Cambia (Diclofenac)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Acute Renal Failure Associated with Diflunisal J. G. WHARTON D. 0
Postgrad Med J: first published as 10.1136/pgmj.58.676.104 on 1 February 1982. Downloaded from Postgraduate Medical Journal (February 1982) 58, 104-105 Acute renal failure associated with diflunisal J. G. WHARTON D. 0. OLIVER B.Sc., M.R.C.P. F.R.C.P., F.R.A.C.P. M. S. DUNNILL F.R.C.P., F.R.C.Path. Renal Unit, Churchill Hospital, and Department of Pathology, John Radcliffe Hospital, Oxford Summary eosinophils 224 x 106/1; ESR 30 mm/hr; urea 305 The case of a 44-year-old man with acute oliguric mmol/l; creatinine 1651 ,Lmol/l; potassium 6-43 renal failure due to tubulo-interstitial nephritis after mmol/l; serum amylase 88 Somogyi units; urine 3 months' diflunisal is reported. The possible mecha- contained no casts; no red cells but 10 neutrophils, nisms are discussed. no eosinophils and no growth. Antistreptolysin 0 titre 50 i.u./ml; IgG 16-5 g/l; IgA 3-8 g/l; IgM 1.1 g/l antinuclear factor negative; C3 122 mg/dl, C4 54Protected by copyright. Introduction mg/dl; hepatitis B surface antigen negative; chest Diflunisal has been reported as causing acute radiograph, cardiomegaly plus congestion; intra- allergic interstitial nephritis (Chan et al., 1980) venous urogram with tomograms, no obstruction, resulting in acute oliguric renal failure. A case of poor nephrogram. A renal biopsy showed tubulo- acute renal failure due to tubulo-interstitial nephritis interstitial nephritis with no eosinophil infiltrate. after 3 months of diflunisal is reported here. Recently, Diflunisal had been stopped 2 days before admission phenylakalonic acids with analgesic and anti- to this renal unit. -

Non-Steroidal Anti-Inflammatory Drugs (Nsaids)* *See List of Prescription NSAID Nsaids Are Used to Treat Pain, Redness, Swelling, and Heat (Inflammation)
Medication Guide Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)* *see list of prescription NSAID NSAIDs are used to treat pain, redness, swelling, and heat (inflammation). medicines at the end of this guide WHAT IS THE MOST IMPORTANT INFORMATION YOU SHOULD KNOW ABOUT NSAIDS? NSAIDs can increase the risk of kidney failure, gastrointestinal damage, heart attack or stroke. Heart Kidney Gastrointestinal Attack Damage Damage (GI) Never use right before or You should not take NSAIDs Beware of life-threatening after coronary bypass graft if you have one of these ulcers and bleeding that may ! (CABG) surgery. ! high-risk conditions: ! happen without warning. Your risk† of heart attack or • Kidney disease Your GI risk increases with: stroke increases if: • Diabetes • Taking medicines called corticosteroids • You have heart disease • High blood pressure and anticoagulants • Even with short-term use • You take water pills or pills with • Old age or having poor health † • Smoking and drinking alcohol low dose aspirin does not pose this risk names that end in ‘pril’ or ‘sartan’ Your health risks increase the longer you take NSAIDs WHO SHOULD NOT TAKE NSAIDS? Do talk to your doctor if you: Do not take NSAIDs if you: • have medical conditions • have had an allergic reaction to aspirin or other NSAID • are breastfeeding • are a pregnant woman late in your pregnancy • take more than one medication: show your health provider a list of all of your medicines — some may cause serious side effects when combined with NSAIDs. WHAT ARE SERIOUS SIDE EFFECTS YOU -

Arthritis Treatment Comparison Arthritis Treatment Comparison
ARTHRITIS TREATMENT COMPARISON ARTHRITIS TREATMENT COMPARISON GENERIC OA of (BRAND) HOW SUPPLIED AS GA JIA JRA OA Knee PsA RA CHELATING AGENTS Penicillamine Cap: 250mg ✓ (Cuprimine) Penicillamine Tab: 250mg ✓ (Depen) CYCLIC POLYPEPTIDE IMMUNOSUPPRESSANTS Cyclosporine Cap: 25mg, 100mg; ✓ (Gengraf, Neoral) Sol: 100mg/mL CYCLOOXYGENASE-2 INHIBITORS Celecoxib Cap: 50mg, 100mg, ✓ ✓ ✓ ✓ (Celebrex) 200mg, 400mg DIHYDROFOLIC ACID REDUCTASE INHIBITORS Methotrexate Inj: 25mg/mL; ✓ ✓ Tab: 2.5mg Methotrexate Tab: 5mg, 7.5mg, ✓ ✓ (Trexall) 10mg, 15mg INTERLEUKIN RECEPTOR ANTAGONISTS Anakinra Inj: 100mg/0.67mL ✓ (Kineret) Tocilizumab Inj: 20mg/mL, ✓ ✓ (Actemra) 162mg/0.9mL GOLD COMPOUNDS Auranofin Cap: 3mg ✓ (Ridaura) Gold sodium thiomalate Inj: 50mg/mL ✓ ✓ (Myochrysine) HYALURONAN AND DERIVATIVES Hyaluronan Inj: 30mg/2mL ✓ (Orthovisc) Sodium hyaluronate Inj: 1% ✓ (Euflexxa) Sodium hyaluronate Inj: 10mg/mL ✓ (Hyalgan) Sodium hyaluronate Inj: 2.5mL ✓ (Supartz) HYLAN POLYMERS Hylan G-F 20 Inj: 8mg/mL ✓ (Synvisc, Synvisc One) KINASE INHIBITORS Tofacitinib Tab: 5mg ✓ (Xeljanz) MONOCLONAL ANTIBODIES Ustekinumab Inj: 45mg/0.5mL, ✓ (Stelara) 90mg/mL MONOCLONAL ANTIBODIES/CD20-BLOCKERS Rituximab Inj: 100mg/10mL, ✓ (Rituxan) 500mg/50mL (Continued) ARTHRITIS TREATMENT COMPARISON GENERIC OA of (BRAND) HOW SUPPLIED AS GA JIA JRA OA Knee PsA RA MONOCLONAL ANTIBODIES/TNF-BLOCKERS Adalimumab Inj: 20mg/0.4mL, ✓ ✓ ✓ ✓ (Humira) 40mg/0.8mL Golimumab Inj: 50mg/0.5mL, ✓ ✓ ✓ (Simponi) 100mg/mL Infliximab Inj: 100mg ✓ ✓ ✓ (Remicade) NON-STEROIDAL ANTI-INFLAMMATORY DRUGS -

2 Inhibitors and Non-Steroidal Anti-Inflammatory Drugs (Nsaids)
Drug Class Review on Cyclo-oxygenase (COX)-2 Inhibitors and Non-steroidal Anti-inflammatory Drugs (NSAIDs) Final Report Update 3 Evidence Tables November 2006 Original Report Date: May 2002 Update 1 Report Date: September 2003 Update 2 Report Date: May 2004 A literature scan of this topic is done periodically The purpose of this report is to make available information regarding the comparative effectiveness and safety profiles of different drugs within pharmaceutical classes. Reports are not usage guidelines, nor should they be read as an endorsement of, or recommendation for, any particular drug, use or approach. Oregon Health & Science University does not recommend or endorse any guideline or recommendation developed by users of these reports. Roger Chou, MD Mark Helfand, MD, MPH Kim Peterson, MS Tracy Dana, MLS Carol Roberts, BS Produced by Oregon Evidence-based Practice Center Oregon Health & Science University Mark Helfand, Director Copyright © 2006 by Oregon Health & Science University Portland, Oregon 97201. All rights reserved. Note: A scan of the medical literature relating to the topic is done periodically(see http://www.ohsu.edu/ohsuedu/research/policycenter/DERP/about/methods.cfm for scanning process description). Upon review of the last scan, the Drug Effectiveness Review Project governance group elected not to proceed with another full update of this report. Some portions of the report may not be up to date. Prior versions of this report can be accessed at the DERP website. Final Report Update 3 Drug Effectiveness Review Project TABLE OF CONTENTS Evidence Table 1. Systematic reviews…………………………………………………………………3 Evidence Table 2. Randomized-controlled trials………………………………………………………9 Evidence Table 3. -

Nonsteroidal Anti-Inflammatory Drugs for Dysmenorrhoea (Review)
Cochrane Database of Systematic Reviews Nonsteroidal anti-inflammatory drugs for dysmenorrhoea (Review) Marjoribanks J, Ayeleke RO, Farquhar C, Proctor M Marjoribanks J, Ayeleke RO, Farquhar C, Proctor M. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database of Systematic Reviews 2015, Issue 7. Art. No.: CD001751. DOI: 10.1002/14651858.CD001751.pub3. www.cochranelibrary.com Nonsteroidal anti-inflammatory drugs for dysmenorrhoea (Review) Copyright © 2015 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. TABLE OF CONTENTS HEADER....................................... 1 ABSTRACT ...................................... 1 PLAINLANGUAGESUMMARY . 2 SUMMARY OF FINDINGS FOR THE MAIN COMPARISON . ..... 4 BACKGROUND .................................... 5 OBJECTIVES ..................................... 6 METHODS ...................................... 6 Figure1. ..................................... 8 Figure2. ..................................... 10 Figure3. ..................................... 12 RESULTS....................................... 14 Figure4. ..................................... 16 Figure5. ..................................... 18 Figure6. ..................................... 24 ADDITIONALSUMMARYOFFINDINGS . 25 DISCUSSION ..................................... 26 AUTHORS’CONCLUSIONS . 27 ACKNOWLEDGEMENTS . 27 REFERENCES ..................................... 28 CHARACTERISTICSOFSTUDIES . 40 DATAANDANALYSES. 130 Analysis 1.1. Comparison 1 NSAIDs vs placebo, Outcome 1 Pain relief dichotomous data. 136 -

Inflammatory Drugs (Nsaids) for People with Or at Risk of COVID-19
Evidence review Acute use of non-steroidal anti- inflammatory drugs (NSAIDs) for people with or at risk of COVID-19 Publication date: April 2020 This evidence review sets out the best available evidence on acute use of non- steroidal anti-inflammatory drugs (NSAIDs) for people with or at risk of COVID-19. It should be read in conjunction with the evidence summary, which gives the key messages. Evidence review commissioned by NHS England Disclaimer The content of this evidence review was up-to-date on 24 March 2020. See summaries of product characteristics (SPCs), British national formulary (BNF) or the MHRA or NICE websites for up-to-date information. For details on the date the searches for evidence were conducted see the search strategy. Copyright © NICE 2020. All rights reserved. Subject to Notice of rights. ISBN: 978-1-4731-3763-9 Contents Contents ...................................................................................................... 1 Background ................................................................................................. 2 Intervention .................................................................................................. 2 Clinical problem ........................................................................................... 3 Objective ...................................................................................................... 3 Methodology ................................................................................................ 4 Summary of included studies -

Anti-Inflammatory Pain Powders Page: 1 of 5
Federal Employee Program® 1310 G Street, N.W. Washington, D.C. 20005 202.942.1000 Fax 202.942.1125 5.70.26 Section: Prescription Drugs Effective Date: April 1, 2020 Subsection: Analgesics and Anesthetics Original Policy Date: June 20, 2013 Subject: Anti-Inflammatory Pain Powders Page: 1 of 5 Last Review Date: March 13, 2020 Anti-Inflammatory Pain Powders Description Celecoxib Powder, Diclofenac Powder, Fenoprofen Powder, Flurbiprofen Powder, Ibuprofen Powder, Ketoprofen Powder, Meloxicam Powder, Naproxen Powder, Tramadol Powder Background Pharmacy compounding is an ancient practice in which pharmacists combine, mix or alter ingredients to create unique medications that meet specific needs of individual patients. Some examples of the need for compounding products would be: the dosage formulation must be changed to allow a person with dysphagia (trouble swallowing) to have a liquid formulation of a commercially available tablet only product, or to obtain the exact strength needed of the active ingredient, to avoid ingredients that a particular patient has an allergy to, or simply to add flavoring to medication to make it more palatable. Celecoxib, diclofenac, fenoprofen, flurbiprofen, ibuprofen, ketoprofen, meloxicam, and naproxen are non-steroidal anti-inflammatory drugs (NSAID) that decrease inflammation, pain and fever by inhibiting COX-1 and 2 enzymes, which then inhibit the production of prostaglandins and leukotrienes (1-7). Tramadol is a centrally acting synthetic opioid analgesic used to treat moderate to moderately severe chronic -

Utah Medicaid Pharmacy and Therapeutics Committee Drug
Utah Medicaid Pharmacy and Therapeutics Committee Drug Class Review Non-Selective Oral Nonsteroidal Anti-Inflammatory Drugs AHFS Classification: 28:08.04.92 Other Nonsteroidal Anti-inflammatory Agents Diclofenac Etodolac Fenoprofen Flurbiprofen Ibuprofen Indomethacin Ketoprofen Ketorolac Mefenamic Acid Meloxicam Nabumetone Naproxen Oxaprozin Piroxicam Sulindac Tolmetin Final Report April 2018 Review prepared by: Elena Martinez Alonso, B.Pharm., Medical Writer Vicki Frydrych, B.Pharm., Pharm.D., Clinical Pharmacist Valerie Gonzales, Pharm.D., Clinical Pharmacist Joanita Lake, B.Pharm., MSc EBHC (Oxon), Research Assistant Professor, Clinical Pharmacist Michelle Fiander, MA, MLIS, Research Assistant Professor, Evidence Synthesis Librarian Joanne LaFleur, PharmD, MSPH, Associate Professor University of Utah College of Pharmacy University of Utah College of Pharmacy, Drug Regimen Review Center Copyright © 2018 by University of Utah College of Pharmacy Salt Lake City, Utah. All rights reserved 1 Contents Executive Summary ...................................................................................................................................... 3 Introduction ................................................................................................................................................... 6 Table 1. FDA-Approved Oral Non-selective NSAIDs......................................................................... 7 Table 2. FDA-Approved Indication for Oral Non-selective NSAIDs ............................................... -

Four New Anti-Inflammatory Drugs: Responses and Variations
1048 BRITISH MEDICAL JOURNAL 1 MAY 1976 The final place of labetalol for hypertension must await the 3 Frohlich, E D, et al, Circulation, 1968, 37, 417. results of forthcoming comparative studies. Our data indicate 4 Hansson, L, et al, Klinische Wochenschrift, 1972, 50, 364. s Somer, T, Luomanmaki, K, and Frick, M H, Acta Medica Scandinavica, Br Med J: first published as 10.1136/bmj.1.6017.1048 on 1 May 1976. Downloaded from that it is well suited for treating mild and moderate hypertension, 1974, suppl No 554, p 33. in which we restored the blood pressure to normal in 75o, of 6 Furberg, C, et al, Acta Medica Scandinavica, 1969, 186, 447. patients with a dose of 200 mg thrice daily. Evident advantages 7 Lydtin, H, et al, American HeartJournal, 1972, 83, 589. substances include safer use in patients 8 Prichard, B N C, et al, British Heart Journal, 1970, 32, 236. over pure beta-blocking 9 Hansson, L, et al, Acta Medica Scandinavica, 1974, 196, 27. with initial bradycardia; in patients with atrioventricular con- 10 Tarazi, R C, and Dustan, H P, American Journal of Cardiology, 1972, 29, duction disturbances; and in asthmatics, who do not exhibit 633. bronchoconstriction when on labetalol.18 1 Farmer, J B, et al, British Journal of Pharmacology, 1972, 45, 660. 12 Kennedy, I, and Levy, G P, BritishJournal of Pharmacology, 1975, 53, 585. 13 Richards, D A, et al, British3Journal of Clinical Pharmacology, 1974, 1, 505. 14 Collier, J G, et al, British Journal of Pharmacology, 1972, 44, 286. References 15 Katila, M, and Frick, M H, InternationalJouirnal of Clinical Pharmacology, Therapy and Toxicology, 1970, 4, 111. -

Indocin® (Indomethacin) Oral Suspension
INDOCIN® (INDOMETHACIN) ORAL SUSPENSION Cardiovascular Risk • NSAIDs may cause an increased risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at a greater risk. (See WARNINGS.) • INDOCIN is contraindicated for the treatment of peri-operative pain in the setting of coronary artery bypass graft (CABG) surgery (see WARNINGS). Gastrointestinal Risk • NSAIDs cause an increased risk of serious gastrointestinal adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events. (See WARNINGS.) DESCRIPTION Suspension INDOCIN1 for oral use contains 25 mg of indomethacin per 5 mL, alcohol 1%, and sorbic acid 0.1% added as a preservative and the following inactive ingredients: antifoam AF emulsion, flavors, purified water, sodium hydroxide or hydrochloric acid to adjust pH, sorbitol solution, and tragacanth. Indomethacin is a non-steroidal anti-inflammatory indole derivative designated chemically as 1-(4-chlorobenzoyl)-5-methoxy-2-methyl-1H-indole-3-acetic acid. 1 Indomethacin is practically insoluble in water and sparingly soluble in alcohol. It has a pKa of 4.5 and is stable in neutral or slightly acidic media and decomposes in strong alkali. The suspension has a pH of 4.0-5.0. The structural formula is: 1 Registered trademark of MERCK & CO., Inc., Whitehouse Station, NJ U.S.A. and licensed to Iroko Pharmaceuticals, LLC, Philadelphia, PA, U.S.A. -

NDA 17-604/S-040 Page 3 NALFON (Fenoprofen Calcium Capsules, USP)
NDA 17-604/S-040 Page 3 NALFON® (fenoprofen calcium capsules, USP) 200 mg & 300mg Rx only Cardiovascular Risk • NSAIDs may cause an increased risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk (See WARNINGS). •Nalfon® is contraindicated for the treatment of peri-operative pain in the setting of coronary artery bypass graft (CABG) surgery (see WARNINGS). Gastrointestinal Risk • NSAIDs cause an increased risk of serious gastrointestinal adverse events including bleeding, ulceration, and perforation of stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events (see WARNINGS). DESCRIPTION Nalfon® (Fenoprofen Calcium Capsules, USP) is a nonsteroidal, anti-inflammatory, antiarthritic drug. Nalfon capsules contain fenoprofen calcium as the dihydrate in an amount equivalent to 200 mg (0.826 mmol) or 300 mg (1.24 mmol) of fenoprofen. The capsules also contain cellulose, gelatin, iron oxides, silicone, titanium dioxide, and other inactive ingredients. The 300 mg capsules also contain D & C Yellow No. 10 and F D & C Yellow No. 6. Chemically, Nalfon is an arylacetic acid derivative. The structural formula is as follows: Benzeneacetic acid, α-methyl-3-phenoxy-, calcium salt dihydrate, (±)- Nalfon is a white crystalline powder that has the structural formula C30H26CaO6•2H2O representing a molecular weight of 558.65. At 25°C, it dissolves to a 15 mg/mL solution in alcohol (95%). -
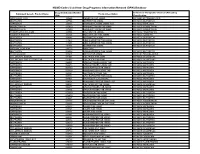
NSAID Codes Used from Drug Programs Information Network (DPIN) Database
NSAID Codes Used from Drug Programs Information Network (DPIN) Database Drug Identification Number Anatomical Therapeutic Chemical (ATC) Drug Equivalent Generic Product Name Product Description (DIN) Classification MEFENAMIC ACID 155225 PONSTAN CAP 250MG M01AG01 MEFENAMIC ACID IBUPROFEN 327794 MOTRIN TAB 300MG M01AE01 IBUPROFEN NAPROXEN 335193 NAPROSYN 250MG 250MG TAB M01AE02 NAPROXEN INDOMETHACIN 337420 NOVO-METHACIN CAP 25MG M01AB01 INDOMETACIN INDOMETHACIN 337439 NOVO-METHACIN CAP 50MG M01AB01 INDOMETACIN FENOPROFEN CALCIUM 345504 NALFON TAB 600MG M01AE04 FENOPROFEN TOLMETIN SODIUM 364126 TOLECTIN 200 TAB 200MG M01AB03 TOLMETIN IBUPROFEN 364142 MOTRIN TAB 400MG M01AE01 IBUPROFEN IBUPROFEN 441643 APO IBUPROFEN TAB 200MG M01AE01 IBUPROFEN IBUPROFEN 441651 APO IBUPROFEN TAB 300MG M01AE01 IBUPROFEN IBUPROFEN 484911 MOTRIN TAB 600MG M01AE01 IBUPROFEN NAPROXEN SODIUM 491772 ANAPROX IBUPROFEN 506052 APO-IBUPROFEN TAB 400MG M01AE01 IBUPROFEN PENICILLAMINE 511641 DEPEN TAB 250MG M01CC01 PENICILLAMINE DICLOFENAC SODIUM 514004 VOLTAREN TAB 25MG M01AB05 DICLOFENAC DICLOFENAC SOD SR 75MG TAB 514012 VOLTAREN TAB 50MG M01AB05 DICLOFENAC NAPROXEN 522651 APO NAPROXEN 250MG TAB M01AE02 NAPROXEN NAPROXEN 522678 APO NAPROXEN 125MG TAB M01AE02 NAPROXEN NAPROXEN 565350 NOVO-NAPROX TAB 250MG M01AE02 NAPROXEN NAPROXEN 565369 NOVO-NAPROX 125MG TAB M01AE02 NAPROXEN NAPROXEN 583367 NAPROSYN 375MG TAB M01AE02 NAPROXEN IBUPROFEN 585114 APO IBUPROFEN TAB 600MG M01AE01 IBUPROFEN NAPROXEN 587923 NAPROSYN SUS 25MG/ML M01AE02 NAPROXEN NAPROXEN 589861 NOVO-NAPROX TAB