujal Wujal! GOLD COAST CITY ! Southport DOUGLAS SHIRE ! Beaudesert Port Douglas ! YARRABAH SCENIC RIM SOUTHERN REGIONAL Gununa ! ABORIGINAL DOWNS Cairns SHIRE CARPENTARIA !! REGIONAL MAREEBA Mareeba ! ! Coolangatta MORNINGTON SHIRE SHIRE Yarrabah SHIRE ! Warwick Atherton ! CAIRNS REGIONAL DOOMADGEE ABORIGINAL Normanton ! SHIRE ! Burketown Doomadgee ! Tully ! CASSOWARY COAST CROYDON TABLELANDS ! Croydon Georgetown REGIONAL BURKE SHIRE ! REGIONAL SHIRE ETHERIDGE Ingham ! Palm Island SHIRE ! HINCHINBROOK PALM ISLAND SHIRE ABORIGINAL SHIRE TOWNSVILLE CITY Townsville ! BURDEKIN ! Ayr SHIRE Charters MOUNT CHARTERS Towers ISA CITY ! RICHMOND TOWERS MCKINLAY SHIRE REGIONAL Proserpine -

CASE STUDY Burketown Boat Ramp
CASE STUDY Burketown Boat Ramp Burketown | Queensland BACKGROUND The Burketown Council approached Green Frog Systems to design a solar lighting and energy storage solution for the Burketown Shire Boat Ramp car park. Burketown is located in the far north-western Shire of Burke, Queensland and is 898km west of Cairns on the Albert River and Savannah Way in the area known as the Gulf Savannah. The Burke Shire’s remoteness is also an advantage, with world class Barramundi fishing, an abundance of bird life and well fed crocodiles. The local boat ramp is popular with locals and tourists a like seeking to take to the water and enjoy this popular boating and fishing destination. OUR SOLUTION The solution for the client was a six (6) cyclone rated solar powered street lighting towers fitted with high capacity solar panel arrangements and extended battery storage. Each tower has a twin 300W panel configuration and a 40W CREE LED lighting fixture delivering 7,560lm of light output. The upgraded solar panels enabled the lighting towers to harvest enough solar energy to power a specialised CCTV camera system with a live feed microwave transmission feed back to council headquarters. This system has to be 100% off grid and vandal resistant with virtually no maintenance required for operation. it also needed to endure the waterfront environment and the Queensland tropics. RESULTS The Burketwon Shire Council was extremely pleased with the outcome of this project. The improvements to the wharf and boat ramp were complimented by the addition of lighting which has increased the utilisation of this community asset after dark.