To Investigate Models of Health Service Delivery to Transgender and Gender Diverse Populations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Nexus of Sex Work and Homelessness Wednesday March 6, 2019 Disclaimer
The Nexus of Sex Work and Homelessness Wednesday March 6, 2019 Disclaimer This project was supported by the Health Resources & Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number U30CS09746, a National Training and Technical Assistance Cooperative Agreement for $1,625,741, with 0% match from nongovernmental sources. This information or content and conclusions are those of the presenters and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government. NHCHC is a nonpartisan, noncommercial organization. Presenters Jonathan Santos- Ramos Director of Community Engagement & Strategic Initiatives Joanna Rivera Callen-Lorde Health Director of Transgender Center Housing New York, NY Ali Forney Center Aruna Krishnakumar, Tracee Brown LCSW Coordinator of Training Director of Health & Advocacy Outreach to Teens Pronouns: They/Them Callen-Lorde Ali Forney Center Learning Objectives Participants will be able to… • Provide introduction to the relationship between sex work and homelessness among diverse feminine-presenting communities. • Present service delivery efforts for feminine-presenting clients engaging in sex work, specifically with NYC youth. • Discuss nuances, challenges, and successes of providing care to special populations at the intersections of oppression AGENDA ▪ The Basics ▪ Defining Sex Work ▪ What is Feminine presenting/Transgender/Gender Non-Binary/Gender Non-Conforming and why is important ▪ Increases -

Current Funding
Fiscal Year 2020 Continuum of Care Competition Non-competitive Awarded Projects Report Organization Name Project or Award Name Grant Number FY2020 Amount State:Alabama CoC Number: AL-500 CoC Name: Birmingham/Jefferson, St. Clair, Shelby Counties CoC Jefferson County Housing Authority AL0013L4C001811 FY2019 AL0013L4C002013 $3,737,584 One Roof AL-500 CoC Planning Project Application AL0186L4C002000 $273,350 2020 AIDS Alabama, Inc. Ascension Project Consolidated FY2019 AL0127L4C002005 $1,035,212 One Roof Coordinated Assessment FY2019 AL0144L4C002004 $377,643 First Light, Inc. Fourth Floor 2019 AL0010L4C002013 $117,915 The Cooperative Downtown Ministries, FY 2019 Consolidated PSH AL0001L4C002013 $794,516 Inc. The Cooperative Downtown Ministries, FY 2019 Safe Haven AL0003L4C002013 $128,834 Inc. The Cooperative Downtown Ministries, FY2019 Nashamah AL0006L4C002013 $223,262 Inc. One Roof HMIS Combined Grant FY2019 AL0005L4C002013 $332,480 AIDS Alabama, Inc. Le Transclusive Project Consolidated AL0142L4C002004 $460,076 FY2019 First Light, Inc. Rapid Rehousing 2019 AL0128L4C002005 $511,398 Jefferson-Blount-St. Clair Mental Health REACT Supportive Housing FY19 AL0021L4C002013 $667,722 Authority Pathways Inc. Safe Haven Shelter FY 19 AL0011L4C002013 $142,468 Jefferson-Blount-St. Clair Mental Health Supportive Housing Program FY 19 AL0019L4C002013 $524,928 Authority Youth Towers Inc. TH/RRH Hybrid FY2019 AL0165L4C002002 $117,462 First Light, Inc. TRIO PSH Combined FY2019 AL0008L4C002013 $437,590 AIDS Alabama, Inc. Way Station TH/RRH FY2019 AL0155L4C002003 $308,281 CoC Number: AL-501 CoC Name: Mobile City & County/Baldwin County CoC State of Alabama ADMH MI-Rental Assistance Mobile based AL0040L4C012013 $259,643 project Housing First, Inc. AL-501 CoC Planning Project Application AL0187L4C012000 $113,744 2020 Organization Name Project or Award Name Grant Number FY2020 Amount Housing First, Inc. -

Download the Know Your Rights Brochure
RESOURCES KNOW YOUR RIGHTS LGBTQ Youth in Foster Care ACS LGBTQ Youth Resources HOTT (Health Outreach to Teens) – If you are having a problem in foster care or juvenile Callen-Lorde Community Health Center and Juvenile Justice Systems justice systems because of your sexual orientation, Free or low cost medical and mental health care/ gender identity, or gender expression, contact us. counseling, including physical exams, gynecological www.nyc.gov/acs/LGBTQ (212) 676-9421 exams, and STD/HIV treatment and testing to LGBTQ and homeless youth ages 13-24. Hormone therapy The Ali Forney Center available for youth ages 18-24. The nation’s largest and most comprehensive organization www.callen-lorde.org (212) 271-7200 dedicated to providing support and services for homeless LGBT youth, aged 16-24, to escape the streets and begin Hetrick-Martin Institute/Harvey Milk High School to live healthy and independent lives. The Supportive Services Department provides group, www.aliforneycenter.org (212) 206-0574 family and individual counseling for LGBT youth and families. Also offers assistance with after school programs, The Lesbian, Gay, Bisexual, and Transgender intern placement, GED assistance, peer counseling, Community Center – Center Youth/YES Program pantry and clothing. The second-largest LGBT community center in the world www.hmi.org (212) 674-2400 providing a full range of support, education, arts, and leadership programming to LGBTQ and allied youth The Trevor Project – Trevor Lifeline ages 13-21 through the Center Youth/YES program. A free and confidential hotline offering trained counselors www.gaycenter.org (212) 620-7310 available and equipped to support LGBTQ young people in crisis, feeling suicidal, or in need of a safe The Door and nonjudgmental place to talk 24/7. -

Doing Business Search - People
Doing Business Search - People MOCS PEOPLE ID ORGANIZATION NAME 50136 CASTLE SOFTWARE INC 158890 J2 147-07 94TH AVENUE LI LLC 160281 SDF67 SPRINGFIELD BLVD OWNER LLC 129906 E-J ELECTRIC INSTALLATION CO. 63414 NEOPOST USA INC 56283 MAKE THE ROAD NEW YORK 53828 BOSTON TRUST & INVESTMENT MANAGEMENT COMPANY 89181 FALCON BUILDER INC 105272 STERLING INFOSYSTEMS INC 107736 SIEGEL & STOCKMAN 160919 UTECH PRODUCTS INC 49631 LIRO GIS INC. 12881 THE GORDIAN GROUP INC. 64818 ZUCKER'S GIFTS INC 52185 JAMAICA CENTER FOR ARTS & LEARNING INC 146694 GOOD SHEPHERD SERVICES 156009 ATOMS INC. 116226 THE MENTAL HEALTH ASSOCIATION OF NEW YORK CITY INC. 150172 SOSA USA LLC Page 1 of 1464 09/26/2021 Doing Business Search - People PERSON FIRST NAME PERSON MIDDLE NAME SCOTT FRANK C NATALIE DEBORAH L LUCIA B MEHMET ANDREW PHILIPPE J JAMES J MICHAEL HARRY H MARVIN CATHY HUIYING RACHEL SIDRA SUSAN UZI B Page 2 of 1464 09/26/2021 Doing Business Search - People PERSON LAST NAME PERSON_NAME_SUFFIX FISCHER PRG NATIONAL URBAN FUNDS LLC SULLIVAN DEBT FUND HLDINGS LLC LAMBRAIA ADAIR AXT SANTINI PALAOGLU REIBEN DALLACORTE COSTANZO BAILEY MELLON STERNBERG HUNG KITAY QASIM SHANKLIN SCHEFFER Page 3 of 1464 09/26/2021 Doing Business Search - People RELATIONSHIP TYPE CODE MCT EWN EWN MCT MCT CFO OWN CFO CFO CEO MCT MCT MCT CEO CEO MCT COO COO CEO Page 4 of 1464 09/26/2021 Doing Business Search - People DOING BUSINESS START DATE 09/21/0016 11/20/0019 01/14/0020 03/10/0016 08/08/0008 04/03/0021 11/19/0008 06/02/0014 09/02/0016 03/03/0013 04/03/0021 06/02/0018 08/02/0008 12/05/0008 04/14/0015 02/22/0018 06/05/0019 03/08/0014 01/03/0020 Page 5 of 1464 09/26/2021 Doing Business Search - People DOING BUSINESS END DATE Page 6 of 1464 09/26/2021 Doing Business Search - People 65572 RUSSELL TRUST COMPANY 53596 MOHAWK LTD 68208 ST ANN'S ABH OWNER LLC 136274 NEW YORK CITY CENTER INC. -

Police Abuse and Misconduct Against Lesbian, Gay, Bisexual and Transgender People in the U.S
United States of America Stonewalled : Police abuse and misconduct against lesbian, gay, bisexual and transgender people in the U.S. 1. Introduction In August 2002, Kelly McAllister, a white transgender woman, was arrested in Sacramento, California. Sacramento County Sheriff’s deputies ordered McAllister from her truck and when she refused, she was pulled from the truck and thrown to the ground. Then, the deputies allegedly began beating her. McAllister reports that the deputies pepper-sprayed her, hog-tied her with handcuffs on her wrists and ankles, and dragged her across the hot pavement. Still hog-tied, McAllister was then placed in the back seat of the Sheriff’s patrol car. McAllister made multiple requests to use the restroom, which deputies refused, responding by stating, “That’s why we have the plastic seats in the back of the police car.” McAllister was left in the back seat until she defecated in her clothing. While being held in detention at the Sacramento County Main Jail, officers placed McAllister in a bare basement holding cell. When McAllister complained about the freezing conditions, guards reportedly threatened to strip her naked and strap her into the “restraint chair”1 as a punitive measure. Later, guards placed McAllister in a cell with a male inmate. McAllister reports that he repeatedly struck, choked and bit her, and proceeded to rape her. McAllister sought medical treatment for injuries received from the rape, including a bleeding anus. After a medical examination, she was transported back to the main jail where she was again reportedly subjected to threats of further attacks by male inmates and taunted by the Sheriff’s staff with accusations that she enjoyed being the victim of a sexual assault.2 Reportedly, McAllister attempted to commit suicide twice. -

Annual Report 2018-2019
ANNUAL REPORT 2018-2019 1 2 CONTENTS A Letter from Our Executive Director 4 A Letter from the Chair of the Board 5 Our Namesakes 6 Celebrating Our History: 50 Years of LGBTQ Health 8 Timeline 12 Reflections on our History 14-17 Our Patients 18 A Year in Photos 22 Our Staff 24 Callen-Lorde Brooklyn 26 Board of Directors 28 Senior Leadership 29 Howard J. Brown Society 30 Our Supporters 32 ABOUT US Callen-Lorde is the global leader in LGBTQ healthcare. Since the days of Stonewall, we have been transforming lives in LGBTQ communities through excellent comprehensive care, provided free of judgment and regardless of ability to pay. In addition, we are continuously pioneering research, advocacy and education to drive positive change around the world, because we believe healthcare is a human right. 3 A LETTER FROM OUR EXECUTIVE DIRECTOR Dear Friends, Supporters, and Community Members, Fifty years ago, Sylvia Rivera and Marsha P. Johnson were among the first brick throwers in the Stonewall Rebellions, igniting the fire that began – slowly – to change LGBTQ lives. That same year, the beginnings of Callen- Lorde started when two physicians opened the St. Mark’s Health Clinic to provide free healthcare services to the ‘hippies, freaks, and queers’ in the East Village. Today, that little clinic is Callen-Lorde Community Health Center - a network of health centers soon to be in three boroughs of New York City and improving LGBTQ health worldwide. What has not changed in 50 years is our commitment to serving people regardless of ability to pay, our passion for health equity and justice for our diverse LGBTQ communities and people living with HIV, and our belief that access to healthcare is a human right and not a privilege. -

Annual Report 2019 - 2020
ANNUAL REPORT 2019 - 2020 1 2 ABOUT US Callen-Lorde is the global leader in LGBTQ healthcare. Since the days of Stonewall, we have been transforming lives in LGBTQ communities through excellent comprehensive care, provided free of judgment and regardless of ability to pay. In addition, we are continuously pioneering research, advocacy and education to drive positive change around the world, because we believe healthcare is a human right. CONTENTS History and Namesakes . 4 A Letter from our Executive Director Wendy Stark . 6 A Letter from our Board Chair Lanita Ward-Jones ������������������������������������������������������������ 7 COVID-19 Impact . 8 Callen-Lorde Brooklyn ������������������������������������������������������������������������������������������������������������������������������������������������10 Advocacy & Policy ��������������������������������������������������������������������������������������������������������������������������������������������������������������10 The Keith Haring Nurse Practitioner Postgraduate Fellowship in LGBTQ+ Health ������������������������������������������������������������������������������������������������������������������������������������������������������������������������ 12 Callen-Lorde by the Numbers . 14 Senior Staff and Board of Directors ������������������������������������������������������������������������������������������������������ 16 Howard J. Brown Society . .17 John B. Montana Society �����������������������������������������������������������������������������������������������������������������������������������������17 -

Rights of Transgender Adolescents to Sex Reassignment Treatment
THE DOCTOR WON'T SEE YOU NOW: RIGHTS OF TRANSGENDER ADOLESCENTS TO SEX REASSIGNMENT TREATMENT SONJA SHIELD* I. INTRODUCTION .................................................................................................... 362 H . DEFINITIO NS ........................................................................................................ 365 III. THE HARMS SUFFERED BY TRANSGENDER ADOLESCENTS CREATE A NEED FOR EARLY TRANSITION .................................................... 367 A. DISCRIMINATION AND HARASSMENT FACED BY TRANSGENDER YOUTH .............. 367 1. School-based violence and harassment............................................................. 368 2. Discriminationby parents and thefoster care system ....................................... 372 3. Homelessness, poverty, and criminalization...................................................... 375 B. PHYSICAL AND MENTAL EFFECTS OF DELAYED TRANSITION ............................... 378 1. Puberty and physical changes ........................................................................... 378 2. M ental health issues ........................................................................................... 382 IV. MEDICAL AND PSYCHIATRIC RESPONSES TO TRANSGENDER PEOPLE ........................................................................................ 385 A. GENDER IDENTITY DISORDER TREATMENT ........................................................... 386 B. FEARS OF POST-TREATMENT REGRET ................................................................... -

Estudio Comparativo Del Impacto De La Homosexualidad En El Proceso De Envejecimiento Del Hombre Gay En Nueva York Y Madrid
TESIS DOCTORAL 2020 ESTUDIO COMPARATIVO DEL IMPACTO DE LA HOMOSEXUALIDAD EN EL PROCESO DE ENVEJECIMIENTO DEL HOMBRE GAY EN NUEVA YORK Y MADRID PROGRAMA DE DOCTORADO EN ANÁLISIS DE PROBLEMAS SOCIALES Autor: MATEO SANCHO CARDIEL Directora de Tesis: DRA. Dª VERÓNICA DÍAZ MORENO 1 Departamento de Sociología III (Tendencias Sociales) Facultad de Ciencias Políticas y Sociología de la UNED “Estudio comparativo del impacto de la homosexualidad en el proceso de envejecimiento del hombre gay en Nueva York y Madrid” Autor: Mateo Sancho Cardiel. Máster en Problemas Sociales por la UNED. Directora de la Tesis: Doctora Doña Verónica Díaz Moreno. 2 AGRADECIMIENTOS La conclusión más importante de toda tesis doctoral es que la construcción del conocimiento tiene una naturaleza necesariamente coral. Esta tesis, en concreto, no hubiese sido posible sin la asistencia, la motivación, la fe en mí y el impulso de mi marido, Nelson Núñez-Rodríguez, capaz de oscilar entre la exigencia y la comprensión. Gracias por tu paciencia y por tu solidez, que han hecho posible que no engrosáramos la amplia lista de parejas que no sobreviven al doctorado de uno de sus miembros. Gracias a mis padres, José Miguel y Celina, por haberme educado en un espacio de amor incondicional, intercambio de ideas y empatía por el otro, por haberme inculcado la importancia de la escucha. Sin esa ductilidad emocional mamada en casa, creo que hubiese sido imposible crear en tan poco tiempo el ambiente de confianza necesario para que los informantes abrieran su corazón. Me siento privilegiado por haber formado parte de un hogar que entiende las diferencias entre cuatro hermanos (gracias también Simón, Valeria y Eloísa) y en el que se fomentó la curiosidad y las pasiones como base del aprendizaje. -

I Mmmmmmmm I I Mmmmmmmmm I M I M I Mmmmmmmmmm 5A Gross Rents
OMB No. 1545-0052 Form 990-PF Return of Private Foundation I or Section 4947(a)(1) Trust Treated as Private Foundation À¾µ¼ Do not enter social security numbers on this form as it may be made public. Department of the Treasury I Internal Revenue Service Go to www.irs.gov/Form990PF for instructions and the latest information. Open to Public Inspection For calendar year 2018 or tax year beginning 02/01 , 2018, and ending 01/31 , 20 19 Name of foundation A Employer identification number SALESFORCE.COM FOUNDATION 94-3347800 Number and street (or P.O. box number if mail is not delivered to street address) Room/suite B Telephone number (see instructions) 50 FREMONT ST 300 (866) 924-0450 City or town, state or province, country, and ZIP or foreign postal code C If exemption applicatmionm ism m m m m m I pending, check here SAN FRANCISCO, CA 94105 m m I G Check all that apply: Initial return Initial return of a former public charity D 1. Foreign organizations, check here Final return Amended return 2. Foreign organizations meeting the 85% test, checkm hem rem anmd am ttamchm m m I Address change Name change computation H Check type of organization: X Section 501(c)(3) exempt private foundation E If private foundation status was terminamtedI Section 4947(a)(1) nonexempt charitable trust Other taxable private foundation under section 507(b)(1)(A), check here I Fair market value of all assets at J Accounting method: Cash X Accrual F If the foundation is in a 60-month terminmatIion end of year (from Part II, col. -
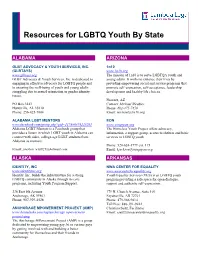
Resources for LGBTQ Youth by State
Resources for LGBTQ Youth By State ALABAMA ARIZONA GLBT ADVOCACY & YOUTH SERVICES, INC. 1n10 (GLBTAYS) www.1n10.org www.glbtays.org The mission of 1n10 is to serve LGBTQA youth and GLBT Advocacy & Youth Services, Inc. is dedicated to young adults. It works to enhance their lives by engaging in effective advocacy for LGBTQ people and providing empowering social and service programs that to ensuring the well-being of youth and young adults promote self‐expression, self‐acceptance, leadership struggling due to sexual orientation or gender identity development and healthy life choices. issues. Phoenix, AZ PO Box 3443 Contact: Michael Weakley Huntsville, AL 35810 Phone: 602-475-7456 Phone: 256-425-7804 Email: [email protected] ALABAMA LGBT MENTORS EON www.facebook.com/group.php?gid=117888378225291 www.wingspan.org Alabama LGBT Mentors is a Facebook group that The Homeless Youth Project offers advocacy, provides a forum in which LGBT youth in Alabama can information, a support group, access to shelters and basic connect with older, college-age LGBT students from services to LGBTQ youth. Alabama as mentors. Phone: 520-624-1779 ext. 115 Email: [email protected] Email: [email protected] ALASKA ARKANSAS IDENTITY, INC NWA CENTER FOR EQUALITY www.identityinc.org www.nwacenterforequality.org Identity, Inc. builds the infrastructure for a strong Youth Equality Services (YES) is an LGBTQ youth LGBTQ community in Alaska through its core program providing a safe space for open dialogue, programs, including Youth Program Support. support and -

Coat Drive Report 2016 Th Is Year, the Coat D Rive Goes Mobile
Coat Drive This year, the Report 2016 Coat Drive goes mobile. Text COAT to Just buys a new coat for a New Yorker in need. Table of Contents The Coat Drive Goes Mobile 4 Coat Drive Champions 6 Coat Drive Media and Press 8 Shifting the Coat Drive Call to Action 9 Financial Supporters 12 Collection Partners 24 Recipient Agencies 34 New York Cares York New Coat Drive Report 2016 3 The Coat Drive Goes Mobile Thanks to the generosity and compassion of “The need in our city is simply More than 1,400 companies, civic groups, and thousands of New Yorkers, New York Cares individuals also stepped up this year to deliver collected and distributed 109,213 winter coats enormous, and we developed the gently used coats through their own private during the 28th Annual Coat Drive. This year’s text option to cast a wider net collection efforts. When combined with the coats numbers broke collection records as a new mobile dropped off at our 300 public collection sites, these donation option and increased participation and engage more New Yorkers groups delivered 78,000 coats in 2016. from companies and civic groups delivered than ever. We understand that unprecedented warmth across the city. With homelessness in New York City reaching near- not everyone has an extra coat at record highs and the rising cost-of-living pushing In 2016, for the first time, New York Cares made it home to donate or can make it to more residents below the poverty line, requests possible to give a coat via a simple text message.