Covid 19 Coastal Plan- Trivandrum
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Accused Persons Arrested in Thiruvananthapuram Rural District from 11.12.2016 to 17.12.2016
Accused Persons arrested in Thiruvananthapuram Rural district from 11.12.2016 to 17.12.2016 Name of the Name of Name of the Place at Date & Court at Sl. Name of the Age & Cr. No & Sec Police Arresting father of Address of Accused which Time of which No. Accused Sex of Law Station Officer, Rank Accused Arrested Arrest accused & Designation produced 1 2 3 4 5 6 7 8 9 10 11 Thodiyil veedu, Kurup 2598/16 U/S Lane, Velloorkonam, 11.12.16, V S Prasanth, SI JFMC 1 , 1 Suresh Velappan M, 49 Katcheri Jn U/s 279 IPC & Attingal Chittattinkara, 12.40 hrs of police Attingal 185 of MV Act Attingal Nandanam veedu, Vavaravila veedu, 2599/16 U/S 11.12.16, Gopalakrishna JFMC 1 , 2 Sajith Satheesan M, 24 Kaduvayil, Velarkudi U/s 279 IPC & Attingal 16.07 hrs kurup, GSI Attingal Chittattinkara, 185 of MV Act Attingal Kaduvayil veedu, Kadambattu, 2600/16 U/S 11.12.16, Gopalakrishna JFMC 1 , 3 Sajeev Chandran M, 35 Ramachamvila, Katcheri Jn U/s 279 IPC & Attingal 19.51 hrs kurup, GSI Attingal Chittattinkara, 185 of MV Act Attingal Puthanvila veedu, 2602/16 U/S 11.12.6, V S Prasanth, SI JFMC 1 , 4 Rijin Maheendran M, 27 Keezhattingal Desom, Katcheri Jn U/s 279 IPC & Attingal 21.50 hrs of police Attingal Keezhattingal Village 185 of MV Act Renju 2603/16 U/S Bhuvanachan Balakrishna Near KSRTC 11.12.16, V S Prasanth, SI JFMC 1 , 5 M, 60 Bhavan,Aliyadu,Manik U/s 279 IPC & Attingal dran Nair Pillai Stand 21.52 hrs of police Attingal kal, Koliyakode 185 of MV Act Thenguvila veedu, H& Shaji Muhammad 11.12.16, 2604/16 U/S V S Prasanth, SI JFMC 1 , 6 M,47 C Compound, -

49Th Week (1St December to 7Th December) 2014
DISEASE ALERTS/OUTBREAKS REPORTED AND RESPONDED TO BY STATES/UTs THROUGH INTEGRATED DISEASE SURVEILLANCE PROGRAMME (IDSP) 49th week (1st December to 7th December) 2014 District wise disease alerts/outbreaks reported in the 49th week, 2014 Reporting Status of States/UT’s No. of States/UT’s Submitted outbreak report ( including NIL report) 32 No. of States/UT’s Submitted ‘NIL’ outbreak report 14 INTEGRATED DISEASE SURVEILLANCE PROGRAMME, NATIONAL CENTRE FOR DISEASE CONTROL, DELHI Tel No. 23913148, Fax No. 23922677; www.idsp.nic.in Date of Comments/ Action Taken Name of Name of No. of No. of Date of Current S. No. Disease/ Illness Start of State/UT District Cases Deaths Reporting Status Outbreak Cases reported from Village Bodamolladinne, SC Isukanuthapalli, PHC CTM,Mandal Madanapalle District Chittoor. District RRT investigated the outbreak. Out of 08 water samples collected and sent to Regional Public Health i. Acute Under Lab, Tirupati, only 02 samples were found to be potable. All Chittoor diarrheal 22 02 29/11/14 08/12/14 control 03 rectal swabs sent to SVIMS Tirupati tested negative for disease any pathogen. 02 females aged 16& 45 years died due to the condition. A medical camp was organized. Water tanks were Andhra 1. cleaned and water chlorinated. Health education given on Pradesh personal hygiene and environmental hygiene. Cases reported from Village Kotbarpally, SC Sangakalam, PHC Gingurthy, District Ranga Reddy. District RRT ii. Food Under investigated the outbreak All the cases had history of Ranga Reddy 19 0 05/12/14 09/12/14 poisoning control consumption of midday meal. Health education given on drinking water and personal hygiene. -

KERALA SOLID WASTE MANAGEMENT PROJECT (KSWMP) with Financial Assistance from the World Bank
KERALA SOLID WASTE MANAGEMENT Public Disclosure Authorized PROJECT (KSWMP) INTRODUCTION AND STRATEGIC ENVIROMENTAL ASSESSMENT OF WASTE Public Disclosure Authorized MANAGEMENT SECTOR IN KERALA VOLUME I JUNE 2020 Public Disclosure Authorized Prepared by SUCHITWA MISSION Public Disclosure Authorized GOVERNMENT OF KERALA Contents 1 This is the STRATEGIC ENVIRONMENTAL ASSESSMENT OF WASTE MANAGEMENT SECTOR IN KERALA AND ENVIRONMENTAL AND SOCIAL MANAGEMENT FRAMEWORK for the KERALA SOLID WASTE MANAGEMENT PROJECT (KSWMP) with financial assistance from the World Bank. This is hereby disclosed for comments/suggestions of the public/stakeholders. Send your comments/suggestions to SUCHITWA MISSION, Swaraj Bhavan, Base Floor (-1), Nanthancodu, Kowdiar, Thiruvananthapuram-695003, Kerala, India or email: [email protected] Contents 2 Table of Contents CHAPTER 1. INTRODUCTION TO THE PROJECT .................................................. 1 1.1 Program Description ................................................................................. 1 1.1.1 Proposed Project Components ..................................................................... 1 1.1.2 Environmental Characteristics of the Project Location............................... 2 1.2 Need for an Environmental Management Framework ........................... 3 1.3 Overview of the Environmental Assessment and Framework ............. 3 1.3.1 Purpose of the SEA and ESMF ...................................................................... 3 1.3.2 The ESMF process ........................................................................................ -
Technical Design for Component A
Consultancy Services for Implementation of Component-A of Last Mile Connectivity of NCRMP TECHNICAL DESIGN REPORT Version: 2.0 Credit # 4772-IN Submitted by: Telecommunications Consultants India Limited TCIL Bhawan, Greater Kailash Part – I New Delhi- 110 048, India. TECHNICAL DESIGN REPORT TCIL Document Details Project Title Consultancy Services for Implementation of Component-A of Last Mile Connectivity of National Cyclone Risk Mitigation Project (NCRMP) Report Title Technical Design Report Report Version Version 2.0 Client State Project Implementation Unit (SPIU) National Cyclone Risk Mitigation Project - Kerala (NCRMP- Kerala) Department of Disaster Management Government of Kerala Report Prepared by Project Team Date of Submission 19.12.2018 TCIL’s Point of Contact Mr. A. Sampath Kumar Team Leader Telecommunications Consultants India Limited TCIL Bhawan, Greater Kailash-I New Delhi-110048 [email protected] Private & Confidential Page 2 TECHNICAL DESIGN REPORT TCIL Contents List of Abbreviations ..................................................................................................................................... 4 1. Executive Summary ............................................................................................................................... 9 2. EARLY WARNING DISSEMINATION SYSTEM .......................................................................................... 9 3. Objective of the Project ..................................................................................................................... -

Accused Persons Arrested in Thiruvananthapuram Rural District from 15.04.2018 to 21.04.2018
Accused Persons arrested in Thiruvananthapuram Rural district from 15.04.2018 to 21.04.2018 Name of Name of the Name of the Place at Date & Arresting Court at Sl. Name of the Age & Cr. No & Sec Police father of Address of Accused which Time of Officer, which No. Accused Sex of Law Station Accused Arrested Arrest Rank & accused Designation produced 1 2 3 4 5 6 7 8 9 10 11 Thanseem A S , 764/18 U/S279 Parappanvilakom, Sub Inspector JFMC I 1 Sudheer Sundaran M, 31 Nalumukku 15.04.18 IPC & 185 of Attingal Edanjimoola, Azhoor of Police, Attingal MV Act Attingal Charuvila veedu, Thanseem A S , 765/18 Karichiyil, Sub Inspector JFMC I 2 Asokan Janardanan M, 45 Katcheri 15.04.18 U/S118(A) of Attingal Chittattinkara,Avanav of Police, Attingal KP Act anchery Attingal Thanseem A S , Rejula Manzil, 766/18 U/S279 Sub Inspector JFMC I 3 Sajan Habeebulla M, 32 Mananakku, Katcheri 15.04.18 IPC & 185 of Attingal of Police, Attingal Manamboor MV Act Attingal Thanseem A S , Shailaja Bhavan, Near 767/18 Sub Inspector JFMC I 4 Sanjeep Santhulla M, 23 AJ College, Pvt Bus satnd 15.04.18 U/S118(A) of Attingal of Police, Attingal Thonnakkal KP Act Attingal Thanseem A S , Ratheesh Bhavan, 768/18 U/S279 Katcheri Sub Inspector JFMC I 5 Rajesh Retnakaran M, 32 Seemavila, 15.04.18 IPC & 185 of Attingal junction of Police, Attingal Koduvazhannoor MV Act Attingal Thanseem A S , 769/18 U/S279 Radhakrishna Kuzhivilakom Veedu, Sub Inspector JFMC I 6 Arjunan M, 21 Katcheri Jn 15.04.18 IPC & 185 of Attingal Kurup Mundayil, Varakal of Police, Attingal MV Act Attingal Aswathy veedu, Near Thanseem A S , 770/18 U/S279 Mahadevar kovil, Sub Inspector JFMC I 7 Akhil Sugunan M, 22 Katcheri 15.04.18 IPC & 185 of Attingal Irattakkalngu, of Police, Attingal MV Act Kizhuvilam Attingal Thanseem A S , Geethanjali veedu, 771/18 U/S279 Sub Inspector JFMC I 8 Ajin Anilkumar M, 22 Valiyakunnu, Katcheri 15.04.18 IPC & 185 of Attingal of Police, Attingal Kizhuvilam MV Act Attingal Thanseem A S , bhamalayam, 772/18 U/S279 Sub Inspector JFMC I 9 Vinod Gopi M, 47 Kattumpuram,. -

Fish and Shell Fish Fauna of the Retting and Nonretting Zones of the Kadinamkulam Kayal, Kerala
Fish and shell fish fauna of the retting and nonretting zones of the Kadinamkulam kayal, Kerala Item Type article Authors Bijoy Nandan, S.; Abdul Azis, P.K. Download date 02/10/2021 13:10:23 Link to Item http://hdl.handle.net/1834/32164 Journal of the Indian Fisheries Associank at. 35 23, 1993, 35-43 FISH AND SHELL FISH FAUNA OF THE RETTING AND NONRETT1NG ZONES OF THE KADINAMKULAM KAYAL, KERALA S. BUOY NANDAN* AND P.K. ABDUL AZIS Department of Aquatic Biology & Fisheries, University of Kerala, Trivandrum - 695 007 AI$STRACT Retting of coconut husk is one of the major problems of pollution hi the estuaries (kayals) of Kerala. Retting activity has resulted in the mass destruction of the flora and fauna and has converted sizeable sections of the kayal into virtual cesspools of foul smelling stagnant waters. Levels of hydrogen sulphide, phosphate and BOD, increased while dissi lived oxygen and fish and shellfish fauna decreased in the ambient waters. In the Kadinamkulam kayal a total of 37 species of fishes belonging to 26 families, 5 species of prawn and 2 species each of crabs and molluscs were recorded from the nonretting zone, whereas only 20 species of fish in dead condition were collected from the rating zone. Prawns, crabs and molluscs were absent at the vetting zone. IVIajority of the fish fauna in the kayal were marine forms. INTRODUCTION MATERIAL AND METHODS The rating of coconut husk has led to Two stations were selected in the extensive pollution of the clean and highly Kadinamkulam. kayal (lat.8°35'-8°40'N and productive estuaries of Kerala, The process of long. -

Thiruvananthapuram
GOVERNMENT OF KERALA DISTRICT SURVEY REPORT OF MINOR MINERALS (EXCEPT RIVER SAND) Prepared as per Environment Impact Assessment (EIA) Notification, 2006 issued under Environment (Protection) Act 1986 by DEPARTMENT OF MINING AND GEOLOGY www.dmg.kerala.gov.in November, 2016 Thiruvananthapuram Table of Contents Page No. 1. Introduction ............................................................................................................................... 3 2. Drainage ..................................................................................................................................... 5 3. Rainfall and climate.................................................................................................................... 6 4. Geology ...................................................................................................................................... 6 5. Geomorphology ......................................................................................................................... 9 6. Soil types .................................................................................................................................. 10 7. Groundwater scenario ............................................................................................................. 10 8. Natural hazards ........................................................................................................................ 13 9. Mineral Resources .................................................................................................................. -
Portly Problems Blue Growth Implementing the SSF Guidelines Women Fishworkers Safety at Sea a Rights-Based Approach to SSF
SAMUDRA Report No.73, April 2016 Item Type monograph Publisher International Collective in Support of Fishworkers Download date 02/10/2021 01:15:40 Link to Item http://hdl.handle.net/1834/35690 No. 73 | April 2016 issn 0973–1121 REPORT samudraTHE TRIANNUAL JOURNAL OF THE INTERNATIONAL COLLECTIVE IN SUPPORT OF FISHWORKERS Portly Problems Blue Growth Implementing the SSF Guidelines Women Fishworkers Safety at Sea A Rights-based Approach to SSF Fisheries, Communities, Livelihoods ICSF is an international NGO working on issues that concern and action, as well as communications. SAMUDRA Report invites fi shworkers the world over. It is in status with the Economic and contributions and responses. Correspondence should be addressed Social Council of the UN and is on ILO’s Special List of to Chennai, India. Non-governmental International Organizations. It also has Liaison Status with FAO. The opinions and positions expressed in the articles are those of the authors concerned and do not necessarily represent the As a global network of community organizers, teachers, offi cial views of ICSF. technicians, researchers and scientists, ICSF’s activities encompass monitoring and research, exchange and training, campaigns All issues of SAMUDRA Report can be accessed at www.icsf.net HHARINIARINI KKUMARUMAR REPORT FRONT COVER THE TRIANNUAL JOURNAL OF THE INTERNATIONAL COLLECTIVE IN SUPPORT OF FISHWORKERS NO.73 | APRIL 2016 samudraINFOSAMAK CENTER “Half-moon Boat Coming Out of the Sea” by Stella Maris Vallejo email: [email protected] PUBLISHED BY the International Collective in Support of Fishworkers 27 College Road Chennai 600 006, India Phone: (91) 44–2827 5303 Fax: (91) 44–2825 4457 Email: [email protected] ICSF BELGIUM OFFICE Sentier des Rossignols 2 1330 Rixensart, Belgium Phone: (32) 2–652 5201 Fax: (32) 2–654 0407 Email: [email protected] EDITED BY KG Kumar INDIA NORWAY DESIGNED BY P Sivasakthivel A casual approach ........................... -

NATIONAL MEANS CUM MERIT SCHOLARSHIP EXAMINATION (NMMSE)-2019 (FINAL LIST of ELIGIBLE CANDIDATES) THIRUVANANTHAPURAM DISTRICT GENERAL CATEGORY Sl
NATIONAL MEANS CUM MERIT SCHOLARSHIP EXAMINATION (NMMSE)-2019 (FINAL LIST OF ELIGIBLE CANDIDATES) THIRUVANANTHAPURAM DISTRICT GENERAL CATEGORY Sl. Caste ROLL NO Applicant Name School_Name No Category 1 42192790174 SREEHARI VINOD General Govt. Model HSS For Boys Attingal , Attingal 2 42192830290 GOPIKA I G General Govt. V.H.S.S. Kallara , KALLARA 3 42192730328 ARATHY M General GOVT. H S S, NEDUVELI, KONCHIRA, VEMBAYAM , 4 42192750125 ANAND SWAROOP J S General Govt. H S S Elampa , Elampa 5 42192740003 AMAL A L General L. V. H. S. Pothencode , Pothencode 6 42192860293 DEVANARAYANAN S R General P. P. M. H. S. Karakonam , karakonam 7 42192810350 KRIPA SUDISH General R R V GHSS Kilimanoor , kilimanoor 8 42192830280 ASNA S General Govt. V.H.S.S. Kallara , KALLARA 9 42192870029 AKHILA S General St. Thomas H. S. S. Amboori , Amboori 10 42192830299 MIDHUNA S NAIR General Govt. V.H.S.S. Kallara , KALLARA 11 42192740032 RESHMA S R General St. Goretti's Girls H. S. S. Nalanchira , Nalanchira 12 42192760120 ASHTAMI A S General DBHS Vamanapuram , vamanapuram 13 42192790241 GANGA G PRASANNAN General Govt H S S For Girls Attingal , Attingal 14 42192790227 ATHIDI ANILKUMAR General Govt H S S For Girls Attingal , Attingal 15 42192810135 DEVIKA B General Govt. HSS Kilimanoor , kilimanoor 16 42192820005 ADWAITH S R General Govt V H S S Njekkad , NJEKKAD 17 42192830371 RISHAV RAJ General M R M K M M H S S Edava , EDAVA 18 42192850125 SHANU S General St. Mary`s H. S. S. Vizhinjam , Vizhinjam 19 42192840321 JAYASREE J S General New H. S. -
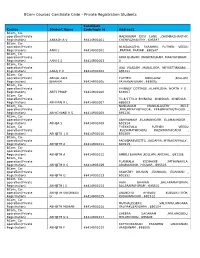
Bcom Courses Candidate Code – Private Registration Students
BCom Courses Candidate Code – Private Registration Students Candidate Course Student Name Code/login id Address1 BCom_ Co- operation(Private MADHAVAM DEVI LANE ,CHEMPAZHANTHY, Registration) AAKASH A V 88414901001 CHEMPAZHANTHY , 695587 BCom_ Co- operation(Private MUNDAKATHIL PARAMBIL PUTHEN VEEDU Registration) AANI S 88414901002 ,PRAYAR, PRAYAR , 690547 BCom_ Co- operation(Private ARYA BHAVAN ,MARIYAPURAM, MARIYAPURAM , Registration) AANI S S 88414901003 0 BCom_ Co- operation(Private JAYA VILASAM ,MANALOOR, NEYYATTINKARA , Registration) AARAJ P R 88414901004 695121 BCom_ Co- operation(Private ABDUL AZIZ PUTHEN BUNGLOW ,KOLLAM, Registration) IBRAHIM 88414901005 PATHANAPURAM , 689695 BCom_ Co- operation(Private PHINNEY COTTAGE ,ALAPPUZHA, NORTH P O , Registration) ABEY PHILIP 88414901006 688007 BCom_ Co- operation(Private TC-4/1779-9 BHINURA ,KOWDIAR, KOWDIAR , Registration) ABHI RAJ R L 88414901007 695003 BCom_ Co- NANDANAM MANGALASERY MELE operation(Private ,PERUMPAZHUTHOOR, PERUMPAZHUTHOOR , Registration) ABHICHAND R S 88414901008 695126 BCom_ Co- operation(Private ABHIRAMAM ,ELAMANNOOR, ELAMANNOOR , Registration) ABHIJA S 88414901009 691524 BCom_ Co- THEKKEVILA PUTHEN VEEDU operation(Private ,KUZHIMATHICADU, KUZHIMATHICADU , Registration) ABHIJITH J G 88414901010 691509 BCom_ Co- operation(Private PADINJAREVEETTIL ,KADAPPA, MYNAGAPPALLY , Registration) ABHIJITH A 88414901011 690519 BCom_ Co- operation(Private Registration) ABHIJITH A 88414901012 AMBILI BHAVAN ,KOLLAM, ANCHAL , 691306 BCom_ Co- operation(Private PLANKALA KIZHAKKE ,PATHANAVILA, -

Accused Persons Arrested in Thiruvananthapuram Rural District from 12.05.2019To18.05.2019
Accused Persons arrested in Thiruvananthapuram Rural district from 12.05.2019to18.05.2019 Name of Name of the Name of the Place at Date & Arresting Court at Sl. Name of the Age & Cr. No & Sec Police father of Address of Accused which Time of Officer, which No. Accused Sex of Law Station Accused Arrested Arrest Rank & accused Designation produced 1 2 3 4 5 6 7 8 9 10 11 Cr 347/19, U/s 279 IPC & 3(1) Nazeerudeen K JFMC,Varka 1 Nikhil Cleetus Anchuthengu r/w 181 of MV A SI of police la Inchivilakom Veedu Act 19 Male Anchuthengu 12/5/2019 12.30 Hrs Anchuthengu Kettupura Colony Cr 348/19 U/S 42 Nazeerudeen K JFMC,Varka 2 Janardanan Kettupura Kettupura 15(c ) r/w 63 of Male A SI of police la Anchuthengu Abkari Act Vijayakumar 12/5/2019 15.00 Hrs Anchuthengu Kettupura Colony Cr 349/19 U/S 45 Nazeerudeen K JFMC,Varka 3 Janardanan Kettupura Vakkamkulam 15(c ) r/w 63 of Male A SI of police la Anchuthengu Abkari Act Jayakumar 12/5/2019 15.10 Hrs Anchuthengu Cr.350/19 U/s 49 Ayyappanthottam Nazeerudeen K JFMC,Varka 4 Santhosh Dharman 118(a) of KP Male Anchutheugu A SI of police la Kayikkara 12/5/2019 16.35 ActHrs Anchuthengu Puthumanl Cr 351/19, U/s 21 Purayidom Veedu 279 IPC & 3(1) S.Prasad SI of JFMC,Varka 5 Vineeth Jeesus Dasan Male Mampally r/w 181 of MV Police la Anchuthengu Act Anchuthengu 13/5/2019 11.45 Hrs Anchuthengu 36 Mooppakudi Veedu Cr 352/19, U/s S.Prasad SI of JFMC,Varka 6 Thanzil Thaha Shappumukku Male Arivalam Vettoor 279 IPC Police la 13/5/2019 15.30 Hrs Anchuthengu Kizhakkeythitta Cr 353/19, U/s Kaladharan 33 Veedu Vadakkey JFMC,Varka -

Accused Persons Arrested in Thiruvananthapuram Rural District from 22.03.2015 to 28.03.2015
Accused Persons arrested in Thiruvananthapuram Rural district from 22.03.2015 to 28.03.2015 Name of Name of the Name of the Place at Date & Arresting Court at Sl. Name of the Age & Cr. No & Sec Police father of Address of Accused which Time of Officer, Rank which No. Accused Sex of Law Station Accused Arrested Arrest & accused Designation produced 1 2 3 4 5 6 7 8 9 10 11 Manappalli Cr.443/15 U/s Veedu,Altharamoodu, D.Unnikrishnan, JFMC 1 1 Suresh Madaswami 43.M Attingal 24/03/15 294(b),447,323 Attingal Darsanavattom,Nagar SCPO 9959 Attingal ,324,34 IPC oor Manappalli Cr.443/15 U/s Veedu,Altharamoodu, D.Unnikrishnan, JFMC 1 2 Leena Radha 37.F Attingal 24/03/15 294(b),447,323 Attingal Darsanavattom,Nagar SCPO 9959 Attingal ,324,34 IPC oor Manappalli Cr.443/15 U/s Veedu,Altharamoodu, D.Unnikrishnan, JFMC 1 3 Laila Kamala 51.F Attingal 24/03/15 294(b),447,323 Attingal Darsanavattom,Nagar SCPO 9959 Attingal ,324,34 IPC oor SAR Cr.480/15 U/s Manzil,Alamcode,The 25.03.2015, 118(i) of KP Act JFMC 1 4 Sharafudeen Abdul Rasaq 42.M Alamcode Attingal B.Jayan,SI ncherykonam,Manam 17.30 Hrs & 6(b) of Attingal boor COTPA Cr.508/15 Charuvila U/s118 Iof JS Praveen SI of 5 Sudharmani Parvathi 50 veedu,Nr.THQ Nr,.Govt HS 24-03-2015 Varkala JFMC I Varkala KPAct sec6 r/w Police Hospital,Varkala 24 of COTPA Cr.397/15 U/s.20 (b) (i)of M.Sukumar,Add Kunnil 23-03- Narcotic Drugs l.SI of JFMC 1 6 ChandraBose Vasu 66,m veedu,Mavinmoodu,O Mullaramcodu Kallambalam 15,15.00Hrs and Police,Kallambal Varkakala ttoor psychotropic am substance act Suji nivas, (CP/VIII)Nr.Guru G.