Postpartum Contraception
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
A History of Birth Control Methods
Report Published by the Katharine Dexter McCormick Library and the Education Division of Planned Parenthood Federation of America 434 West 33rd Street, New York, NY 10001 212-261-4716 www.plannedparenthood.org Current as of January 2012 A History of Birth Control Methods Contemporary studies show that, out of a list of eight somewhat effective — though not always safe or reasons for having sex, having a baby is the least practical (Riddle, 1992). frequent motivator for most people (Hill, 1997). This seems to have been true for all people at all times. Planned Parenthood is very proud of the historical Ever since the dawn of history, women and men role it continues to play in making safe and effective have wanted to be able to decide when and whether family planning available to women and men around to have a child. Contraceptives have been used in the world — from 1916, when Margaret Sanger one form or another for thousands of years opened the first birth control clinic in America; to throughout human history and even prehistory. In 1950, when Planned Parenthood underwrote the fact, family planning has always been widely initial search for a superlative oral contraceptive; to practiced, even in societies dominated by social, 1965, when Planned Parenthood of Connecticut won political, or religious codes that require people to “be the U.S. Supreme Court victory, Griswold v. fruitful and multiply” — from the era of Pericles in Connecticut (1965), that finally and completely rolled ancient Athens to that of Pope Benedict XVI, today back state and local laws that had outlawed the use (Blundell, 1995; Himes, 1963; Pomeroy, 1975; Wills, of contraception by married couples; to today, when 2000). -

Contraception
Contraception The Society of Obstetricians and Gynaecologists of Canada sexandu.ca Introduction Contraception Contraception, also known as birth control, is used In this section, we review the methods that are available to prevent pregnancy. There are many different birth to help you understand the options and help you narrow control methods to help you and your partner prevent an down the choices. You can always talk over your choices unplanned pregnancy. You may be starting with a pretty with your health care provider. good idea of what you are looking for, or you may not be sure where to start – or which method to choose. *These summaries are for information purposes only and are incomplete. When considering contraception, patients should review all potential risks and benefits on a medicine, device or procedure with their health care providers prior to selecting the option that is most appropriate for their needs. Topics Covered Emergency Contraception Hormonal Contraception Oral Contraceptive Pill Contraceptive Patch Vaginal Ring Intrauterine Contraception (IUC) Injectable Contraception Non-Hormonal Contraception Male Condom Female Condom Sponge Cervical Cap Diaphragm Spermicides Vasectomy Tubal Ligation & Tubal Occlusion Intrauterine Contraception (IUC) Natural Methods Fertility-Awareness Based Methods Lactational Amenorrhea Method (LAM) Withdrawal (Coitus interruptus) Abstinence sexandu.ca Emergency Contraception Emergency Contraception Emergency contraception is not to be used as a regular method of birth control but, if needed, it can help prevent unplanned pregnancies. If you have had unprotected sex and you already know that you do not want to get pregnant, emergency contraception can help prevent unplanned pregnancies if used as soon as possible. -

Collection of Semen for Analysis
Collection of Semen for Analysis Specimens will be accepted Monday through Friday between 6 a.m. and 7 p.m. excluding holidays. Private collection rooms are not available at either of the testing sites. 1. Semen is to be collected after a period of two to seven days of sexual abstinence. 2. Produce the specimen by masturbation and collect in a sterile plastic container. Note: Collection by interrupted sexual intercourse (coitus interruptus) is not recommended due to a likely loss of the first portion of the ejaculate, which contains the highest concentration of spermatozoa. Condoms contain spermicidal agents and must not be used for specimen collection. 3. Label the container with patient’s name, date of birth and date and time of collection. It is very important that testing begins within 30 minutes after collection. 4. The specimen should be kept as close to body temperature as possible. Protect from extremes of heat or cold until it reaches the laboratory. 5. Please complete the questionnaire on reverse side and bring it with you to laboratory. 6. The specimen must be taken directly to the laboratory at either Lakeland Hospital, Niles or Lakeland Medical Center, St. Joseph within 30 minutes after collection. Lakeland Hospital, Niles Lakeland Medical Center 31 N. St. Joseph Avenue 1234 Napier Avenue Niles, MI 49120 St. Joseph, MI 49085 NS050-127 (6/17) www.lakelandhealth.org Lakeland Laboratory Semen Collection Patient Information Form Patient Name: __________________________________ Date:__________________ This information is required for adequate interpretation of your test resultes. Date of collection: __________________________________ Time of colletion: ___________________________________ q a.m. -

Contraception and Abortion Contraception Contraception Methods of Contraception Coitus Interruptus (Withdrawal)
12/3/2013 Contraception Contraception and • The intentional prevention of pregnancy Abortion – Birth control- the device or practice to decrease risk of conceiving – Family planning – conscious decision on when to conceive • More than half of pregnancies each year are unintended in Foundations of MCH women under 20 years • Risk of pregnancy with contraception – Using an imperfect method of contraception – Using a method of contraception incorrectly • Decreasing the risk of pregnancy – Providing adequate instruction about how to use contraceptive methods, when to use a backup method, & when to use emergency contraception Contraception Methods of Contraception • Contraceptive failure • Coitus Interruptus – The percentage of contraceptive users expected to have • Natural Family Planning & Fertility Awareness an accidental pregnancy during the first year, even Methods when use of methods is consistent and correct Barrier Methods – Effectiveness varies from couple to couple • • Properties of the method • Hormonal Methods • Characteristics of the user • Emergency Contraception • Failure rates decrease over time • Intrauterine Devices – Users gain experience • Sterilization – Users use methods more appropriately • Future Trends – Less effective users stop using the methods Natural Family Planning & Fertility Coitus Interruptus (Withdrawal) Awareness Methods • Involves the male partner withdrawing the • Knowledge of the menstrual cycle is basic to the practice of NFP penis from the woman’s vagina before he – Human ovum can be fertilized no later -

Impact of the COVID-19 Pandemic on Sexual and Reproductive Health Among Women with Induced Abortion
www.nature.com/scientificreports OPEN Impact of the COVID‑19 pandemic on sexual and reproductive health among women with induced abortion Pengcheng Tu1,2, Jianan Li1,2, Xiaomei Jiang1, Kaiyan Pei1,2,3* & Yiqun Gu1,2,3 The coronavirus disease (COVID‑19) has already been declared a global pandemic. To our knowledge, there is very little information regarding the efects of COVID‑19 on women seeking reproductive health services, specifcally abortion. This study was aimed to assess the impact of the COVID‑19 pandemic on reproductive and sexual health among women seeking abortion services. We conducted a series of preliminary analyses using data collected from ten maternal and child health hospitals of seven provinces in China before and during the COVID‑19 lockdown. The present study showed that a signifcant decrease was observed in the frequency of sexual intercourse during the COVID‑19 pandemic. Moreover, a signifcant increase in contraceptive use including condom, rhythm method and coitus interruptus whereas a decrease in choosing oral contraceptives were observed during the COVID‑19 pandemic. In addition, the pandemic was associated with increased intention of seeking induced abortion due to social factors. Future research should look into the long‑term impact of the COVID‑19 pandemic on sexual and reproductive health. As an event that can cause physical, emotional, and psychological harm, the COVID-19 pandemic may afect sexual and reproductive health of individuals. From the end of January 2020, people in China were required to implement “social distancing” and restricted to step outside homes except for essential activities, and public transport was suspended1,2. -

Fact Sheet Scale None EC.Indd 1 10/02/2006 14:41:38 UNDP/UNFPA/WHO/World Bank • Special Programme of Research, Devleopment and Research Training in Human Repoduction
Levonorgestrel for emergency contraception fact sheet fact sheet Emergency contraception refers to back- – dislodgment, breakage, tearing, or early October 2005 up methods for contraceptive emergencies removal of a diaphragm or cervical cap which women can use within the fi rst few – failed coitus interruptus (e.g., ejacula- days after unprotected intercourse to pre- tion in vagina or on external genitalia) vent an unwanted pregnancy. Emergency – failure of a spermicide tablet or fi lm to contraceptives are not suitable for regular melt before intercourse use. – miscalculation of the periodic The WHO-recommended regimen for emer- abstinence method or failure to abstain gency contraception is: on fertile day of cycle • 1.5 mg levonorgestrel as a single dose. – IUD expulsion; • in cases of sexual assault when the Who needs emergency contraception? woman was not protected by an effec- Any woman of reproductive age may need tive contraceptive method. emergency contraception at some point to avoid an unwanted pregnancy. It is meant Mode of action to be used in situations such as: Levonorgestrel emergency contraceptive • when no contraceptive has been used; pills (ECPs) have been shown to prevent • when there is a contraceptive failure or ovulation and they did not have any detect- incorrect use, including: able effect on the endometrium (uterine – condom breakage, slippage, or incor- lining) or progesterone levels when given rect use after ovulation. ECPs are not effective once – three or more consecutive missed the process of implantation has begun, and combined oral contraceptive pills will not cause abortion. – progestogen-only pill (minipill) taken morethan three hours late Effectiveness Based on reports from four studies includ- – more than two weeks late for a pro- ing almost 5000 women, the levonorgestrel gestogen-only contraceptive injection regimen used within 5 days after unpro- (depot-medroxyprogesterone acetate or tected intercourse reduced a woman’s norethisterone enanthate) chance of pregnancy by 60-90 per cent. -
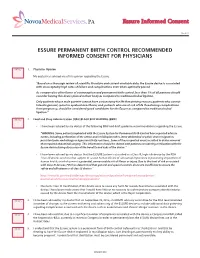
Essure Informed Consent Form
No vo aMe di ca lServi ces, PA Essure Informed Consent Rev 4/1 6 ESSURE PERMANENT BIRTH CONTROL RECOMMENDED INFORMED CONSENT FOR PHYSICIANS INITIALS 1. Physician Opinion My doctor has advised me of his opinion regarding the Essure. “Based on a thorough review of scientific literature and current available data, the Essure device is associated with unacceptably high rates of failure and complications even when optimally placed. As compared to other forms of contraception and permanent birth control, less than 1% of all patients should consider having this device placed in their body as compared to traditional tubal ligation. Only patients whose male partner cannot have a vasectomy for life threatening reasons; patients who cannot tolerate general, spinal or epidural anesthesia; and, patients who are at risk of life threatening complications from pregnancy, should be considered good candidates for the Essure as compared to traditional tubal ligation.” INITIALS 2. Food and Drug Administration (FDA) BLACK BOX WARNING (BBW) • I have been advised by my doctor of the following BBW and draft guidance recommendations regarding the Essure. “WARNING: Some patients implanted with the Essure System for Permanent Birth Control have reported adverse events, including perforation of the uterus and/or fallopian tubes, intra-abdominal or pelvic device migration, persistent pain, and allergy or hypersensitivity reactions. Some of these reported events resulted in device removal that required abdominal surgery. This information should be shared with patients considering sterilization with the Essure device during discussion of the benefits and risks of the device.” • I have been advised by my doctor that the ESSURE System is classified as a Class III, high risk device by the FDA. -

Sexual Behavior of Adolescents with an Emphasis on Use of Contraceptives / Risk of Sexually Transmitted Infections
Cent Eur J Nurs Midw 2020;11(1):2–8 doi: 10.15452/CEJNM.2020.11.0002 ORIGINAL PAPER SEXUAL BEHAVIOR OF ADOLESCENTS WITH AN EMPHASIS ON USE OF CONTRACEPTIVES / RISK OF SEXUALLY TRANSMITTED INFECTIONS Simona Kelčíková1, Marcela Pydová1, Nora Malinovská2 1Department of Midwifery, Jessenius Faculty of Medicine in Martin, Comenius University in Bratislava, Slovakia 2Department of Foreign Languages, Jessenius Faculty of Medicine in Martin, Comenius University in Bratislava, Slovakia Received June 17, 2019; Accepted December 16, 2019. Copyright: This is an open access article under the CC BY-NC-ND license. Abstract Aim: The aim of the study was to survey adolescent sexual behavior, use of contraceptives, and sexually transmitted infections, and, in addition, to see how these factors correlated with selected individual characteristics of the respondents (e.g., age, gender). Design: A quantitative cross-sectional study. Methods: An exploratory method, using a specially designed questionnaire, was selected. The research sample consisted of 381 adolescents with an average age of 17.75 years (± 1.28). Data were analyzed using descriptive statistics and the Chi-squared (χ2) test (p < 0.05). Results: More than half of adolescents (61.35%; 2.49 ± 1.91) have had sexual intercourse. We found a variety of reasons for differences in the use of contraceptive methods. The most commonly used contraceptive methods during sexual intercourse were male condoms (50.13%), and hormonal pills (16.80%). However, most respondents (86.61%) reported they had not used condoms during their last sexual intercourse. Only 12.86% of respondents considered their sexual behavior safe. Statistically significant differences were found in adolescent sexual behavior relating to contraceptive use in terms of gender and age (p < 0.05). -

Contraception and Abortion in Medieval Medicine Amanda Hartigan
Contraception and Abortion in Medieval Medicine Religious Views Infanticide Amanda Hartigan By the early Middle Ages, pagan and Christian alike had reached Although religious and some secular law spoke against exposure of infant, consensus in condemning sodomy, adultery, abortion, contraception, some data from the Middle Ages show a higher male-female ratio than one Department of History mutilation (notably castration), nudity, sexual relations, during would expect in a biologically neutral environment free from interferences. It State University of New York, College at Oneonta menstruation and after birth until weaning, and infanticide. Religious has been found that children had to be born before their sex was known; in values held the most important influence on the use of birth control, the premodern period there were more males born than females; biologically, before and after one conceives. Taking their cue from the Old Testament we would expect a male-female ratio closer to 1:1 and it has been found that Contraceptive Practices commandment to “Be fruitful, and multiply,” medieval Christianity saw premoderns practiced some form(s) of birth control; therefore the means of Coitus Interruptus- Scholars agree that evidence in Roman literature for coitus the sole purpose of sex as a means to conceive children. Therefore, the population control practiced was infanticide. However, mist historians doubt interruptus is virtually nonexistent but other could argue that it was so common idea that one could use birth control to stop conception was usually that there was extensive infanticide during the Middle Ages. A study and kept so private that sources do not even refer to it. -

Male Contraception Without Prescription a Reevaluation of the Condom and Coitus Interruptus
Male Contraception Without Prescription A Reevaluation of the Condom and Coitus Interruptus MICHAEL J. FREE, PhD, and NANCY J. ALEXANDER, PhD CONTRACEPTIVE METHODS imple- the stigma of being associated with mented by the male were among promiscuity and venereal disease- the first birth control procedures. an association stamped on them by Even today these methods have sig- the military services and the "old nificance for almost every sexually morality" and perpetuated until active person during some stage of life, and they constitute the main or only birth control methods prac- D Dr. Free is senior research scien- ticed by many couples. Therefore tist, biology department, Battelle physicians, in particular, should Pacific Northwest Laboratories, know the background, subtleties, Richland, Wash. Dr. Alexander, strengths, and shortcomings of these associate scientist in reproductive nonprescription methods for male physiology, Oregon Regional Pri- use. mate Research Center, Beaverton, is director, Infertility Laboratory The Condom at the University of Oregon Often denigrated by being cate- Health Sciences Center, Portland. gorized as a "traditional" contra- This paper is Oregon Regional ceptive method and accorded only Primate Research Center Publica- the cursory interest given to his- tion No. 836, whose preparation torical artifacts, the condom is was supported in part by National clearly not a symbol of our times. Institutes of Health grants Nos. HD Because condoms must be used at 05969 and RR 00163. Tearsheet re- the time of coitus, in the past they quests to Dr. Michael J. Free, were perhaps too personally and Biology Department, Battelle Pacific graphically sexual for Western Northwest Laboratories, Battelle sensibilities. -

Patient Instructions Semen Analysis Collection
PATIENT INSTRUCTIONS SEMEN ANALYSIS COLLECTION Sample Collection • Refrain from sexual activity (including masturbation) for 48 hours prior to the planned date of collection. Abstinence should be no longer than 7 days prior to the collection. • Wash and dry hands and genitals. • Collect entire semen emission using masturbation into the sterile collection container provided. o Do not use a sheath or condom for collection as this can decrease sperm activity and viability and will thus invalidate the results. o Do not collect the specimen via coitus interruptus since the first portion of the ejaculate contains the highest concentration of spermatozoa and this method jeopardizes collection of this portion. • Record your name, date of birth, date and time of collection on the label. Record your spouse or partner’s name also. Delivery • The sample must be delivered to the laboratory location listed below within one hour of collection. (Samples may be collected on-site at the location below if the delivery time is a concern.) • Ensure that sample temperature is maintained at room temperature or body temperature (by carrying near the body). Samples must not be refrigerated or artificially heated. • Drop the specimen off at the location below: Allenmore Hospital Laboratory (253-459-6336) 1901 S Union Ave Tacoma, WA 98405. Ask at the inside information desk to be directed to the laboratory. Monday – Friday only 8:00am – 2pm (test is not available on weekends) Test Information Patient Name: ________________________________________ DOB: __________________ -

The Current Status of Fertility Control
THE CURRENT STATUS OF FERTILITY CONTROL CmsToPHER Tmrm* About two-thirds of the human race inhabit those regions of the world where the practice of birth control is sufficiently limited to make it appropriate to refer to them as regions of uncontrolled fertility. In these areas, the annual birth rate ranges between about forty and fifty per i,ooo population. The remaining one-third of the world's people inhabits areas where fertility is comparatively well-controlled-North America, Europe (including the Soviet Union), the temperate zones of South America and Oceania, and Japan. In most of the countries of these regions, the annual birth rate in recent years has ranged from about fifteen to twenty-five per i,ooo population.' This article discusses the methods employed to control fertility, and the extent and effectiveness of their use in the United States and other countries. From a biological point of view, all of these methods may be conveniently grouped into four categories: (i) abstinence, (2) contraception, (3) sterilization, and (4) abortion. From a sociological point of view, delayed marriage and permanent celibacy, as well as other customs reducing the proportion married among the population of reproductive age, must also be considered to be methods of fertility control, since in most societies, varying degrees of restraint are imposed on the sexual activities of unmarried persons. I * ABsTINENcE Ireland is the classical example of a country where social institutions serve as effective restraints on population growth. According to the Irish census of i95I, about thirty-one per cent of the men and twenty-six per cent of the women at fifty years of age had never married, as compared with about eight per cent for either sex in the United States.