Byfavo, INN- Remimazolam
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Assessment Report
28 January 2021 EMA/160756/2021 Committee for Medicinal Products for Human Use (CHMP) Assessment report Byfavo International non-proprietary name: remimazolam Procedure No. EMEA/H/C/005246/0000 Note Assessment report as adopted by the CHMP with all information of a commercially confidential nature deleted. Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us An agency of the European Union Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 © European Medicines Agency, 2021. Reproduction is authorised provided the source is acknowledged. Table of contents List of abbreviations .................................................................................... 4 1. Background information on the procedure .............................................. 7 1.1. Submission of the dossier ...................................................................................... 7 1.2. Steps taken for the assessment of the product ......................................................... 8 2. Scientific discussion .............................................................................. 10 2.1. Problem statement ............................................................................................. 10 2.1.1. Disease or condition ......................................................................................... 10 2.1.2. Epidemiology ................................................................................................. -
Introduced B.,Byhansen, 16
LB301 LB301 2021 2021 LEGISLATURE OF NEBRASKA ONE HUNDRED SEVENTH LEGISLATURE FIRST SESSION LEGISLATIVE BILL 301 Introduced by Hansen, B., 16. Read first time January 12, 2021 Committee: Judiciary 1 A BILL FOR AN ACT relating to the Uniform Controlled Substances Act; to 2 amend sections 28-401, 28-405, and 28-416, Revised Statutes 3 Cumulative Supplement, 2020; to redefine terms; to change drug 4 schedules and adopt federal drug provisions; to change a penalty 5 provision; and to repeal the original sections. 6 Be it enacted by the people of the State of Nebraska, -1- LB301 LB301 2021 2021 1 Section 1. Section 28-401, Revised Statutes Cumulative Supplement, 2 2020, is amended to read: 3 28-401 As used in the Uniform Controlled Substances Act, unless the 4 context otherwise requires: 5 (1) Administer means to directly apply a controlled substance by 6 injection, inhalation, ingestion, or any other means to the body of a 7 patient or research subject; 8 (2) Agent means an authorized person who acts on behalf of or at the 9 direction of another person but does not include a common or contract 10 carrier, public warehouse keeper, or employee of a carrier or warehouse 11 keeper; 12 (3) Administration means the Drug Enforcement Administration of the 13 United States Department of Justice; 14 (4) Controlled substance means a drug, biological, substance, or 15 immediate precursor in Schedules I through V of section 28-405. 16 Controlled substance does not include distilled spirits, wine, malt 17 beverages, tobacco, hemp, or any nonnarcotic substance if such substance 18 may, under the Federal Food, Drug, and Cosmetic Act, 21 U.S.C. -

Remimazolam Manufacturer1
Brand Name: Byfavo Generic Name: Remimazolam Manufacturer1: Acacia Pharma, Inc Drug Class1,2,3,4,5: Benzodiazepine Labeled Uses1,2,3,4,5:Sedation for Procedures lasting 30 minutes or less Mechanism of Action1,2,3,4,5: Remimazolam is a benzodiazepine that binds to GABA-A receptors in the brain. The formation of the benzodiazepine-GABA complex increases the effects of GABA which increases the inhibition of the ascending reticular activating system. It appears that Remimazolam does not have selectivity between different GABA receptors. Pharmacokinetics1,2,3,4,5: Absorption: Tmax 20-30 minutes Vd 0.76-0.98 L/kg T1/2 37-53 minutes Clearance 54-75 L/hr Protein Binding >91% Bioavailability Unknown Metabolism: Remimazolam is metabolized by tissue carboxylesterases to an inactive metabolite CNS7054. There does not appear to be any major CYP450 metabolism. Elimination: Remimazolam is mainly excreted in the urine as its metabolite CNS7054 (50- 60%). A very small amount of remimazolam is also excreted unchanged in the urine (0.003%) Efficacy6,7,8: Borkett KM, Riff DS, Schwartz HI, et al. A Phase IIa, randomized, double-blind study of remimazolam (CNS 7056) versus midazolam for sedation in upper gastrointestinal endoscopy. Anesth Analg. 2015;120(4):771-780. Study Design: Randomized, double blind, active control, parallel study Description of Study: Methods: 100 patients were randomly assigned in a 1:1:1:1 ratio to 1 of 4 treatment groups: one dose of remimazolam 0.1, 0.15, or 0.2 mg/kg; or one dose of midazolam 0.075 mg/kg. The patients were given their medication as an IV injection over one-minute by an anesthesiologist. -
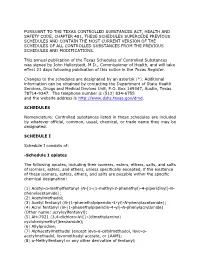
Schedules of Controlled Substances (.Pdf)
PURSUANT TO THE TEXAS CONTROLLED SUBSTANCES ACT, HEALTH AND SAFETY CODE, CHAPTER 481, THESE SCHEDULES SUPERCEDE PREVIOUS SCHEDULES AND CONTAIN THE MOST CURRENT VERSION OF THE SCHEDULES OF ALL CONTROLLED SUBSTANCES FROM THE PREVIOUS SCHEDULES AND MODIFICATIONS. This annual publication of the Texas Schedules of Controlled Substances was signed by John Hellerstedt, M.D., Commissioner of Health, and will take effect 21 days following publication of this notice in the Texas Register. Changes to the schedules are designated by an asterisk (*). Additional information can be obtained by contacting the Department of State Health Services, Drugs and Medical Devices Unit, P.O. Box 149347, Austin, Texas 78714-9347. The telephone number is (512) 834-6755 and the website address is http://www.dshs.texas.gov/dmd. SCHEDULES Nomenclature: Controlled substances listed in these schedules are included by whatever official, common, usual, chemical, or trade name they may be designated. SCHEDULE I Schedule I consists of: -Schedule I opiates The following opiates, including their isomers, esters, ethers, salts, and salts of isomers, esters, and ethers, unless specifically excepted, if the existence of these isomers, esters, ethers, and salts are possible within the specific chemical designation: (1) Acetyl-α-methylfentanyl (N-[1-(1-methyl-2-phenethyl)-4-piperidinyl]-N- phenylacetamide); (2) Acetylmethadol; (3) Acetyl fentanyl (N-(1-phenethylpiperidin-4-yl)-N-phenylacetamide); (4) Acryl fentanyl (N-(1-phenethylpiperidin-4-yl)-N-phenylacrylamide) (Other name: -
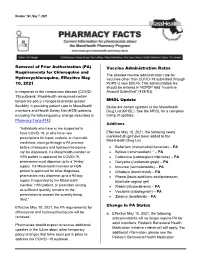
Removal of Prior Authorization (PA) Requirements for Chloroquine And
Pharmacy Facts Number 163, May 7, 2021 Removal of Prior Authorization (PA) Vaccine Administration Rates Requirements for Chloroquine and The allowed vaccine administration rate for Hydroxychloroquine, Effective May vaccines other than COVID-19 submitted through 10, 2021 POPS is now $20.45. This administration fee should be entered in NCPDP field “Incentive In response to the coronavirus disease (COVID- Amount Submitted” (438-E3) 19) outbreak, MassHealth announced certain temporary policy changes to provide greater MHDL Update flexibility in providing patient care to MassHealth Below are certain updates to the MassHealth members and Health Safety Net (HSN) patients, Drug List (MHDL). See the MHDL for a complete including the following policy change described in listing of updates. Pharmacy Facts #143: Additions “Individuals who have or are suspected to have COVID-19, or who have new Effective May 10, 2021, the following newly prescriptions for lupus, malaria, or rheumatic marketed drugs have been added to the MassHealth Drug List. conditions, must go through a PA process before chloroquine and hydroxychloroquine • Bafiertam (monomethyl fumarate) – PA can be dispensed. If a MassHealth member or • Byfavo (remimazolam) ^ – PA HSN patient is approved for COVID-19, • Cabenuva (cabotegravir/rilpivirine) – PA pharmacies must dispense up to a 14-day • Danyelza (naxitamab-gqgk) – PA supply. If a MassHealth member or HSN • Imcivree (setmelanotide) – PA patient is approved for other diagnoses, • Orladeyo (berotralstat) – PA pharmacies may dispense up to a 90-day • Phexxi (lactic acid/citric acid/potassium supply if requested by the MassHealth bitartrate vaginal gel) member, HSN patient, or prescriber as long • Riabni (rituximab-arrx) – PA as sufficient quantity remains on the • Vocabria (cabotegravir) – PA prescription to support the quantity being • Zokinvy (lonafarnib) – PA filled.” Change in PA Status Effective May 10, 2021, the PA requirements for chloroquine and hydroxychloroquine will be a. -

Laws 2021, LB236, § 4
LB236 LB236 2021 2021 LEGISLATIVE BILL 236 Approved by the Governor May 26, 2021 Introduced by Brewer, 43; Clements, 2; Erdman, 47; Slama, 1; Lindstrom, 18; Murman, 38; Halloran, 33; Hansen, B., 16; McDonnell, 5; Briese, 41; Lowe, 37; Groene, 42; Sanders, 45; Bostelman, 23; Albrecht, 17; Dorn, 30; Linehan, 39; Friesen, 34; Aguilar, 35; Gragert, 40; Kolterman, 24; Williams, 36; Brandt, 32. A BILL FOR AN ACT relating to law; to amend sections 28-1202 and 69-2436, Reissue Revised Statutes of Nebraska, and sections 28-401 and 28-405, Revised Statutes Cumulative Supplement, 2020; to redefine terms, change drug schedules, and adopt federal drug provisions under the Uniform Controlled Substances Act; to provide an exception to the offense of carrying a concealed weapon as prescribed; to define a term; to change provisions relating to renewal of a permit to carry a concealed handgun; to provide a duty for the Nebraska State Patrol; to eliminate an obsolete provision; to harmonize provisions; and to repeal the original sections. Be it enacted by the people of the State of Nebraska, Section 1. Section 28-401, Revised Statutes Cumulative Supplement, 2020, is amended to read: 28-401 As used in the Uniform Controlled Substances Act, unless the context otherwise requires: (1) Administer means to directly apply a controlled substance by injection, inhalation, ingestion, or any other means to the body of a patient or research subject; (2) Agent means an authorized person who acts on behalf of or at the direction of another person but does not include a common or contract carrier, public warehouse keeper, or employee of a carrier or warehouse keeper; (3) Administration means the Drug Enforcement Administration of the United States Department of Justice; (4) Controlled substance means a drug, biological, substance, or immediate precursor in Schedules I through V of section 28-405. -

Byfavo (Previously Aptimyda) 2Nd D195 JRAR EN PI
Package leaflet: Information for the patient Byfavo 20 mg powder for solution for injection remimazolam This medicine is subject to additional monitoring. This will allow quick identification of new safety information. You can help by reporting any side effects you may get. See the end of section 4 for how to report side effects. Read all of this leaflet carefully before you are given this medicine because it contains important information for you. - Keep this leaflet. You may need to read it again. -If you have any further questions, ask your doctor or nurse. -If you get any side effects, talk to your doctor or nurse. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet 1. What Byfavo is and what it is used for 2. What you need to know before you are given Byfavo 3. How Byfavo is given 4. Possible side effects 5. How Byfavo is stored 6. Contents of the pack and other information 1. What Byfavo is and what it is used for Byfavo is a medicine that contains the active substance remimazolam. Remimazolam is one of a group of substances known as benzodiazepines. Byfavo is a sedative given before a medical test or procedure to make you feel relaxed and sleepy (sedated). 2. What you need to know before you are given Byfavo You must not be given Byfavo if: - you are allergic to remimazolam or other benzodiazepines (such as midazolam) or any of the other ingredients of this medicine (listed in section 6). -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

Emerging Approaches in Intravenous Moderate and Deep Sedation
Journal of Clinical Medicine Review Emerging Approaches in Intravenous Moderate and Deep Sedation Basavana Goudra 1,* and Keira P. Mason 2 1 Department of Anesthesiology and Critical Care Medicine, Hospital of the University of Pennsylvania, Philadelphia, PA 19104, USA 2 Department of Anesthesiology, Children’s Hospital Boston, Harvard Medical School, Boston, MA 02115, USA; [email protected] * Correspondence: [email protected] Abstract: Successful pharmacological innovations that have made a difference in daily practice are rare in the world of anesthesia and sedation. After many years of research, it seems that we finally have two new drug innovations that are likely to change the paradigm of moderate and deep sedation. These are oliceridine and remimazolam. Both have been in development for over a decade. Oliceridine was synthesized in a lab as an entirely new molecule. It is a biased µ- receptor agonist that acts preferentially on the G-protein pathway (which is responsible for analgesia). At least in lower doses, it has minimal effect on the beta-arrestin pathway, which is responsible for unwanted effects of µ-opioid receptor activation such as respiratory depression and gastrointestinal dysfunction. Like any other µ- receptor agonist, it produces appropriate dose-dependent analgesia. Remimazolam is structurally similar to midazolam; however, it has an additional ester linkage that delivers the kinetics of remifentanil. As a result, while pharmacodynamically identical to midazolam, remimazolam is metabolized by ester hydrolysis and subsequently its elimination is rapid and predictable. The present review discusses the two drugs in detail with a particular emphasis on their potential role in Citation: Goudra, B.; Mason, K.P. -

212295Orig1s000 SUMMARY REVIEW
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 212295Orig1s000 SUMMARY REVIEW Food and Drug Administration CENTER FOR DRUG EVALUATION AND RESEARCH Division of Anesthesiology, Addiction Medicine, and Pain Medicine 10903 New Hampshire Ave. Silver Spring, MD 20993-0002 Division Director Summary and Cross-Discipline Team Leader Review Date July 2, 2020 Martha A. Van Clief, MD, Team Leader From Rigoberto Roca, MD, Division Director NDA Number 212295 Cosmo Technologies, Ltd., Dublin, Ireland Applicant (U.S. Agent - Conventus Biomedical Solutions, Inc.) Date of Submission April 5, 2019 PDUFA Goal Date July 3, 2020 Proprietary Name Byfavo Established or Proper Name Remimazolam Dosage Form/Strength Solution for intravenous administration, 2.5 mg/mL Applicant Proposed For the induction and maintenance of procedural Indication/Population sedation in adults. Adult Patients: • Administer an initial dose of Byfavo intravenously as a 5 mg (2 mL) push injection over a 1-minute time period. • If necessary, administer supplemental doses of 2.5 mg (1 mL) Byfavo over a 15-second time period. • At least 2 minutes must have elapsed prior to the Applicant Proposed Dosing administration of any supplemental dose. Regimen Debilitated Patients (ASA III-IV, at the discretion of the physician): • Based on the general condition of the patient, administer 2.5 to 5 mg (1 or 2 mL) of Byfavo over 1-minute time period. If necessary, administer supplemental doses of 1.25 to 2.5 mg (0.5 or 1 mL) Byfavo as a push injection over a 15 second time period. Regulatory Action Approval For the induction and maintenance of procedural Recommended Indication sedation in adults undergoing procedures lasting 30 minutes or less. -

New Horizons for Sedation the Ultrashort Acting Benzodiazepine
Techniques in Gastrointestinal Endoscopy 18 (2016) 22–28 Contents lists available at ScienceDirect Techniques in Gastrointestinal Endoscopy journal homepage: www.techgiendoscopy.com/locate/tgie New horizons for sedation: The ultrashort acting benzodiazepine remimazolam Daniel J. Pambiancoa,1,2,n, Brooks D. Cashb,2 a Charlottesville Medical Research, 325 Winding River Lane, Suite 102, Charlottesville, Virginia 22911 b Digestive Health Center, University of South Alabama, Mobile, Alabama article info abstract Article history: Procedural sedation is used in 98% of endoscopies performed in the United States. The predominant agents Received 17 November 2015 used are benzodiazepines, opioids, and propofol. The optimal sedation depends on the procedure being Accepted 11 February 2016 performed and its duration. An ideal sedative would allow for flexible, rapid onset and offset of sedation with predictable short duration of action with minimal cardiopulmonary risk factors. Remimazolam is a Keywords: novel “soft drug” with the characteristics of a benzodiazepine and organ-independent metabolism. Remimazolam Remimazolam binds selectively and with high affinity to the gamma-aminobutyric acid receptor, with Benzodiazepine no off-target activities. In animal studies, remimazolam has a short, initial phase half-life and high volume Procedural sedation of distribution, indicating extensive tissue distribution, minimal tissue accumulation, and rapid elimina- Pharmacokinetics tion. Remimazolam is hydroxylated to an inactive metabolite, and its effects can be reversed with Clinical trials flumazenil. In clinical studies for procedural sedation, remimazolam was well tolerated with no serious Gastrointestinal endoscopy adverse events. Times to onset or offset of sedation were shorter with remimazolam versus active control. All remimazolam-related adverse reactions are well known to clinicians and can be managed by trained staff. -

Pipeline Report May 2020
Pipeline Report May 2020 Pipeline Report May 2020 © 2020 Envolve. All rights reserved. Page 1 This quarterly at-a-glance publication is developed by our Clinical Pharmacy Drug Information team to Table of Contents increase your understanding of the drug pipeline, ensuring you’re equipped with insights to prepare Recent Specialty Drug Approvals 1 for shifts in pharmacy benefit management. In this issue, you’ll learn more about these key themes and notable drugs: Recent Non-Specialty Drug Approvals 2 > Despite the FDA’s recent intense focus on COVID- 19-related activities, oncology drug pipeline is one Upcoming Specialty Products 3 therapeutic area which remains vibrant in the immediate term. This is evidenced by the consistent rate of FDA approvals, as well as acceptance of New Drug and Biologic License Applications for review. In fact, multiple oncology agents were Upcoming Non-Specialty Products 7 FDA-approved several months ahead of schedule, underscoring the urgency with which the FDA continues to act on oncologic agents. Biosimilars 9 > Several pipeline agents on this quarterly report are worth highlighting as possible new alternatives in high-cost disease states with few therapeutic options. These Generic Specialty Agents 10 agents include viltolarsen in the treatment of Duchenne muscular dystrophy (DMD), fostemsavir in the treatment of heavily treatment-experienced adult patients with HIV, and roxadustat which offers the first oral alternative to Generic Non-Specialty Agents 11 injectable agents such as Aranesp, Epogen and Procrit, for the treatment of anemia associated with chronic kidney disease. To prepare this report, our team accesses a wide range of clinical resources.