Australians Take Sides on the Right to Die
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
'Landscapes of Exploration' Education Pack
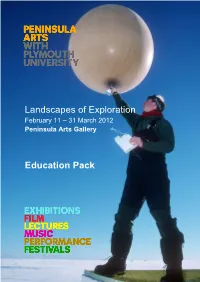
Landscapes of Exploration February 11 – 31 March 2012 Peninsula Arts Gallery Education Pack Cover image courtesy of British Antarctic Survey Cover image: Launch of a radiosonde meteorological balloon by a scientist/meteorologist at Halley Research Station. Atmospheric scientists at Rothera and Halley Research Stations collect data about the atmosphere above Antarctica this is done by launching radiosonde meteorological balloons which have small sensors and a transmitter attached to them. The balloons are filled with helium and so rise high into the Antarctic atmosphere sampling the air and transmitting the data back to the station far below. A radiosonde meteorological balloon holds an impressive 2,000 litres of helium, giving it enough lift to climb for up to two hours. Helium is lighter than air and so causes the balloon to rise rapidly through the atmosphere, while the instruments beneath it sample all the required data and transmit the information back to the surface. - Permissions for information on radiosonde meteorological balloons kindly provided by British Antarctic Survey. For a full activity sheet on how scientists collect data from the air in Antarctica please visit the Discovering Antarctica website www.discoveringantarctica.org.uk and select resources www.discoveringantarctica.org.uk has been developed jointly by the Royal Geographical Society, with IBG0 and the British Antarctic Survey, with funding from the Foreign and Commonwealth Office. The Royal Geographical Society (with IBG) supports geography in universities and schools, through expeditions and fieldwork and with the public and policy makers. Full details about the Society’s work, and how you can become a member, is available on www.rgs.org All activities in this handbook that are from www.discoveringantarctica.org.uk will be clearly identified. -

Agenda 0945 Welcome Explaining the Rule of Law and Its Elements Using the Rule of Session 1: Law Pyramid
17/09/2017 WELCOME TO THE “RULE OF LAW EXPOSED” PROFESSIONAL LEARNING SEMINAR Agenda 0945 Welcome Explaining the rule of law and its elements using the rule of Session 1: law pyramid. 1015 Session 2: Explore contemporary examples, especially Racial Discrimination and Freedom of Speech. 1100 Session 3: Promoting student engagement in Years 7-10 RoLI resources and Q&A. 1125 Session 4: Teaching & Learning approaches to help understand rule of law in contexts suitable to students of both Civics & Citizenship and Politics & Law ATAR. 1145 Conclusion Q&A or WACE Student Revision Seminar for Politics & Law 1 17/09/2017 RULE OF LAW EXPOSED BY JACKIE CHARLES Please see the separate document which contains the presentation 2 17/09/2017 TEACHING & LEARNING STRATEGIES FOR CIVICS & CITIZENSHIP AS WELL AS POLITICS & LAW CIVICS & CITIZENSHIP CURRICULUM Year 7 Civics & Citizenship: the purpose and value of the Australian Constitution; the concept of the separation of powers between the legislature, executive and judiciary and how it seeks to prevent the excessive concentration of power; how Australia’s legal system aims to provide justice, including through the rule of law, presumption of innocence, burden of proof, right to a fair trial, and right to legal representation; Year 9 Civics & Citizenship: the key principles of Australia’s justice system, including equality before the law, independent judiciary, and right of appeal; Year 10 Civics & Citizenship: the role of the High Court, including interpreting the Constitution; the international agreements -

The Morality and Political Antagonisms of Neoliberal Discourse: Campbell Brown and the Corporatization of Educational Justice
International Journal of Communication 11(2017), 3030–3050 1932–8036/20170005 The Morality and Political Antagonisms of Neoliberal Discourse: Campbell Brown and the Corporatization of Educational Justice LEON A. SALTER1 SEAN PHELAN Massey University, New Zealand Neoliberalism is routinely criticized for its moral indifference, especially concerning the social application of moral objectives. Yet it also presupposes a particular moral code, where acting on the assumption of individual autonomy becomes the basis of a shared moral-political praxis. Using a discourse theoretical approach, this article explores different articulations of morality in neoliberal discourse. We focus on the case of Campbell Brown, the former CNN anchor who reinvented herself from 2012 to 2016 as a prominent charter school advocate and antagonist of teachers unions. We examine the ideological significance of a campaigning strategy that coheres around an image of the moral superiority of corporatized schooling against an antithetical representation of the moral degeneracy of America’s public schools system. In particular, we highlight how Brown attempts to incorporate the fragments of different progressive discourses into a neoliberalized vision of educational justice. Keywords: neoliberalism, discourse, media, public education, charter schools, unions Neoliberalism is routinely criticized for its moral indifference, especially concerning the social application of moral objectives. Davies (2014) suggests that “neoliberalism has sought to eliminate normative judgment from public life to the greatest possible extent” (p. 8) by subordinating ethical concerns to putatively objective market measures. Hay (2007) ties neoliberalism to discourses that disparage the notion of the common good, because of the axiomatic rational choice assumption that the pursuit of self- interest is the only meaningful diagnostic of human action. -

The Morality and Political Antagonisms of Neoliberal Discourse: Campbell Brown and the Corporatization of Educational Justice
International Journal of Communication 11(2017), 3030–3050 1932–8036/20170005 The Morality and Political Antagonisms of Neoliberal Discourse: Campbell Brown and the Corporatization of Educational Justice LEON A. SALTER1 SEAN PHELAN Massey University, New Zealand Neoliberalism is routinely criticized for its moral indifference, especially concerning the social application of moral objectives. Yet it also presupposes a particular moral code, where acting on the assumption of individual autonomy becomes the basis of a shared moral-political praxis. Using a discourse theoretical approach, this article explores different articulations of morality in neoliberal discourse. We focus on the case of Campbell Brown, the former CNN anchor who reinvented herself from 2012 to 2016 as a prominent charter school advocate and antagonist of teachers unions. We examine the ideological significance of a campaigning strategy that coheres around an image of the moral superiority of corporatized schooling against an antithetical representation of the moral degeneracy of America’s public schools system. In particular, we highlight how Brown attempts to incorporate the fragments of different progressive discourses into a neoliberalized vision of educational justice. Keywords: neoliberalism, discourse, media, public education, charter schools, unions Neoliberalism is routinely criticized for its moral indifference, especially concerning the social application of moral objectives. Davies (2014) suggests that “neoliberalism has sought to eliminate normative judgment from public life to the greatest possible extent” (p. 8) by subordinating ethical concerns to putatively objective market measures. Hay (2007) ties neoliberalism to discourses that disparage the notion of the common good, because of the axiomatic rational choice assumption that the pursuit of self- interest is the only meaningful diagnostic of human action. -

The South Polar Race Medal
The South Polar Race Medal Created by Danuta Solowiej The way to the South Pole / Sydpolen. Roald Amundsen’s track is in Red and Captain Scott’s track is in Green. The South Polar Race Medal Roald Amundsen and his team reaching the Sydpolen on 14 Desember 1911. (Obverse) Captain R. F. Scott, RN and his team reaching the South Pole on 17 January 1912. (Reverse) Created by Danuta Solowiej Published by Sim Comfort Associates 29 March 2012 Background The 100th anniversary of man’s first attainment of the South Pole recalls a story of two iron-willed explorers committed to their final race for the ultimate prize, which resulted in both triumph and tragedy. In July 1895, the International Geographical Congress met in Lon- don and opened Antarctica’s portal by deciding that the southern- most continent would become the primary focus of new explora- tion. Indeed, Antarctica is the only such land mass in our world where man has ventured and not found man. Up until that time, no one had explored the hinterland of the frozen continent, and even the vast majority of its coastline was still unknown. The meet- ing touched off a flurry of activity, and soon thereafter national expeditions and private ventures started organizing: the Heroic Age of Antarctic Exploration had begun, and the attainment of the South Pole became the pinnacle of that age. Roald Engelbregt Gravning Amundsen (1872-1928) nurtured at an early age a strong desire to be an explorer in his snowy Norwegian surroundings, and later sailed on an Arctic sealing voyage. -

Don't Blame the Unemployed
Journal & Proceedings of the Royal Society of New South Wales, vol. 150, part 1, 2017, pp. 3–8. ISSN 0035-9173/17/010003-06 Don’t Blame the Unemployed Peter Baume AC DistFRSN Distinguished Fellow’s Lecture Annual Dinner of the Royal Society of New South Wales, The Union, University and Schools Club 25 Bent St, Sydney, 3 May, 2017 Professor Baume studied medicine at the University of Sydney, General Hospital, Birmingham, and as a U.S. Public Health Service Fellow in Nashville, Tennessee. He practiced as a gastroenterologist and physician in Australia from 1967 to 1974 and received his M.D. from the University of Sydney during that time. From 1974 to 1991 he served as a Senator for New South Wales. He held a number of portfolios, including Aboriginal Affairs, Health, and Education, and was a member of Cabinet. From 1991 to 2000, Professor Baume was Professor of Community Medicine at the University of N.S.W. He was on the Council of the Australian National University from 1986 to 2006 and was Chancellor of A.N.U. from 1994 to 2006. He has also been Commissioner of the Australian Law Reform Commission, Deputy Chair of the Australian National Council on AIDS, and Foundation Chair of the Australian Sports Anti-Doping Authority. id you know that the good food you photography? You are thoughtful and dis- Dhave just eaten demands a quarter of all tinguished and contributing to society. your blood for digestion and absorption, and Let me put one — just one — serious this can lead to anyone becoming somno- proposition to you to start. -

Durkheim and Organizational Culture
IRLE IRLE WORKING PAPER #108-04 June 2004 Durkheim and Organizational Culture James R. Lincoln and Didier Guillot Cite as: James R. Lincoln and Didier Guillot. (2004). “Durkheim and Organizational Culture.” IRLE Working Paper No. 108-04. http://irle.berkeley.edu/workingpapers/108-04.pdf irle.berkeley.edu/workingpapers Durkheim and Organizational Culture James R. Lincoln Walter A. Haas School of Business University of California Berkeley, CA 94720 Didier Guillot INSEAD Singapore June , 2004 Prepared for inclusion in Marek Kocsynski, Randy Hodson, and Paul Edwards (editors): Social Theory at Work . Oxford, UK: Oxford University Press. Durkheim and Organizational Culture “The degree of consensus over, and intensity of, cognitive orientations and regulative cultural codes among the members of a population is an inv erse function of the degree of structural differentiation among actors in this population and a positive, multiplicative function of their (a) rate of interpersonal interaction, (b) level of emotional arousal, and (c) rate of ritual performance. ” Durkheim’ s theory of culture as rendered axiomatically by Jonathan Turner (1990) Introduction This paper examines the significance of Emile Durkheim’s thought for organization theory , particular attention being given to the concept of organizational culture. We ar e not the first to take the project on —a number of scholars have usefully addressed the extent and relevance of this giant of Western social science for the study of organization and work. Even so, there is no denying that Durkheim’s name appears with vast ly less frequency in the literature on these topics than is true of Marx and W eber, sociology’ s other founding fathers . -

Report X Terminology Xi Acknowledgments Xii
Senate Legal and Constitutional Legislation Committee Consideration of Legislation Referred to the Committee Euthanasia Laws Bill 1996 March 1997 The Parliament of the Commonwealth of Australia Senate Legal and Constitutional Legislation Committee Consideration of Legislation Referred to the Committee Euthanasia Laws Bill 1996 March 1997 © Commonwealth of Australia 1997 ISSN 1326-9364 This document was produced from camera-ready copy prepared by the Senate Legal and Constitutional Legislation Committee, and printed by the Senate Printing Unit, Department of the Senate, Parliament House, Canberra. Members of the Legislation Committee Members Senator E Abetz, Tasmania, Chair (Chair from 3 March 1997) Senator J McKiernan, Western Australia, Deputy Chair Senator the Hon N Bolkus, South Australia Senator H Coonan, New South Wales (from 26 February 1997: previously a Participating Member) Senator V Bourne, New South Wales (to 3 March 1997) Senator A Murray, Western Australia (from 3 March 1997) Senator W O’Chee, Queensland Participating Members All members of the Opposition: and Senator B Brown, Tasmania Senator M Colston, Queensland Senator the Hon C Ellison, Western Australia (from 26 February 1997: previously the Chair) Senator J Ferris, South Australia Senator B Harradine, Tasmania Senator W Heffernan, New South Wales Senator D Margetts, Western Australia Senator J McGauran, Victoria Senator the Hon N Minchin, South Australia Senator the Hon G Tambling, Northern Territory Senator J Woodley, Queensland Secretariat Mr Neil Bessell (Secretary -

Antarctica: Music, Sounds and Cultural Connections
Antarctica Music, sounds and cultural connections Antarctica Music, sounds and cultural connections Edited by Bernadette Hince, Rupert Summerson and Arnan Wiesel Published by ANU Press The Australian National University Acton ACT 2601, Australia Email: [email protected] This title is also available online at http://press.anu.edu.au National Library of Australia Cataloguing-in-Publication entry Title: Antarctica - music, sounds and cultural connections / edited by Bernadette Hince, Rupert Summerson, Arnan Wiesel. ISBN: 9781925022285 (paperback) 9781925022292 (ebook) Subjects: Australasian Antarctic Expedition (1911-1914)--Centennial celebrations, etc. Music festivals--Australian Capital Territory--Canberra. Antarctica--Discovery and exploration--Australian--Congresses. Antarctica--Songs and music--Congresses. Other Creators/Contributors: Hince, B. (Bernadette), editor. Summerson, Rupert, editor. Wiesel, Arnan, editor. Australian National University School of Music. Antarctica - music, sounds and cultural connections (2011 : Australian National University). Dewey Number: 780.789471 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying or otherwise, without the prior permission of the publisher. Cover design and layout by ANU Press Cover photo: Moonrise over Fram Bank, Antarctica. Photographer: Steve Nicol © Printed by Griffin Press This edition © 2015 ANU Press Contents Preface: Music and Antarctica . ix Arnan Wiesel Introduction: Listening to Antarctica . 1 Tom Griffiths Mawson’s musings and Morse code: Antarctic silence at the end of the ‘Heroic Era’, and how it was lost . 15 Mark Pharaoh Thulia: a Tale of the Antarctic (1843): The earliest Antarctic poem and its musical setting . 23 Elizabeth Truswell Nankyoku no kyoku: The cultural life of the Shirase Antarctic Expedition 1910–12 . -

Talking to Judges About the Art of Judging: an Annotated Performance Text
TALKING TO JUDGES ABOUT THE ART OF JUDGING: AN ANNOTATED PERFORMANCE TEXT Greta Bird and Nicole Rogers* [We performed this paper at the Judicial Reasoning: Art or Science? conference held at the Australian National University in February 2009. We were performing on at least two levels: as academics and editors of a collection of judicially-authored essays on the art of judging but also, as we proclaimed at the outset, as Jester and Fool. We did not appear in costume as jesters or fools. We did not even appear as fairies, although one of us is well-known at Southern Cross University for donning fairy wings and fairy tales featured in this performance (as did sheep, land rights and playfulness). But then, our audience of judges had also left their costumes behind; there were no wigs or robes. They were in civilian clothes, recognisable only as judges through name tags. They were, in fact, unmasked. Greta began by acknowledging the traditional custodians of the land. Nicole then spoke. The accompanying slide portrays a fool, colourfully clad, balanced lightly and without any apparent concern at the edge of a precipice, and a jester in classic costume.] Our focus is on judging as performance and judging as playfulness. We write as outsiders, in the guise of the Jester and the Fool: playful figures who are outside the law. Brian Sutton-Smith argues that the Fool ‘live[s] in the place where the “writ does not run”’.1 We are also influenced, however, by our role as editors of a recent collection of articles on the art of judging. -

Ministerial Staff Under the Howard Government: Problem, Solution Or Black Hole?
Ministerial Staff Under the Howard Government: Problem, Solution or Black Hole? Author Tiernan, Anne-Maree Published 2005 Thesis Type Thesis (PhD Doctorate) School Department of Politics and Public Policy DOI https://doi.org/10.25904/1912/3587 Copyright Statement The author owns the copyright in this thesis, unless stated otherwise. Downloaded from http://hdl.handle.net/10072/367746 Griffith Research Online https://research-repository.griffith.edu.au Ministerial Staff under the Howard Government: Problem, Solution or Black Hole? Anne-Maree Tiernan BA (Australian National University) BComm (Hons) (Griffith University) Department of Politics and Public Policy, Griffith University Submitted in fulfilment of the requirements of the degree of Doctor of Philosophy November 2004 Abstract This thesis traces the development of the ministerial staffing system in Australian Commonwealth government from 1972 to the present. It explores four aspects of its contemporary operations that are potentially problematic. These are: the accountability of ministerial staff, their conduct and behaviour, the adequacy of current arrangements for managing and controlling the staff, and their fit within a Westminster-style political system. In the thirty years since its formal introduction by the Whitlam government, the ministerial staffing system has evolved to become a powerful new political institution within the Australian core executive. Its growing importance is reflected in the significant growth in ministerial staff numbers, in their increasing seniority and status, and in the progressive expansion of their role and influence. There is now broad acceptance that ministerial staff play necessary and legitimate roles, assisting overloaded ministers to cope with the unrelenting demands of their jobs. However, recent controversies involving ministerial staff indicate that concerns persist about their accountability, about their role and conduct, and about their impact on the system of advice and support to ministers and prime ministers. -

Herbert Ponting; Picturing the Great White South
City University of New York (CUNY) CUNY Academic Works Dissertations and Theses City College of New York 2014 Herbert Ponting; Picturing the Great White South Maggie Downing CUNY City College How does access to this work benefit ou?y Let us know! More information about this work at: https://academicworks.cuny.edu/cc_etds_theses/328 Discover additional works at: https://academicworks.cuny.edu This work is made publicly available by the City University of New York (CUNY). Contact: [email protected] The City College of New York Herbert Ponting: Picturing the Great White South Submitted in partial fulfillment of the requirements for the degree of Master of Arts of the City College of the City University of New York. by Maggie Downing New York, New York May 2014 Dedicated to my Mother Acknowledgments I wish to thank, first and foremost my advisor and mentor, Prof. Ellen Handy. This thesis would never have been possible without her continuing support and guidance throughout my career at City College, and her patience and dedication during the writing process. I would also like to thank the rest of my thesis committee, Prof. Lise Kjaer and Prof. Craig Houser for their ongoing support and advice. This thesis was made possible with the assistance of everyone who was a part of the Connor Study Abroad Fellowship committee, which allowed me to travel abroad to the Scott Polar Research Institute in Cambridge, UK. Special thanks goes to Moe Liu- D'Albero, Director of Budget and Operations for the Division of the Humanities and the Arts, who worked the bureaucratic college award system to get the funds to me in time.