Pre Consultation Business Case Version
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Walking Pack Broadway Layout 1
A weekend with walks AT A GLANCE n Visit Ashmolean Museum in Broadway n Smell the lavender in Snowshill n Lovely boutique shopping n Gorgeous views from Broadway Tower n Gordon Russell Museum n Fabulous children’s play area n Visit Snowshill Manor Broadway - Breathtaking views and picturesque village Art, history, classic Cotswolds Evesham Vale (a good place to be available from Broadway Visitor and time to go shopping… during the asparagus season). St Information Centre Eadburgha’s Church is tucked away on Broadway is one of the most beautiful the Snowshill Road but worth finding. Broadway Tower and return (3 miles) Cotswold villages, situated at the The Lygon Arms Hotel was once a local although uphill all the way, this walk is Gateway to the Cotswolds (and only 2 manor house and is something of a worth the climb as the views from the hours from central London). Its wide Cotswold institution – in its time it has top are outstanding. It’s downhill on High Street lined with horse chestnut hosted both Charles I and Oliver return. trees contains a mixture of period Cromwell. houses and picturesque honey Broadway Tower circular walk coloured Cotswold stone cottages There are plenty of great places to eat (Included in the town free guide) which have lured visitors for centuries. here with a good range from higher end restaurants such as The Lygon Arms Broadway to Chipping Campden Often referred to as the 'Jewel of the and Russells to good hearty grub at see some gorgeous Cotswold Cotswolds', Broadway village lies many of the pubs and cafes. -

Charles Paget Wade
Charles Paget Wade This is Charles Paget Wade, a gentleman I came across whilst on holiday in the Cotswolds in 2014 near the picturesque village of Snowshill in Gloucestershire, which is noted for its extensive lavender fields and for its Manor which is where Charles Wade spent much of his life. Its name may be familiar to National Trust members. So what did he do and why is he of local interest? Well first let’s have a look at his family tree: Wade Family Tree As a teenager, Wade’s paternal grandfather, Solomon Abraham Wade (1806-1881), moved with his family from St Martin, an island in the north east of the West Indies archipelago to St. Kitts, about 50 miles to the south. Solomon set himself up as a merchant and by the early1860s had built a thriving business with four stores on St Kitts. Initially it was as S. A. Wade & Co and then, with a trusted employee, Samuel Abbott, he formed the partnership of Wade & Abbott. Through his business as a supplier and increasingly as an agent for the island ‘plantocracy’, Solomon gained knowledge and profits he used independent of Wade and Abbott to diversify and acquire property (including sugar cane plantations) in St Kitts and in nearby Nevis and Montserrat. His success established the fortune of the family into which Charles Wade was later born. Between 1844 and 1855 Solomon had seven children with Mary James (1817-1914), his housekeeper, who was of Afro-Caribbean descent, finally marrying in 1855. I do not have full details of the family and their birth dates but the names shown here are correct. -

THE COTSWOLDS Malvern Hills Pershore Area of Outstanding Natural Beauty Evesham
Worcester MORGAN HIRE CAR ROUTE A449 A THE COTSWOLDS Malvern Hills Pershore Area of Outstanding Natural Beauty Evesham Upton-Upon The Cotswolds covers a huge area, almost 800 square miles, Severn and runs through five counties (Gloucestershire, Oxfordshire, Warwickshire, Wiltshire and Worcestershire). One of the delights of visiting the Cotswolds is exploring the different areas, each with Broadway its own identity, yet all with those defining Cotswold features: M50 golden stone and rolling hills, the ‘wolds’. Beautiful driving roads A46 Snowshill make this stunning part of the country ideal for a top down Tewksbury #MorganAdventure. We’d loosely recommend a loop that sticks to A and B roads M5 taking in Upton-Upon-Severn, Pershore, Broadway, Snowshill, The Slaughters, Northleach, Burford and then back through Stow-On-The-Wold and Tewkesbury. The joy of the Cotswolds is Stow-on-the-Wold Town Council turning off the beaten track, exploring the quintessentially English Upper Slaughter villages of honey coloured stone, enjoying the stunning scenery Cheltenham from the cockpit of a Morgan. A424 Bourton-on-the-Water A429 POINTS OF INTEREST: Northleach A40 • Snowshill Manor and Garden - National Trust, WR12 7JU • Broadway Tower - Cotswolds Highest Tower, WR12 7LD Burford • Royal Oak, Ramsden - Good Pub Guide recommended, and an ideal lunch stop OX7 3AU M5 • Stow on The Wold - Quintessential Cotswold Town • Burford - Historic Market Town The Cotswolds An Area of Outstanding • The Slaughters - Twin villages situated near to Natural Beauty Bourton-On-The-Water • The Swan Hotel, Bibury - A former Cotswold coaching inn and an ideal lunch stop, GL7 5NW From: Malvern WR14 2LL Via: Stow-on-the-Wold & Bourton-on-the-Water To: Shipton-Under-Wychwood (and return) Distance: 103 miles Time: 2hr 56min. -

Inscriptions in the Abbey Church
The Monumental Inscriptions in the Abbey Church The earliest document to record any of the monumental inscriptions in Tewkesbury Abbey is “History in Marble” by Thomas Dingley, compiled during the reign of Charles II (1660 – 1685). This volume is in manuscript, and was published in facsimile in two volumes by the Campden Society in 1868. Tewkesbury is to be found in Volume Two. In 1750 Ralph Bigland commenced his monumental work “Historical, Monumental and Genealogical Collections relative to the County of Gloucestershire”. This recorded the monumental inscriptions in most of the parish churches in Gloucestershire, but by the time of Bigland’s death in 1784, none of his work had been published. His son and two colleagues continued his work, and it was published in instalments between 1791 and 1899. They visited Tewkesbury during Scott’s work of restoration (1875 – 1879), but were unable to check the inscriptions on the stones in the floor of the nave as it was “entirely covered with Matting and Chairs”. They make the comment that “In the course of this Work [of restoration] much of the flagging has been removed in the Choir, Transepts and Chancel, and thus the means of verifying Bigland’s account of the flat stone Inscriptions taken away”. They also refer to a Notice for a Faculty regarding the removal and re-erection of monuments, and the placing of upright head stones flat on the ground. This citation, which is in the Gloucestershire Archives, is dated 30 th April 1878, and was affixed to the door of the church on 5 th May 1878. -

Evesham, Worcestershire
FOR YOU AND 60,000 READERS ACROSS THE COTSWOLDS & VALE FREE Cotswold & & INDEPENDENT valeAUGUST 2020 Issue No. 242 magazine NO LOOKING BACK Nostalgia rules Oh no it doesn't, says our Rob Future proof Keeping our fruit heritage alive Looking ahead Students share their hopes for the future Thanks for those doorstep claps Paramedic Joann explains why they were so very important LOCAL WALKS • EATING OUT • MOTORING • PROPERTY • GARDENING • LEISURETIME • HEALTH & BEAUTY • BUSINESS and more! www.tomcookcarpets.co.uk TOM COOK OPENING HOURS Monday-Friday 9am - 5pm Saturday 9am - 2pm CARPETS t: 01386 833766 WE’RE Re-fresh Your Home with BACK fabulous NEW Flooring OPEN! - DOMESTIC & COMMERCIAL - Exciting NEW We’re proud to have Ranges NOW IN been awarded High Level of Customer Satisfaction CARPETS • VINYLS • LAMINATES A great range of flooring for your home or office... to suit all budgets! CALL IN AT OUR BLACKMINSTER SHOWROOM BLACKMINSTER BUSINESS PARK, BLACKMINSTER, EVESHAM, WORCESTERSHIRE. WR11 7RE Vale Magazine 2 THE INDEPENDENT THE BATHROOM BATHROOM STUDIO EVESHAM LTD SPECIALIST design installation supply only retail supply only trade contract specialist VISIT THE SHOWROOM - OPEN Mon to Fri 8am-5pm. Sat 9am-5pm Unit 2, Evesham Trade Centre, St Richards Road, Evesham. WR11 1XG Tel: 01386 47234 www.the-bathroomstudio.co.uk OPEN: Monday to Friday 8.30am-5pm. Saturday 9am-5pm www.the-flooringstudio.co.uk Vale Magazine 3 THANKS a million for all of your kind messages DOMESTIC & COMMERCIAL welcoming our first post lockdown magazine back into your homes and businesses. It’s great to be with you again. TARMAC It’s also wonderful to see so many of the area’s businesses up and running again. -

Autumn 2019 FREE Please Take One
the Autumn 2019 FREE Please Take One The magazine of the Gloucestershire Branches of the Campaign for Real Ale Front cover photograph competition sponsored by THE KING THE SOARING OF PALE SUMMIT OF the ALES HOPPINESS The magazine of the Gloucestershire Branches of the Campaign for Real Ale ©The Campaign for Real Ale 2019. Opinions expressed need not represent those of CAMRA Ltd or its officials HILLSIDE BREWERY FRONT COVER COMPETITION WINNER: On the edge of the Forest and thebanks of the mighty River Severn, Westbury on Severn’s very own Lyon Inn. Photograph by Stephanie Leibbrandt. THE BEER THAT contents: SCREAMS THE SUPERIOR Letters to the Editor page 4 25 Years of Goffs page 34 ‘SUMMER!’ NAME IN PREMIUM The Hunter’s Column page 8 Hillside Front Cover Comp. page 37 REAL ALE Cheltenham News page 10 View from the Brewhouse page 38 North Cotswolds News page 16 The New Inn - Willersey page 40 Cheltenham News page 14 Bushel+Peck - Cider & Perry page 42 Cirencester Beer Festival page 18 Real Ale Ramble page 44 The Ups and Downs of Exeter page 21 Seven Tuns - Birthday Party page 46 News from Gloucester page 23 Dodgy Ticker - Naming of Beers page 48 Pub News page 24 The Woolpack in Slad page 52 Stroud Summer Pub Focus page 28 Gloucester Prize Wordsearch page 57 Competition - Name that Pub page 31 What’s Coming Up? page 60 Brewery News page 32 CAMRA contacts page 62 THE SMOOTHEST, THE WISE CHOICE SILKIEST OF OF CLASSIC CONTRIBUTION DEADLINES: STOUTS CASK ALE these have now changed to SECOND FRIDAY OF FEBRUARY, MAY, AUGUST AND NOVEMBER We value feedback and news from around the county, so, if you’ve got something to say, want to make a contribution, compliment or criticise, then get in touch: The Editor, The Tippler, 23 Theocs Close, Tewkesbury, Glos. -
Liable from Property Referenceaccount Name 01/04/2000
Liable From Property referenceAccount name 01/04/2000 5050003056030 MR C M WARREN 07/07/2012 5050068207001 MR LUKE MARTIN COLE 01/04/2000 5089200046000 01/04/2003 5042051129001 TIMEFORE LTD 29/01/2012 5089131172030 MR IAN WOODWARD 01/04/2000 5049008036000 MESSRS DE HUDSON & G MATTHEWS 01/04/2003 503405203400B RAY & JULIE DAWN KIRBY 01/04/2000 5034002001000 MRS M K DARBY 01/04/2000 5021005039000 MR PETER FOULDS 01/04/2000 5021007071000 MR K D CASTLE 01/04/2000 5001008024000 DRAKES BROUGHTON VILLAGE HALL 01/04/2008 5074022102020 LISA WHELAN 01/04/2008 5074022102010 MR PAUL TURNER 01/04/2000 5095110107000 01/04/2000 5050343005000 MR JAMES BOMFORD 01/04/2000 5065014021000 MR R F COTTRILL 01/04/2000 5007001005000 MR CLIVE EDWARDS 01/04/2000 5051003051000 MR ANTHONY HAYNES 01/04/2000 5034052045000 DROITWICH GOLF & C CLUB LTD 01/04/2000 5042014051000 MR R HANNON 01/04/2000 5073002060000 MR MICHAEL J TAYLOR 01/04/2000 5021035045000 MISS S D WELLS 01/04/2000 5089001136000 MRS MARY SUTTON 01/04/2015 5050003014080 MR A G BURNEY & 01/01/2006 5095222999030 MR TIMOTHY JAMES GITTINS & 27/07/2002 503406200500A MR CHRISTOPHER STEPHEN DONNE 18/06/2007 50953830130A0 MR GEOFF BROWNE 01/04/2000 5050223040000 MR A H EAKETTS 06/03/2018 5050098050140 WYCHAVON DISTRICT COUNCIL 07/09/2013 505400105909B MR ROBERT D FARR 31/03/2016 5083008074010 WAKERING ENGINEERING LTD 01/04/2000 5082015058000 17/11/2003 506503600700A MR DEREK RIDGE 10/01/2018 5050018021000 NATIONAL OFFENDER MANAGEMENT 20/05/2015 5054026027040 BECKFORD SOCIAL CLUB 01/04/2000 5050249016000 L M STANBRA -

Economic Development and Tourism Strategy 2017-21
Economic development and tourism Strategy 2017-2021 April 2017 Economic development and tourism strategy Tewkesbury Borough Council’s future focus for economic development and tourism will be on: 1 Employment land planning. 2 Transport infrastructure improvement. 3 Business growth support. 4 Promoting Tewkesbury Borough. The Borough Council intends 5 Employability, education and training. to work closely with the business community and its partners... to deliver and monitor this work. Economic development and tourism strategy Introduction Background to the strategy The purpose of this strategy is to set the priorities within which the Borough Council will deliver and support The current Economic Development and economic development and tourism over Tourism Strategy ‘Regenerating and the next four years. This is based on Growing the Economy,’ has come to the research, consultation and identified need end of its life and in order to reflect the from within the local business community changing nature of the local economy and and partner organisations. the impact on businesses, the council has developed a new strategy. The strategy outlines how the council will help promote a strong and diverse local A clear focus on economic growth has economy, support business growth, inform emerged through the government’s spatial planning strategy, support National Growth Policy and regeneration, encourage inward Gloucestershire’s Strategic Economic Plan investment and maximise visitor numbers (SEP). The borough has also been to the area. identified as a key area for growth in the county, in terms of both housing, It sets out the Borough Council’s employment and associated facilities and objectives and priorities and a series of it’s important the new Strategy supports actions to be delivered through an annual this within its priorities. -

Land at Snowshill Broadway, Worcestershire
Land at Snowshill, Gloucestershire © Crown copyright 2016 Licence Number 100020449 Land at Snowshill Broadway, Worcestershire Ordnance Survey © Crown Copyright 2016. All rights reserved. Licence number 100022432. Plotted Scale - 1:6000 Land at Snowshill, Description General VAT: Is not payable on the purchase price but The land at Snowshill comprises one field parcel Method of Sale and Tenure: The Land at in the event where VAT is or becomes payable Broadway, Worcestershire of excellent quality free draining arable land and Snowshill is offered for sale as a whole by in respect of the property the purchaser will be WR12 7JT is currently cropped as part of a spring cropping private treaty with vacant possession upon responsible for the full amount due. All enquiries rotation. The soil has been enriched with completion as of 29th September 2016 or upon are welcome and terms to be negotiated. 12 years of pasture grazed by livestock before removal of the current growing crop at harvest Viewing: Strictly by arrangement. Given the 70 acres (28.33 hectares) being returned to arable. (whichever is the earlier). potential hazards of a working farm we ask you of arable land for sale on According to the Land Classification Maps Basic Payment Scheme Entitlements: The to be as vigilant as possible when making your the outskirts of Snowshill produced by DEFRA, the land is classified land will be sold with the inclusion of the Basic inspection for your own personal safety. as Grade 3 to Grade 4. The soil is shallow Payment Entitlement and transfer of these to the by private treaty as a whole. -
An Atmospheric Cotswold Stone Building, the Lygon Arms Dates
Broadway, Cotswolds Overview: An atmospheric Cotswold stone building, The Lygon Arms dates • 78 bedrooms including 7 suites • Free parking on-site for up to 100 cars from the 16th Century, and blends • Dine in the Great Hall or Luke’s Broadway unique period charm with the finest • Award-winning spa contemporary comforts. • Indoor pool with retractable roof • Beauty treatment rooms In the heart of Broadway, a picture- • Birmingham International Airport 39 miles postcard village at the foot of the • Evesham Railway Station 6.5 miles Cotswolds, The Lygon Arms is surrounded by some of England’s most spectacular countryside, and within easy reach of Stratford-upon- Avon, Cheltenham and Oxford. Contact Central Reservations on 0800 652 8413 or visit thehotelcollection.co.uk Bedrooms Local attractions Total bedrooms 78 Singles 2 Snowshill Manor & Garden How far: 2.4 miles Location of singles First floor Snowshill, Nr Broadway, Gloucestershire, WR12 7JU Ground floor rooms and lifts A typical Cotswold manor house, Snowshill was bought in 1919 by Charles Wade. True to his family motto, ‘Let nothing perish’, Mr Wade spent much of his life, How many ground floor rooms? 15 and most of his considerable inherited fortune, amassing a spectacular collection of everyday and extraordinary objects from across the globe. Laid out theatrically Distance from reception 100 metres according to Mr Wade’s wishes, the Manor is literally packed to the rafters with Does the hotel have a lift? No over 22,000 items, from tiny toys to splendid suits of Samurai armour. The Manor is surrounded by an intriguing terraced hillside garden designed in the Arts & Crafts style. -
2018/19 Annual Report and Accounts of the National Trust
National Trust Annual Report 2018/19 National Trust Annual Report 2018/19 1 The National Trust in brief Our purpose To look after special places throughout England, Wales and Northern Ireland for ever, for everyone. About us The charity was founded in 1895 by three people who understood the importance of our nation’s heritage and open spaces and wanted to protect them for everyone to enjoy. Almost 125 years later, their vision is still at the heart of everything we do. Through our strategy,Playing our part, we look after coastline, forests, woods, fens, beaches, farmland, moorland, islands, archaeological remains, nature reserves, villages, historic houses, gardens, mills and pubs. We restore them, protect them and make them accessible. We welcome everyone to explore: • 780 miles of coastline • 248,000 hectares of land • Over 500 historic houses, castles, ancient monuments, gardens and parks and nature reserves Most of our property is held inalienably, so it cannot be sold or developed without the consent of Parliament. Many of our properties are unable to fund their own permanent preservation. The cost of caring for them is high: our overall conservation expenditure on property projects, conservation repairs and conservation of contents was £148.4 million in 2018/19 (see page 50). We rely on the support of our members, donors, volunteers and grant-making bodies, as well as income from commercial activities such as retail and catering, to look after the places in our care. This Annual Report can also be viewed online at www.nationaltrustannualreport.org.uk A 2018/19 Impact Review is also available at www.nationaltrust.org.uk/features/annual-reports. -
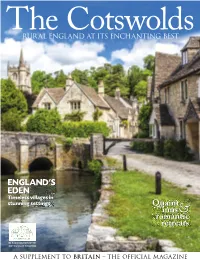
Cotswolds Britain Guide
TheRURAL ENGLAND Cotswolds AT ITS ENCHANTING BEST ENGLAND'S EDEN Timeless villages in stunning settings Quaint inns romantic& retreats IN ASSOCIATION WITH COTSWOLDS TOURISM A SUPPLEMENT TO BRITAIN THE OFFICIAL MAGAZINE cover .indd 1 21/11/2018 10:10 Britain’s Greatest Palace Birthplace of Sir Winston Churchill WORLD HERITAGE SITE Buy one day get 12 months free* blenheimpalace.com *Terms and conditions apply BP_210x297_GROUPS_ADVERT.indd 1 09/11/2018 16:35 Welcome e Cotswolds: a dreamy, lost-in-time landscape of honey-stone villages nestled in rolling hills. is very English region is so famous for its small-scale architecture that many imagine it as a small cluster of villages. In fact, those famous ‘wolds’ (hills) cover nearly 800 miles and span ve counties (Gloucestershire, Wiltshire, Oxfordshire, Warwickshire and Worcestershire). Must-sees abound. Over the next 32 pages, we cherry-pick the 4 highlights: picture-perfect villages built in the local creamy stone, 4 stately homes to swoon over, and PRETTIEST VILLAGES special places to stay: for a real Our pick of the Cotswolds' loveliest corners avour of the Cotswolds, it has to be a c o s y i n n o r g r a n d c o u n t r y h o u s e . Finally, these lovely landscapes 12 haven’t escaped the attention of CASTLES & MANORS From Jacobean manors to Tudor lmmakers. We’ve tracked down castles, visit the area's most some of the locations you might just stunning stately homes recognize – yet more places to add to your must-visit list.