Prokinetics for the Treatment of Functional Dyspepsia: Bayesian
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Real World Efficacy and Tolerability of Acotiamide, in Relieving Meal
testinal & in D o i tr g s e Journal of Gastrointestinal & a s t G i v f e o Narayanan et al., J Gastrointest Dig Syst 2018, 8:1 S l y a s n r ISSN: 2161-069Xt Digestive System DOI: 10.4172/2161-069X.1000553 e u m o J Research Article Open Access Real World Efficacy and Tolerability of Acotiamide, in Relieving Meal- related Symptoms of Functional Dyspepsia Varsha Narayanan*, Amit Bhargava and Shailesh Pallewar 1Department of Medical Services and Research, Lupin Ltd., India *Corresponding author: Narayanan V, Department of Medical Services and Research, Lupin Ltd., Mumbai, India, Tel: +912266402222; E-mail: [email protected] Received date: February 09, 2018; Accepted date: February 21, 2018; Published date: February 27, 2018 Copyright: © 2018 Narayanan V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Background: Functional Dyspepsia (FD) is a highly prevalent clinical condition that imposes negative economic burden on health-care system as well as greatly impairs quality of life. Treatment of non-specific and bothersome meal-related FD symptoms like post-prandial fullness, upper abdominal bloating and early satiety, is a therapeutic challenge for the clinicians as poorly-defined and ill-understood pathogenesis has hampered efforts to develop effective treatments. Acotiamide is first-in-class drug that exerts its gastro-kinetic effect by enhancing acetylcholine release. Though evidence of its efficacy and tolerance are available through randomized clinical trials, real world data from its regular in-clinic use is lacking. -

PN0496-Acotiamide.Pdf
Acotiamide hydrochloride hydrate (Acofide®) 盐酸阿考替胺 Z-338 in Zeria; YM-443 in Astellas Tablet, oral, EQ 100 mg acotiamide Acotiamide is a peripheral acetylcholinesterase inhibitor, indicated for the treatment of functional dyspepsia (FD), which was first-in-class drug to treat FD in the world and approved in 2013 by Japan PMDA. It was originally discovered by Zeria, and co-developed with Astellas. The drug is co-marketing in Japan with a single brand name. The human recommended starting dose is 100 mg at a time, and 3 times a day before meals. Worldwide Key Approvals Global Sales ($Million) Key Substance Patent Expiration 2016-May (US5981557A) 2016-May (EP0870765B1) 2013-Mar (JP) Not available 2021-May (JP3181919B2) 2016-May (CN1063442C) Mechanism of Action Acotiamide hydrochloride hydrate is an acetylcholinesterase (AChE) inhibitor and enhanced the acetylcholine (ACh)-induced contraction and motility of the gastric antrum and the gastric body. Target Binding Selectivity In vitro Efficacy In vivo Efficacy Mixed pattern: Ki1= 0.61 µM Effect dose of contraction in gastric sample: Significantly improved the gastrointestinal motility: Ki2= 2.7 µM ACh-induced: at 1 µM In normal and gastric hypomotility dogs: at 10 mg/kg. Inhibition: IC50= 3 µM Electrical-induced: at 0.3 µM In gastric hypomotility rats: at 100 mg/kg. Pharmacokinetics Parameters Rats Dogs Healthy Humans 3 10 3 10 50 mg 100 mg 200 mg 400 mg 800 mg Dose (mg/kg) (i.v.) (p.o.) (i.v.) (p.o.) (p.o.) (p.o.) (p.o.) (p.o.) (p.o.) Tmax (hr) - 0.08 - 0.5 2.75 2.42 2.08 2.25 2.13 Cmax -

New Developments in Prokinetic Therapy for Gastric Motility Disorders
REVIEW published: 24 August 2021 doi: 10.3389/fphar.2021.711500 New Developments in Prokinetic Therapy for Gastric Motility Disorders Michael Camilleri* and Jessica Atieh Clinical Enteric Neuroscience Translational and Epidemiological Research (CENTER), Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, MN, United States Prokinetic agents amplify and coordinate the gastrointestinal muscular contractions to facilitate the transit of intra-luminal content. Following the institution of dietary recommendations, prokinetics are the first medications whose goal is to improve gastric emptying and relieve symptoms of gastroparesis. The recommended use of metoclopramide, the only currently approved medication for gastroparesis in the United States, is for a duration of less than 3 months, due to the risk of reversible or irreversible extrapyramidal tremors. Domperidone, a dopamine D2 receptor antagonist, is available for prescription through the FDA’s program for Expanded Access to Investigational Drugs. Macrolides are used off label and are associated with tachyphylaxis and variable duration of efficacy. Aprepitant relieves some symptoms of gastroparesis. There are newer agents in the pipeline targeting diverse gastric (fundic, antral and pyloric) motor functions, including novel serotonergic 5-HT4 agonists, dopaminergic D2/3 antagonists, neurokinin NK1 antagonists, and ghrelin agonist. Novel Edited by: targets with potential to improve gastric motor functions include the pylorus, macrophage/ Jan Tack, inflammatory function, oxidative -

Prokinetics and Ghrelin for the Management of Cancer Cachexia Syndrome
85 Review Article Prokinetics and ghrelin for the management of cancer cachexia syndrome Jimi S. Malik, Sriram Yennurajalingam Department of Palliative Care, Rehabilitation and Integrative Medicine, The University of Texas MD Anderson Cancer Center, Houston, TX, USA Contributions: (I) Conception and design: All authors; (II) Administrative support: S Yennurajalingam; (III) Provision of study materials or patients: S Yennurajalingam; (IV) Collection and assembly of data: All authors; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Sriram Yennurajalingam, MD. Department of Palliative Care, Rehabilitation, and Integrative Medicine, The University of Texas MD Anderson Cancer Center, 1515 Holcombe Blvd., Unit 1414, Houston, TX 77030, USA. Email: [email protected]. Abstract: Cancer cachexia (CC) is one of the most distressing syndromes for both patients and their families. CC can have an impact on patient reported quality of life and overall survival. It is often associated with symptoms such as fatigue, depressed mood, early satiety, and anorexia. Prokinetic agents have been found to improve chronic nausea and early satiety associated with CC. Among the prokinetic agents, metoclopramide is one of the best studied medications. The role of the other prokinetic agents, such as domperidone, erythromycin, haloperidol, levosulpiride, tegaserod, cisapride, mosapride, renzapride, and prucalopride is unclear for use in cachectic cancer patients due to their side effect profile and limited efficacy studies in cancer patients. There has been an increased interest in the use of ghrelin-receptor agonists for the treatment of CC. Anamorelin HCl is a highly selective, novel ghrelin receptor agonist. -

Product List March 2019 - Page 1 of 53
Wessex has been sourcing and supplying active substances to medicine manufacturers since its incorporation in 1994. We supply from known, trusted partners working to full cGMP and with full regulatory support. Please contact us for details of the following products. Product CAS No. ( R)-2-Methyl-CBS-oxazaborolidine 112022-83-0 (-) (1R) Menthyl Chloroformate 14602-86-9 (+)-Sotalol Hydrochloride 959-24-0 (2R)-2-[(4-Ethyl-2, 3-dioxopiperazinyl) carbonylamino]-2-phenylacetic 63422-71-9 acid (2R)-2-[(4-Ethyl-2-3-dioxopiperazinyl) carbonylamino]-2-(4- 62893-24-7 hydroxyphenyl) acetic acid (r)-(+)-α-Lipoic Acid 1200-22-2 (S)-1-(2-Chloroacetyl) pyrrolidine-2-carbonitrile 207557-35-5 1,1'-Carbonyl diimidazole 530-62-1 1,3-Cyclohexanedione 504-02-9 1-[2-amino-1-(4-methoxyphenyl) ethyl] cyclohexanol acetate 839705-03-2 1-[2-Amino-1-(4-methoxyphenyl) ethyl] cyclohexanol Hydrochloride 130198-05-9 1-[Cyano-(4-methoxyphenyl) methyl] cyclohexanol 93413-76-4 1-Chloroethyl-4-nitrophenyl carbonate 101623-69-2 2-(2-Aminothiazol-4-yl) acetic acid Hydrochloride 66659-20-9 2-(4-Nitrophenyl)ethanamine Hydrochloride 29968-78-3 2,4 Dichlorobenzyl Alcohol (2,4 DCBA) 1777-82-8 2,6-Dichlorophenol 87-65-0 2.6 Diamino Pyridine 136-40-3 2-Aminoheptane Sulfate 6411-75-2 2-Ethylhexanoyl Chloride 760-67-8 2-Ethylhexyl Chloroformate 24468-13-1 2-Isopropyl-4-(N-methylaminomethyl) thiazole Hydrochloride 908591-25-3 4,4,4-Trifluoro-1-(4-methylphenyl)-1,3-butane dione 720-94-5 4,5,6,7-Tetrahydrothieno[3,2,c] pyridine Hydrochloride 28783-41-7 4-Chloro-N-methyl-piperidine 5570-77-4 -

Impact of Itopride and Domperidone on Sensitivity of Gastric Distention and Gastric Accommodation in Healthy Volunteers
Impact of Itopride and Domperidone on sensitivity of gastric distention and gastric accommodation in healthy volunteers. Karen Van den Houte, Florencia Carbone, Ans Pauwels, Rita Vos, Tim Vanuytsel, Jan Tack Translational Research Center for Gastrointestinal Disorders, KULeuven, Belgium BACKGROUND & AIM RESULTS Functional dyspepsia (FD), defined as upper abdominal symptoms affecting Conduct of the study Gastric accommodation daily life, as postprandial fullness, early satiation, epigastric pain, and epigastric • 15 healthy volunteers (9 female, 6 male) • No significant differences in VAS scores before and after meal burning, without any underlying organic disease, is one of the most common • Mean age: 28.3±5.8 years ingestion and no significant differences in preprandial intragastric functional gastrointestinal disorders (1). volumes were observed. Itopride, a prokinetic drug with dopamine D2-antagonistic and cholinesterase Gastric compliance and gastric sensitivity • Postprandial gastric volumes and gastric accommodation were inhibitor properties, is frequently used to treat functional dyspepsia. Its effects I50, I100, and D10 did not affect fasting or postprandial gastric significantly lower for I50 and for D10, compared to placebo. on gastric sensitivity and accommodation are unknown (2), compliance and gastric sensitivity to distention significantly The aim of this study is to evaluate the effect of Itopride, compared to compared to placebo. Domperidone, a dopamine D2 receptor antagonist, on the sensitivity to gastric * Placebo balloon -

Pharmacological Agents Currently in Clinical Trials for Disorders in Neurogastroenterology
Pharmacological agents currently in clinical trials for disorders in neurogastroenterology Michael Camilleri J Clin Invest. 2013;123(10):4111-4120. https://doi.org/10.1172/JCI70837. Clinical Review Esophageal, gastrointestinal, and colonic diseases resulting from disorders of the motor and sensory functions represent almost half the patients presenting to gastroenterologists. There have been significant advances in understanding the mechanisms of these disorders, through basic and translational research, and in targeting the receptors or mediators involved, through clinical trials involving biomarkers and patient responses. These advances have led to relief of patients’ symptoms and improved quality of life, although there are still significant unmet needs. This article reviews the pipeline of medications in development for esophageal sensorimotor disorders, gastroparesis, chronic diarrhea, chronic constipation (including opioid-induced constipation), and visceral pain. Find the latest version: https://jci.me/70837/pdf Review Pharmacological agents currently in clinical trials for disorders in neurogastroenterology Michael Camilleri Clinical Enteric Neuroscience Translational and Epidemiological Research (CENTER), Mayo Clinic, Rochester, Minnesota, USA. Esophageal, gastrointestinal, and colonic diseases resulting from disorders of the motor and sensory functions represent almost half the patients presenting to gastroenterologists. There have been significant advances in under- standing the mechanisms of these disorders, through basic and translational research, and in targeting the recep- tors or mediators involved, through clinical trials involving biomarkers and patient responses. These advances have led to relief of patients’ symptoms and improved quality of life, although there are still significant unmet needs. This article reviews the pipeline of medications in development for esophageal sensorimotor disorders, gastropa- resis, chronic diarrhea, chronic constipation (including opioid-induced constipation), and visceral pain. -

4 Supplementary File
Supplemental Material for High-throughput screening discovers anti-fibrotic properties of Haloperidol by hindering myofibroblast activation Michael Rehman1, Simone Vodret1, Luca Braga2, Corrado Guarnaccia3, Fulvio Celsi4, Giulia Rossetti5, Valentina Martinelli2, Tiziana Battini1, Carlin Long2, Kristina Vukusic1, Tea Kocijan1, Chiara Collesi2,6, Nadja Ring1, Natasa Skoko3, Mauro Giacca2,6, Giannino Del Sal7,8, Marco Confalonieri6, Marcello Raspa9, Alessandro Marcello10, Michael P. Myers11, Sergio Crovella3, Paolo Carloni5, Serena Zacchigna1,6 1Cardiovascular Biology, 2Molecular Medicine, 3Biotechnology Development, 10Molecular Virology, and 11Protein Networks Laboratories, International Centre for Genetic Engineering and Biotechnology (ICGEB), Padriciano, 34149, Trieste, Italy 4Institute for Maternal and Child Health, IRCCS "Burlo Garofolo", Trieste, Italy 5Computational Biomedicine Section, Institute of Advanced Simulation IAS-5 and Institute of Neuroscience and Medicine INM-9, Forschungszentrum Jülich GmbH, 52425, Jülich, Germany 6Department of Medical, Surgical and Health Sciences, University of Trieste, 34149 Trieste, Italy 7National Laboratory CIB, Area Science Park Padriciano, Trieste, 34149, Italy 8Department of Life Sciences, University of Trieste, Trieste, 34127, Italy 9Consiglio Nazionale delle Ricerche (IBCN), CNR-Campus International Development (EMMA- INFRAFRONTIER-IMPC), Rome, Italy This PDF file includes: Supplementary Methods Supplementary References Supplementary Figures with legends 1 – 18 Supplementary Tables with legends 1 – 5 Supplementary Movie legends 1, 2 Supplementary Methods Cell culture Primary murine fibroblasts were isolated from skin, lung, kidney and hearts of adult CD1, C57BL/6 or aSMA-RFP/COLL-EGFP mice (1) by mechanical and enzymatic tissue digestion. Briefly, tissue was chopped in small chunks that were digested using a mixture of enzymes (Miltenyi Biotec, 130- 098-305) for 1 hour at 37°C with mechanical dissociation followed by filtration through a 70 µm cell strainer and centrifugation. -

PHARMACEUTICAL APPENDIX to the TARIFF SCHEDULE 2 Table 1
Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names INN which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service CAS registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. -

The Pharmacology of Prokinetic Agents and Their Role in the Treatment of Gastrointestinal Disorders
The Pharmacology of ProkineticAgents IJGE Issue 4 Vol 1 2003 Review Article The Pharmacology of Prokinetic Agents and Their Role in the Treatment of Gastrointestinal Disorders George Y. Wu, M.D, Ph.D. INTRODUCTION Metoclopramide Normal peristalsis of the gut requires complex, coordinated neural and motor activity. Pharmacologic Category : Gastrointestinal Abnormalities can occur at a number of different Agent. Prokinetic levels, and can be caused by numerous etiologies. This review summarizes current as well as new Symptomatic treatment of diabetic gastric agents that show promise in the treatment of stasis gastrointestinal motility disorders. For these Gastroesophageal reflux e conditions, the most common medications used in s Facilitation of intubation of the small the US are erythromycin, metoclopramide, and U intestine neostigmine (in acute intestinal pseudo- Prevention and/or treatment of nausea and obstruction). A new prokinetic agent, tegaserod, vomiting associated with chemotherapy, has been recently approved, while other serotonin radiation therapy, or post-surgery (1) agonist agents (prucalopride, YM-31636, SK-951, n ML 10302) are currently undergoing clinical o Blocks dopamine receptors in chemoreceptor i t studies. Other prokinetics, such as domperidone, c trigger zone of the CNS (2) A are not yet approved in the US, although are used in f Enhances the response to acetylcholine of o other countries. tissue in the upper GI tract, causing enhanced m s i n motility and accelerated gastric emptying a DELAYED GASTRIC EMPTYING OR h without stimulating gastric, biliary, or c G A S T R O E S O P H A G E A L R E F L U X e pancreatic secretions. -

CAS Number Index
2334 CAS Number Index CAS # Page Name CAS # Page Name CAS # Page Name 50-00-0 905 Formaldehyde 56-81-5 967 Glycerol 61-90-5 1135 Leucine 50-02-2 596 Dexamethasone 56-85-9 963 Glutamine 62-44-2 1640 Phenacetin 50-06-6 1654 Phenobarbital 57-00-1 514 Creatine 62-46-4 1166 α-Lipoic acid 50-11-3 1288 Metharbital 57-22-7 2229 Vincristine 62-53-3 131 Aniline 50-12-4 1245 Mephenytoin 57-24-9 1950 Strychnine 62-73-7 626 Dichlorvos 50-23-7 1017 Hydrocortisone 57-27-2 1428 Morphine 63-05-8 127 Androstenedione 50-24-8 1739 Prednisolone 57-41-0 1672 Phenytoin 63-25-2 335 Carbaryl 50-29-3 569 DDT 57-42-1 1239 Meperidine 63-75-2 142 Arecoline 50-33-9 1666 Phenylbutazone 57-43-2 108 Amobarbital 64-04-0 1648 Phenethylamine 50-34-0 1770 Propantheline bromide 57-44-3 191 Barbital 64-13-1 1308 p-Methoxyamphetamine 50-35-1 2054 Thalidomide 57-47-6 1683 Physostigmine 64-17-5 784 Ethanol 50-36-2 497 Cocaine 57-53-4 1249 Meprobamate 64-18-6 909 Formic acid 50-37-3 1197 Lysergic acid diethylamide 57-55-6 1782 Propylene glycol 64-77-7 2104 Tolbutamide 50-44-2 1253 6-Mercaptopurine 57-66-9 1751 Probenecid 64-86-8 506 Colchicine 50-47-5 589 Desipramine 57-74-9 398 Chlordane 65-23-6 1802 Pyridoxine 50-48-6 103 Amitriptyline 57-92-1 1947 Streptomycin 65-29-2 931 Gallamine 50-49-7 1053 Imipramine 57-94-3 2179 Tubocurarine chloride 65-45-2 1888 Salicylamide 50-52-2 2071 Thioridazine 57-96-5 1966 Sulfinpyrazone 65-49-6 98 p-Aminosalicylic acid 50-53-3 426 Chlorpromazine 58-00-4 138 Apomorphine 66-76-2 632 Dicumarol 50-55-5 1841 Reserpine 58-05-9 1136 Leucovorin 66-79-5 -
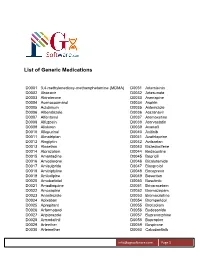
List of Generic Medications
List of Generic Medications D0001 3,4-methylenedioxy-methamphetamine (MDMA) D0031 Artemisinin D0002 Abacavir D0032 Artesunate D0003 Abiraterone D0033 Asenapine D0004 Acenocoumarol D0034 Aspirin D0005 Aclidinium D0035 Astemizole D0006 Albendazole D0036 Atazanavir D0007 Alfentanyl D0037 Atomoxetine D0008 Alfuzosin D0038 Atorvastatin D0009 Aliskiren D0039 Avanafil D0010 Allopurinol D0040 Axitinib D0011 Almotriptan D0041 Azathioprine D0012 Alogliptin D0042 Azilsartan D0013 Alosetron D0043 Bazedoxifene D0014 Alprazolam D0044 Bedaquiline D0015 Amantadine D0045 Bepridil D0016 Amiodarone D0046 Bicalutamide D0017 Amisulpride D0047 Bisoprolol D0018 Amitriptyline D0048 Boceprevir D0019 Amlodipine D0049 Bosentan D0020 Amobarbital D0050 Bosutinib D0021 Amodiaquine D0051 Brivaracetam D0022 Amoxapine D0052 Bromazepam D0023 Anastrozole D0053 Bromocriptine D0024 Apixaban D0054 Bromperidol D0025 Aprepitant D0055 Brotizolam D0026 Arformoterol D0056 Budesonide D0027 Aripiprazole D0057 Buprenorphine D0028 Armodafinil D0058 Bupropion D0029 Arteether D0059 Buspirone D0030 Artemether D0060 Cabozantinib [email protected] Page 1 List of Generic Medications D0061 Canagliflozin D0091 Clofarabine D0062 Cannabidiol (CBD) D0092 Clofibrate D0063 Cannabinol (CBN) D0093 Clomipramine D0064 Captopril D0094 Clonazepam D0065 Carbamazepine D0095 Clonidine D0066 Carisoprodol D0096 Clopidogrel D0067 Carmustine D0097 Clorazepate D0068 Carvedilol D0098 Clozapine D0069 Celecoxib D0099 Cocaine D0070 Ceritinib D0100 Codeine D0071 Cerivastatin D0101 Colchicine D0072 Cetirizine