Emerging Approaches in Intravenous Moderate and Deep Sedation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ong Edmund W 201703 Phd.Pdf (5.844Mb)
INVESTIGATING THE EFFECTS OF PROLONGED MU OPIOID RECEPTOR ACTIVATION UPON OPIOID RECEPTOR HETEROMERIZATION by Edmund Wing Ong A thesis submitted to the Graduate Program in Pharmacology & Toxicology in the Department of Biomedical and Molecular Sciences In conformity with the requirements for the degree of Doctor of Philosophy Queen’s University Kingston, Ontario, Canada March, 2017 Copyright © Edmund Wing Ong, 2017 Abstract Opioid receptors are the sites of action for morphine and most other clinically-used opioid drugs. Abundant evidence now demonstrates that different opioid receptor types can physically associate to form heteromers. Owing to their constituent monomers’ involvement in analgesia, mu/delta opioid receptor (M/DOR) heteromers have been a particular focus of attention. Understandings of the physiological relevance of M/DOR formation remain limited in large part due to the reliance of existing M/DOR findings upon contrived heterologous systems. This thesis investigated the physiological relevance of M/DOR generation following prolonged MOR activation. To address M/DOR in endogenous tissues, suitable model systems and experimental tools were established. This included a viable dorsal root ganglion (DRG) neuron primary culture model, antisera specifically directed against M/DOR, a quantitative immunofluorescence colocalizational analysis method, and a floxed-Stop, FLAG-tagged DOR conditional knock-in mouse model. The development and implementation of such techniques make it possible to conduct experiments addressing the nature of M/DOR heteromers in systems with compelling physiological relevance. Seeking to both reinforce and extend existing findings from heterologous systems, it was first necessary to demonstrate the existence of M/DOR heteromers. Using antibodies directed against M/DOR itself as well as constituent monomers, M/DOR heteromers were identified in endogenous tissues and demonstrated to increase in abundance following prolonged mu opioid receptor (MOR) activation by morphine. -

Biased Versus Partial Agonism in the Search for Safer Opioid Analgesics
molecules Review Biased versus Partial Agonism in the Search for Safer Opioid Analgesics Joaquim Azevedo Neto 1 , Anna Costanzini 2 , Roberto De Giorgio 2 , David G. Lambert 3 , Chiara Ruzza 1,4,* and Girolamo Calò 1 1 Department of Biomedical and Specialty Surgical Sciences, Section of Pharmacology, University of Ferrara, 44121 Ferrara, Italy; [email protected] (J.A.N.); [email protected] (G.C.) 2 Department of Morphology, Surgery, Experimental Medicine, University of Ferrara, 44121 Ferrara, Italy; [email protected] (A.C.); [email protected] (R.D.G.) 3 Department of Cardiovascular Sciences, Anesthesia, Critical Care and Pain Management, University of Leicester, Leicester LE1 7RH, UK; [email protected] 4 Technopole of Ferrara, LTTA Laboratory for Advanced Therapies, 44122 Ferrara, Italy * Correspondence: [email protected] Academic Editor: Helmut Schmidhammer Received: 23 July 2020; Accepted: 23 August 2020; Published: 25 August 2020 Abstract: Opioids such as morphine—acting at the mu opioid receptor—are the mainstay for treatment of moderate to severe pain and have good efficacy in these indications. However, these drugs produce a plethora of unwanted adverse effects including respiratory depression, constipation, immune suppression and with prolonged treatment, tolerance, dependence and abuse liability. Studies in β-arrestin 2 gene knockout (βarr2( / )) animals indicate that morphine analgesia is potentiated − − while side effects are reduced, suggesting that drugs biased away from arrestin may manifest with a reduced-side-effect profile. However, there is controversy in this area with improvement of morphine-induced constipation and reduced respiratory effects in βarr2( / ) mice. Moreover, − − studies performed with mice genetically engineered with G-protein-biased mu receptors suggested increased sensitivity of these animals to both analgesic actions and side effects of opioid drugs. -

Summary Analgesics Dec2019
Status as of December 31, 2019 UPDATE STATUS: N = New, A = Advanced, C = Changed, S = Same (No Change), D = Discontinued Update Emerging treatments for acute and chronic pain Development Status, Route, Contact information Status Agent Description / Mechanism of Opioid Function / Target Indication / Other Comments Sponsor / Originator Status Route URL Action (Y/No) 2019 UPDATES / CONTINUING PRODUCTS FROM 2018 Small molecule, inhibition of 1% diacerein TWi Biotechnology / caspase-1, block activation of 1 (AC-203 / caspase-1 inhibitor Inherited Epidermolysis Bullosa Castle Creek Phase 2 No Topical www.twibiotech.com NLRP3 inflamasomes; reduced CCP-020) Pharmaceuticals IL-1beta and IL-18 Small molecule; topical NSAID Frontier 2 AB001 NSAID formulation (nondisclosed active Chronic low back pain Phase 2 No Topical www.frontierbiotech.com/en/products/1.html Biotechnologies ingredient) Small molecule; oral uricosuric / anti-inflammatory agent + febuxostat (xanthine oxidase Gout in patients taking urate- Uricosuric + 3 AC-201 CR inhibitor); inhibition of NLRP3 lowering therapy; Gout; TWi Biotechnology Phase 2 No Oral www.twibiotech.com/rAndD_11 xanthine oxidase inflammasome assembly, reduced Epidermolysis Bullosa Simplex (EBS) production of caspase-1 and cytokine IL-1Beta www.arraybiopharma.com/our-science/our-pipeline AK-1830 Small molecule; tropomyosin Array BioPharma / 4 TrkA Pain, inflammation Phase 1 No Oral www.asahi- A (ARRY-954) receptor kinase A (TrkA) inhibitor Asahi Kasei Pharma kasei.co.jp/asahi/en/news/2016/e160401_2.html www.neurosmedical.com/clinical-research; -

Assessment Report
28 January 2021 EMA/160756/2021 Committee for Medicinal Products for Human Use (CHMP) Assessment report Byfavo International non-proprietary name: remimazolam Procedure No. EMEA/H/C/005246/0000 Note Assessment report as adopted by the CHMP with all information of a commercially confidential nature deleted. Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us An agency of the European Union Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 © European Medicines Agency, 2021. Reproduction is authorised provided the source is acknowledged. Table of contents List of abbreviations .................................................................................... 4 1. Background information on the procedure .............................................. 7 1.1. Submission of the dossier ...................................................................................... 7 1.2. Steps taken for the assessment of the product ......................................................... 8 2. Scientific discussion .............................................................................. 10 2.1. Problem statement ............................................................................................. 10 2.1.1. Disease or condition ......................................................................................... 10 2.1.2. Epidemiology ................................................................................................. -

The Main Tea Eta a El Mattitauli Mali Malta
THE MAIN TEA ETA USA 20180169172A1EL MATTITAULI MALI MALTA ( 19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2018 /0169172 A1 Kariman (43 ) Pub . Date : Jun . 21 , 2018 ( 54 ) COMPOUND AND METHOD FOR A61K 31/ 437 ( 2006 .01 ) REDUCING APPETITE , FATIGUE AND PAIN A61K 9 / 48 (2006 .01 ) (52 ) U . S . CI. (71 ) Applicant : Alexander Kariman , Rockville , MD CPC . .. .. .. .. A61K 36 / 74 (2013 .01 ) ; A61K 9 / 4825 (US ) (2013 . 01 ) ; A61K 31/ 437 ( 2013 . 01 ) ; A61K ( 72 ) Inventor: Alexander Kariman , Rockville , MD 31/ 4375 (2013 .01 ) (US ) ( 57 ) ABSTRACT The disclosed invention generally relates to pharmaceutical (21 ) Appl . No. : 15 /898 , 232 and nutraceutical compounds and methods for reducing appetite , muscle fatigue and spasticity , enhancing athletic ( 22 ) Filed : Feb . 16 , 2018 performance , and treating pain associated with cancer, trauma , medical procedure , and neurological diseases and Publication Classification disorders in subjects in need thereof. The disclosed inven ( 51 ) Int. Ci. tion further relates to Kratom compounds where said com A61K 36 / 74 ( 2006 .01 ) pound contains at least some pharmacologically inactive A61K 31/ 4375 ( 2006 .01 ) component. pronuPatent Applicationolan Publication manu saJun . decor21, 2018 deSheet les 1 of 5 US 2018 /0169172 A1 reta Mitragynine 7 -OM - nitragynine *** * *momoda W . 00 . Paynantheine Speciogynine **** * * * ! 1000 co Speclociliatine Corynartheidine Figure 1 Patent Application Publication Jun . 21, 2018 Sheet 2 of 5 US 2018 /0169172 A1 -
Introduced B.,Byhansen, 16
LB301 LB301 2021 2021 LEGISLATURE OF NEBRASKA ONE HUNDRED SEVENTH LEGISLATURE FIRST SESSION LEGISLATIVE BILL 301 Introduced by Hansen, B., 16. Read first time January 12, 2021 Committee: Judiciary 1 A BILL FOR AN ACT relating to the Uniform Controlled Substances Act; to 2 amend sections 28-401, 28-405, and 28-416, Revised Statutes 3 Cumulative Supplement, 2020; to redefine terms; to change drug 4 schedules and adopt federal drug provisions; to change a penalty 5 provision; and to repeal the original sections. 6 Be it enacted by the people of the State of Nebraska, -1- LB301 LB301 2021 2021 1 Section 1. Section 28-401, Revised Statutes Cumulative Supplement, 2 2020, is amended to read: 3 28-401 As used in the Uniform Controlled Substances Act, unless the 4 context otherwise requires: 5 (1) Administer means to directly apply a controlled substance by 6 injection, inhalation, ingestion, or any other means to the body of a 7 patient or research subject; 8 (2) Agent means an authorized person who acts on behalf of or at the 9 direction of another person but does not include a common or contract 10 carrier, public warehouse keeper, or employee of a carrier or warehouse 11 keeper; 12 (3) Administration means the Drug Enforcement Administration of the 13 United States Department of Justice; 14 (4) Controlled substance means a drug, biological, substance, or 15 immediate precursor in Schedules I through V of section 28-405. 16 Controlled substance does not include distilled spirits, wine, malt 17 beverages, tobacco, hemp, or any nonnarcotic substance if such substance 18 may, under the Federal Food, Drug, and Cosmetic Act, 21 U.S.C. -

Remimazolam Manufacturer1
Brand Name: Byfavo Generic Name: Remimazolam Manufacturer1: Acacia Pharma, Inc Drug Class1,2,3,4,5: Benzodiazepine Labeled Uses1,2,3,4,5:Sedation for Procedures lasting 30 minutes or less Mechanism of Action1,2,3,4,5: Remimazolam is a benzodiazepine that binds to GABA-A receptors in the brain. The formation of the benzodiazepine-GABA complex increases the effects of GABA which increases the inhibition of the ascending reticular activating system. It appears that Remimazolam does not have selectivity between different GABA receptors. Pharmacokinetics1,2,3,4,5: Absorption: Tmax 20-30 minutes Vd 0.76-0.98 L/kg T1/2 37-53 minutes Clearance 54-75 L/hr Protein Binding >91% Bioavailability Unknown Metabolism: Remimazolam is metabolized by tissue carboxylesterases to an inactive metabolite CNS7054. There does not appear to be any major CYP450 metabolism. Elimination: Remimazolam is mainly excreted in the urine as its metabolite CNS7054 (50- 60%). A very small amount of remimazolam is also excreted unchanged in the urine (0.003%) Efficacy6,7,8: Borkett KM, Riff DS, Schwartz HI, et al. A Phase IIa, randomized, double-blind study of remimazolam (CNS 7056) versus midazolam for sedation in upper gastrointestinal endoscopy. Anesth Analg. 2015;120(4):771-780. Study Design: Randomized, double blind, active control, parallel study Description of Study: Methods: 100 patients were randomly assigned in a 1:1:1:1 ratio to 1 of 4 treatment groups: one dose of remimazolam 0.1, 0.15, or 0.2 mg/kg; or one dose of midazolam 0.075 mg/kg. The patients were given their medication as an IV injection over one-minute by an anesthesiologist. -

The Utilization of Mu-Opioid Receptor Biased Agonists: Oliceridine, an Opioid Analgesic with Reduced Adverse Effects
Current Pain and Headache Reports (2019) 23: 31 https://doi.org/10.1007/s11916-019-0773-1 HOT TOPICS IN PAIN AND HEADACHE (N. ROSEN, SECTION EDITOR) The Utilization of Mu-Opioid Receptor Biased Agonists: Oliceridine, an Opioid Analgesic with Reduced Adverse Effects Ivan Urits1 & Omar Viswanath2,3,4 & Vwaire Orhurhu1 & Kyle Gress5 & Karina Charipova5 & Alan D. Kaye6 & Anh Ngo1 Published online: 18 March 2019 # Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Purpose of Review The purpose of this review is to summarize the current understanding of opioid pathways in mediating and/or modulating analgesia and adverse effects. Oliceridine is highlighted as a novel mu-opioid receptor agonist with selective activation of G protein and β-arrestin signaling pathways. Recent Findings Oliceridine (TRV130; [(3-methoxythiophen-2-yl)methyl]({2-[(9R)-9-(pyridin-2-yl)-6-oxaspiro[4.5]decan-9- yl]ethyl})amine) is a novel MOR agonist that selectively activates G protein and β-arrestin signaling pathways. A growing body of evidence suggests that compared to existing MOR agonists, Oliceridine and other G protein-selective modulators may produce therapeutic analgesic effects with reduced adverse effects. Summary Oliceridine provides analgesic benefits of a pure opioid agonist while limiting related adverse effects mediated through the β-arrestin pathway. Recent insights into the function and structure of G protein-coupled receptors has led to the development of novel analgesic therapies. Keywords Oliceridine . TRV130 . G protein-coupled receptors (GPCR) . Partial opioid agonists Introduction significant driver in an effort to develop novel opioid pharma- cotherapies with less adverse side effects. -
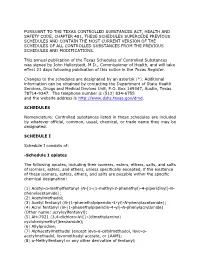
Schedules of Controlled Substances (.Pdf)
PURSUANT TO THE TEXAS CONTROLLED SUBSTANCES ACT, HEALTH AND SAFETY CODE, CHAPTER 481, THESE SCHEDULES SUPERCEDE PREVIOUS SCHEDULES AND CONTAIN THE MOST CURRENT VERSION OF THE SCHEDULES OF ALL CONTROLLED SUBSTANCES FROM THE PREVIOUS SCHEDULES AND MODIFICATIONS. This annual publication of the Texas Schedules of Controlled Substances was signed by John Hellerstedt, M.D., Commissioner of Health, and will take effect 21 days following publication of this notice in the Texas Register. Changes to the schedules are designated by an asterisk (*). Additional information can be obtained by contacting the Department of State Health Services, Drugs and Medical Devices Unit, P.O. Box 149347, Austin, Texas 78714-9347. The telephone number is (512) 834-6755 and the website address is http://www.dshs.texas.gov/dmd. SCHEDULES Nomenclature: Controlled substances listed in these schedules are included by whatever official, common, usual, chemical, or trade name they may be designated. SCHEDULE I Schedule I consists of: -Schedule I opiates The following opiates, including their isomers, esters, ethers, salts, and salts of isomers, esters, and ethers, unless specifically excepted, if the existence of these isomers, esters, ethers, and salts are possible within the specific chemical designation: (1) Acetyl-α-methylfentanyl (N-[1-(1-methyl-2-phenethyl)-4-piperidinyl]-N- phenylacetamide); (2) Acetylmethadol; (3) Acetyl fentanyl (N-(1-phenethylpiperidin-4-yl)-N-phenylacetamide); (4) Acryl fentanyl (N-(1-phenethylpiperidin-4-yl)-N-phenylacrylamide) (Other name: -
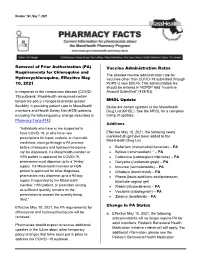
Removal of Prior Authorization (PA) Requirements for Chloroquine And
Pharmacy Facts Number 163, May 7, 2021 Removal of Prior Authorization (PA) Vaccine Administration Rates Requirements for Chloroquine and The allowed vaccine administration rate for Hydroxychloroquine, Effective May vaccines other than COVID-19 submitted through 10, 2021 POPS is now $20.45. This administration fee should be entered in NCPDP field “Incentive In response to the coronavirus disease (COVID- Amount Submitted” (438-E3) 19) outbreak, MassHealth announced certain temporary policy changes to provide greater MHDL Update flexibility in providing patient care to MassHealth Below are certain updates to the MassHealth members and Health Safety Net (HSN) patients, Drug List (MHDL). See the MHDL for a complete including the following policy change described in listing of updates. Pharmacy Facts #143: Additions “Individuals who have or are suspected to have COVID-19, or who have new Effective May 10, 2021, the following newly prescriptions for lupus, malaria, or rheumatic marketed drugs have been added to the MassHealth Drug List. conditions, must go through a PA process before chloroquine and hydroxychloroquine • Bafiertam (monomethyl fumarate) – PA can be dispensed. If a MassHealth member or • Byfavo (remimazolam) ^ – PA HSN patient is approved for COVID-19, • Cabenuva (cabotegravir/rilpivirine) – PA pharmacies must dispense up to a 14-day • Danyelza (naxitamab-gqgk) – PA supply. If a MassHealth member or HSN • Imcivree (setmelanotide) – PA patient is approved for other diagnoses, • Orladeyo (berotralstat) – PA pharmacies may dispense up to a 90-day • Phexxi (lactic acid/citric acid/potassium supply if requested by the MassHealth bitartrate vaginal gel) member, HSN patient, or prescriber as long • Riabni (rituximab-arrx) – PA as sufficient quantity remains on the • Vocabria (cabotegravir) – PA prescription to support the quantity being • Zokinvy (lonafarnib) – PA filled.” Change in PA Status Effective May 10, 2021, the PA requirements for chloroquine and hydroxychloroquine will be a. -

Wednesday, June 12, 2019 4:00Pm
Wednesday, June 12, 2019 4:00pm Oklahoma Health Care Authority 4345 N. Lincoln Blvd. Oklahoma City, OK 73105 The University of Oklahoma Health Sciences Center COLLEGE OF PHARMACY PHARMACY MANAGEMENT CONSULTANTS MEMORANDUM TO: Drug Utilization Review (DUR) Board Members FROM: Melissa Abbott, Pharm.D. SUBJECT: Packet Contents for DUR Board Meeting – June 12, 2019 DATE: June 5, 2019 Note: The DUR Board will meet at 4:00pm. The meeting will be held at 4345 N. Lincoln Blvd. Enclosed are the following items related to the June meeting. Material is arranged in order of the agenda. Call to Order Public Comment Forum Action Item – Approval of DUR Board Meeting Minutes – Appendix A Update on Medication Coverage Authorization Unit/Use of Angiotensin Converting Enzyme Inhibitor (ACEI)/ Angiotensin Receptor Blocker (ARB) Therapy in Patients with Diabetes and Hypertension (HTN) Mailing Update – Appendix B Action Item – Vote to Prior Authorize Aldurazyme® (Laronidase) and Naglazyme® (Galsulfase) – Appendix C Action Item – Vote to Prior Authorize Plenvu® [Polyethylene Glycol (PEG)-3350/Sodium Ascorbate/Sodium Sulfate/Ascorbic Acid/Sodium Chloride/Potassium Chloride] – Appendix D Action Item – Vote to Prior Authorize Consensi® (Amlodipine/Celecoxib) and Kapspargo™ Sprinkle [Metoprolol Succinate Extended-Release (ER)] – Appendix E Action Item – Vote to Update the Prior Authorization Criteria For H.P. Acthar® Gel (Repository Corticotropin Injection) – Appendix F Action Item – Vote to Prior Authorize Fulphila® (Pegfilgrastim-jmdb), Nivestym™ (Filgrastim-aafi), -

State of the Art Opioid-Sparing Strategies for Post-Operative Pain in Adult Surgical Patients
UC San Diego UC San Diego Previously Published Works Title State of the art opioid-sparing strategies for post-operative pain in adult surgical patients. Permalink https://escholarship.org/uc/item/3z9800kv Journal Expert opinion on pharmacotherapy, 20(8) ISSN 1465-6566 Authors Gabriel, Rodney A Swisher, Matthew W Sztain, Jacklynn F et al. Publication Date 2019-06-01 DOI 10.1080/14656566.2019.1583743 Peer reviewed eScholarship.org Powered by the California Digital Library University of California EXPERT OPINION ON PHARMACOTHERAPY https://doi.org/10.1080/14656566.2019.1583743 REVIEW State of the art opioid-sparing strategies for post-operative pain in adult surgical patients Rodney A. Gabriela,b,c, Matthew W. Swishera,c, Jacklynn F. Sztaina, Timothy J. Furnisha, Brian M. Ilfelda,c and Engy T. Saida aDepartment of Anesthesiology, Division of Regional Anesthesia and Acute Pain, University of California, San Diego, La Jolla, CA, USA; bDivision of Biomedical Informatics, University of California, San Diego, La Jolla, CA, USA; cOutcomes Research Consortium, Cleveland, OH, USA ABSTRACT ARTICLE HISTORY Introduction: There are various important implications associated with poorly controlled postoperative Received 17 October 2018 pain in the adult surgical patient – this includes cardiopulmonary complications, opioid-related side Accepted 13 February 2019 effects, unplanned hospital admissions, prolonged hospital stay, and the subsequent development of KEYWORDS chronic pain or opioid addiction. With the ongoing national opioid crisis, it is imperative that perio- Multimodal analgesia; acute perative providers implement pathways for surgical patients that reduce opioid requirements and pain- pain service; opioid; related complications. perioperative Areas covered: In this review, the authors discuss the components of a multimodal opioid-sparing analgesia pathway as it pertains to the perioperative environment.