Pharmacogenetics of Nonsteroidal Anti-Inflammatory Drugs
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Use of Aspirin and Nsaids to Prevent Colorectal Cancer
Evidence Synthesis Number 45 Use of Aspirin and NSAIDs to Prevent Colorectal Cancer Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. 290-02-0021 Prepared by: University of Ottawa Evidence-based Practice Center at The University of Ottawa, Ottawa Canada David Moher, PhD Director Investigators Alaa Rostom, MD, MSc, FRCPC Catherine Dube, MD, MSc, FRCPC Gabriela Lewin, MD Alexander Tsertsvadze, MD Msc Nicholas Barrowman, PhD Catherine Code, MD, FRCPC Margaret Sampson, MILS David Moher, PhD AHRQ Publication No. 07-0596-EF-1 March 2007 This report is based on research conducted by the University of Ottawa Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. 290-02-0021). Funding was provided by the Centers for Disease Control and Prevention. The findings and conclusions in this document are those of the author(s), who are responsible for its content, and do not necessarily represent the views of AHRQ. No statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help clinicians, employers, policymakers, and others make informed decisions about the provision of health care services. This report is intended as a reference and not as a substitute for clinical judgment. This document is in the public domain and may be used and reprinted without permission except those copyrighted materials noted for which further reproduction is prohibited without the specific permission of copyright holders. -

Ticagrelor Antidote) by Mathematical Modeling
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Chalmers Publication Library Citation: CPT Pharmacometrics Syst. Pharmacol. (2016) 5, 313–323; doi:10.1002/psp4.12089 VC 2016 ASCPT All rights reserved ORIGINAL ARTICLE Unraveling the Pharmacokinetic Interaction of Ticagrelor and MEDI2452 (Ticagrelor Antidote) by Mathematical Modeling J Almquist1,2,3, M Penney4, S Pehrsson3, A-S Sandinge3, A Janefeldt3, S Maqbool4, S Madalli5, J Goodman4, S Nylander3 and P Gennemark3* The investigational ticagrelor-neutralizing antibody fragment, MEDI2452, is developed to rapidly and specifically reverse the antiplatelet effects of ticagrelor. However, the dynamic interaction of ticagrelor, the ticagrelor active metabolite (TAM), and MEDI2452, makes pharmacokinetic (PK) analysis nontrivial and mathematical modeling becomes essential to unravel the complex behavior of this system. We propose a mechanistic PK model, including a special observation model for post-sampling equilibration, which is validated and refined using mouse in vivo data from four studies of combined ticagrelor-MEDI2452 treatment. Model predictions of free ticagrelor and TAM plasma concentrations are subsequently used to drive a pharmacodynamic (PD) model that successfully describes platelet aggregation data. Furthermore, the model indicates that MEDI2452-bound ticagrelor is primarily eliminated together with MEDI2452 in the kidneys, and not recycled to the plasma, thereby providing a possible scenario for the extrapolation to humans. We anticipate the modeling work to improve PK and PD understanding, experimental design, and translational confidence. CPT Pharmacometrics Syst. Pharmacol. (2016) 5, 313–323; doi:10.1002/psp4.12089; published online 16 June 2016. Study Highlights WHAT IS THE CURRENT KNOWLEDGE ON THE WHAT THIS STUDY ADDS TO OUR KNOWLEDGE TOPIC? þ A mathematical model describing the simultaneous þ Antiplatelet therapy for the prevention of athero- PKs of ticagrelor and MEDI2452 in the mouse is pre- thrombotic events in patients with acute coronary syn- sented. -
Lumiracoxib: Suspension of UK Licences with Immediate Effect (Non
Primary and Community Care Directorate Pharmacy Division T: 0131-244 2528 F: 0131-244 2375 E: [email protected] abcdefghijklmnopqrstu 19 November 2007 ___ 1. Medical Directors NHS Boards 2. Directors of Public Health 3. Specialists in Pharmaceutical Public Health/Directors of Pharmacy 4. NHS 24 LUMIRACOXIB – SUSPENSION OF UK LICENCES WITH IMMEDIATE EFFECT (NON URGENT ) CASCADE WITHIN 48 HOURS Please see attached for onward transmission a copy of a message from Professor Gordon Duff, Chairman, Commission on Human Medicines about the suspension of UK licences (marketing authorisations) due to the risk of severe liver reactions associated with lumiracoxib. Please could Medical Directors in NHS Boards forward on to :- ● All General Practitioners - please ensure this message is seen by all practice nurses and non principals working in your practice and retain a copy in your ‘locum information pack’. ● Deptutising services Please could all Directors of Public Health forward the message to: ● Chief Executives NHS Boards Specialists in Pharmaceutical Public Health/Directors of Pharmacy will also receive this information through the usual drug alert channels to forward on to community pharmacists. Yours sincerely PAMELA WARRINGTON Deputy Chief Pharmaceutical Officer St Andrew’s House, Regent Road, Edinburgh EH1 3DG www.scotland.gov.uk abcde abc a Ref: EL(07)A/21 LUMIRACOXIB - SUSPENSION OF UK LICENCES WITH IMMEDIATE EFFECT 19 November 2007 Dear Colleague, I am writing to inform you that the UK licences (marketing authorisations) for lumiracoxib have been suspended and stocks are being withdrawn from pharmacies, on the basis of advice from the Commission on Human Medicines (CHM). -

Cytochrome P450 Enzymes in Oxygenation of Prostaglandin Endoperoxides and Arachidonic Acid
Comprehensive Summaries of Uppsala Dissertations from the Faculty of Pharmacy 231 _____________________________ _____________________________ Cytochrome P450 Enzymes in Oxygenation of Prostaglandin Endoperoxides and Arachidonic Acid Cloning, Expression and Catalytic Properties of CYP4F8 and CYP4F21 BY JOHAN BYLUND ACTA UNIVERSITATIS UPSALIENSIS UPPSALA 2000 Dissertation for the Degree of Doctor of Philosophy (Faculty of Pharmacy) in Pharmaceutical Pharmacology presented at Uppsala University in 2000 ABSTRACT Bylund, J. 2000. Cytochrome P450 Enzymes in Oxygenation of Prostaglandin Endoperoxides and Arachidonic Acid: Cloning, Expression and Catalytic Properties of CYP4F8 and CYP4F21. Acta Universitatis Upsaliensis. Comprehensive Summaries of Uppsala Dissertations from Faculty of Pharmacy 231 50 pp. Uppsala. ISBN 91-554-4784-8. Cytochrome P450 (P450 or CYP) is an enzyme system involved in the oxygenation of a wide range of endogenous compounds as well as foreign chemicals and drugs. This thesis describes investigations of P450-catalyzed oxygenation of prostaglandins, linoleic and arachidonic acids. The formation of bisallylic hydroxy metabolites of linoleic and arachidonic acids was studied with human recombinant P450s and with human liver microsomes. Several P450 enzymes catalyzed the formation of bisallylic hydroxy metabolites. Inhibition studies and stereochemical analysis of metabolites suggest that the enzyme CYP1A2 may contribute to the biosynthesis of bisallylic hydroxy fatty acid metabolites in adult human liver microsomes. 19R-Hydroxy-PGE and 20-hydroxy-PGE are major components of human and ovine semen, respectively. They are formed in the seminal vesicles, but the mechanism of their biosynthesis is unknown. Reverse transcription-polymerase chain reaction using degenerate primers for mammalian CYP4 family genes, revealed expression of two novel P450 genes in human and ovine seminal vesicles. -

Clopidogrel Compared with Other Antiplatelet Agents For
Canadian Agency for Agence canadienne Drugs and Technologies des médicaments et des in Health technologies de la santé CADTH Technology Report Issue 131 Clopidogrel Compared with Other Antiplatelet November 2010 Agents for Secondary Prevention of Vascular Events in Adults Undergoing Percutaneous Coronary Intervention: Clinical and Cost-Effectiveness Analyses Supporting Informed Decisions Until April 2006, the Canadian Agency for Drugs and Technologies in Health (CADTH) was known as the Canadian Coordinating Office for Health Technology Assessment (CCOHTA). Publications can be requested from: CADTH 600-865 Carling Avenue Ottawa ON Canada K1S 5S8 Tel: 613-226-2553 Fax: 613-226-5392 Email: [email protected] or downloaded from CADTH’s website: http://www.cadth.ca Cite as: Chen SY, Russell E, Banerjee S, Hutton B, Brown A, Asakawa K, McGahan L, Clark M, Severn M, Cox J, Sharma M. Clopidogrel Compared with Other Antiplatelet Agents for Secondary Prevention of Vascular Events in Adults Undergoing Percutaneous Coronary Intervention: Clinical and Cost-Effectiveness Analyses [Internet]. Ottawa: Canadian Agency for Drugs and Technologies in Health; 2010 (Technology report; no. 131). [cited 2010-11-01]. Available from: http://www.cadth.ca/preview.php/en/publication/2708 Production of this report is made possible by financial contributions from Health Canada and the governments of Alberta, British Columbia, Manitoba, New Brunswick, Newfoundland and Labrador, Northwest Territories, Nova Scotia, Nunavut, Prince Edward Island, Saskatchewan, and Yukon. The Canadian Agency for Drugs and Technologies in Health takes sole responsibility for the final form and content of this report. The views expressed herein do not necessarily represent the views of Health Canada or any provincial or territorial government. -

Salsalate Tablets, USP 500 Mg and 750 Mg Rx Only
SALSALATE RX- salsalate tablet, film coated ANDAPharm LLC Disclaimer: This drug has not been found by FDA to be safe and effective, and this labeling has not been approved by FDA. For further information about unapproved drugs, click here. ---------- Salsalate Tablets, USP 500 mg and 750 mg Rx Only Cardiovascular Risk NSAIDs may cause an increase risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk. (See WARNINGS and CLINICAL TRIALS). Salsalate tablets, USP is contraindicated for the treatment of perioperative pain in the setting of coronary artery bypass graft (CABG) surgery (See WARNINGS). Gastrointestinal Risk NSAIDs cause an increased risk of serious gastrointestinal adverse events including bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events. (See WARNINGS). DESCRIPTION Salsalate, is a nonsteroidal anti-inflammatory agent for oral administration. Chemically, salsalate (salicylsalicylic acid or 2-hydroxybenzoic acid, 2-carboxyphenyl ester) is a dimer of salicylic acid; its structural formula is shown below. Chemical Structure: Inactive Ingredients: Colloidal Silicon Dioxide, D&C Yellow #10 Aluminum Lake, Hypromellose, Microcrystalline Cellulose, Sodium Starch Glycolate, Stearic Acid, Talc, Titanium Dioxide, Triacetin. CLINICAL PHARMACOLOGY Salsalate is insoluble in acid gastric fluids (<0.1 mg/mL at pH 1.0), but readily soluble in the small intestine where it is partially hydrolyzed to two molecules of salicylic acid. -
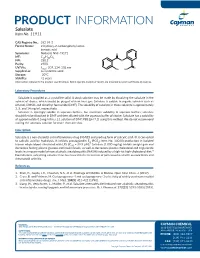
Download Product Insert (PDF)
PRODUCT INFORMATION Salsalate Item No. 11911 CAS Registry No.: 552-94-3 Formal Name: 2-hydroxy-2-carboxyphenyl ester- benzoic acid Synonyms: Nobacid, NSC 49171 O MF: C14H10O5 FW: 258.2 O Purity: ≥98% UV/Vis.: λ: 207, 234, 308 nm O max OH HO Supplied as: A crystalline solid Storage: -20°C Stability: ≥2 years Information represents the product specifications. Batch specific analytical results are provided on each certificate of analysis. Laboratory Procedures Salsalate is supplied as a crystalline solid. A stock solution may be made by dissolving the salsalate in the solvent of choice, which should be purged with an inert gas. Salsalate is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide (DMF). The solubility of salsalate in these solvents is approximately 3, 5, and 14 mg/ml, respectively. Salsalate is sparingly soluble in aqueous buffers. For maximum solubility in aqueous buffers, salsalate should first be dissolved in DMF and then diluted with the aqueous buffer of choice. Salsalate has a solubility of approximately 0.5 mg/ml in a 1:1 solution of DMF:PBS (pH 7.2) using this method. We do not recommend storing the aqueous solution for more than one day. Description Salsalate is a non-steroidal anti-inflammatory drug (NSAID) and prodrug form of salicylic acid.1 It is converted to salicylic acid by hydrolysis. It inhibits prostaglandin E2 (PGE2; Item No. 14010) production in isolated 2 human whole blood stimulated with LPS (IC50 = 39.9 µM). Salsalate (1,000 mg/kg) inhibits weight gain and decreases fasting plasma glucose and insulin levels, as well as decreases plasma cholesterol and triglyceride levels in a mouse model of non-alcoholic steatohepatitis (NASH) induced by a high-fat high-cholesterol diet.3 Formulations containing salsalate have been used in the treatment of pain associated with osteoarthritis and rheumatoid arthritis. -

Nsaids: Dare to Compare 1997
NSAIDs TheRxFiles DARE TO COMPARE Produced by the Community Drug Utilization Program, a Saskatoon District Health/St. Paul's Hospital program July 1997 funded by Saskatchewan Health. For more information check v our website www.sdh.sk.ca/RxFiles or, contact Loren Regier C/O Pharmacy Department, Saskatoon City Hospital, 701 Queen St. Saskatoon, SK S7K 0M7, Ph (306)655-8506, Fax (306)655-8804; Email [email protected] We have come a long way from the days of willow Highlights bark. Today salicylates and non-steroidal anti- • All NSAIDs have similar efficacy and side inflammatory drugs (NSAIDs) comprise one of the effect profiles largest and most commonly prescribed groups of • In low risk patients, Ibuprofen and naproxen drugs worldwide.1 In Saskatchewan, over 20 may be first choice agents because they are different agents are available, accounting for more effective, well tolerated and inexpensive than 300,000 prescriptions and over $7 million in • Acetaminophen is the recommended first line sales each year (Saskatchewan Health-Drug Plan agent for osteoarthritis data 1996). Despite the wide selection, NSAIDs • are more alike than different. Although they do Misoprostol is the only approved agent for differ in chemical structure, pharmacokinetics, and prophylaxis of NSAID-induced ulcers and is to some degree pharmacodynamics, they share recommended in high risk patients if NSAIDS similar mechanisms of action, efficacy, and adverse cannot be avoided. effects. week or more to become established. For this EFFICACY reason, an adequate trial of 1-2 weeks should be NSAIDs work by inhibiting cyclooxygenase (COX) allowed before increasing the dose or changing to and subsequent prostaglandin synthesis as well as another NSAID. -

Efficacy of Etoricoxib, Celecoxib, Lumiracoxib, Non-Selective Nsaids, and Acetaminophen in Osteoarthritis: a Mixed Treatment Comparison W.B
6 The Open Rheumatology Journal, 2012, 6, 6-20 Open Access Efficacy of Etoricoxib, Celecoxib, Lumiracoxib, Non-Selective NSAIDs, and Acetaminophen in Osteoarthritis: A Mixed Treatment Comparison W.B. Stam1, J.P. Jansen2 and S.D. Taylor*,3 1Mapi Group, Houten, The Netherlands 2Mapi Group, Boston, MA, USA 3Merck & Co., Inc., Whitehouse Station, NJ, USA Abstract: Objective: To compare the efficacy of etoricoxib, lumiracoxib, celecoxib, non-selective (ns) NSAIDs and acetaminophen in the treatment of osteoarthritis (OA) Methods: Randomized placebo controlled trials investigating the effects of acetaminophen 4000mg, diclofenac 150mg, naproxen 1000mg, ibuprofen 2400mg, celecoxib 100-400mg, lumiracoxib 100-400mg, and etoricoxib 30-60mg with treatment duration of at least two weeks were identified with a systematic literature search. The endpoints of interest were pain, physical function and patient global assessment of disease status (PGADS). Pain and physical function reported on different scales (VAS or LIKERT) were translated into effect sizes (ES). An ES 0.2 - 0.5 was defined as a “small” treatment effect, whereas ES of 0.5 – 0.8 and > 0.8 were defined as “moderate” and “large”, respectively. A negative effect indicated superior effects of the treatment group compared to the control group. Results of all trials were analyzed simultaneously with a Bayesian mixed treatment comparison. Results: There is a >95% probability that etoricoxib (30 or 60mg) shows the greatest improvement in pain and physical function of all interventions compared. ESs of etoricoxib 30mg relative to placebo, celecoxib 200mg, ibuprofen 2400mg, and diclofenac 150mg were -0.66 (95% Credible Interval -0.83; -0.49), -0.32 (-0.50; -0.14), -0.25 (-0.53; 0.03), and -0.17 (-0.41; 0.08), respectively. -

Acute Renal Failure Associated with Diflunisal J. G. WHARTON D. 0
Postgrad Med J: first published as 10.1136/pgmj.58.676.104 on 1 February 1982. Downloaded from Postgraduate Medical Journal (February 1982) 58, 104-105 Acute renal failure associated with diflunisal J. G. WHARTON D. 0. OLIVER B.Sc., M.R.C.P. F.R.C.P., F.R.A.C.P. M. S. DUNNILL F.R.C.P., F.R.C.Path. Renal Unit, Churchill Hospital, and Department of Pathology, John Radcliffe Hospital, Oxford Summary eosinophils 224 x 106/1; ESR 30 mm/hr; urea 305 The case of a 44-year-old man with acute oliguric mmol/l; creatinine 1651 ,Lmol/l; potassium 6-43 renal failure due to tubulo-interstitial nephritis after mmol/l; serum amylase 88 Somogyi units; urine 3 months' diflunisal is reported. The possible mecha- contained no casts; no red cells but 10 neutrophils, nisms are discussed. no eosinophils and no growth. Antistreptolysin 0 titre 50 i.u./ml; IgG 16-5 g/l; IgA 3-8 g/l; IgM 1.1 g/l antinuclear factor negative; C3 122 mg/dl, C4 54Protected by copyright. Introduction mg/dl; hepatitis B surface antigen negative; chest Diflunisal has been reported as causing acute radiograph, cardiomegaly plus congestion; intra- allergic interstitial nephritis (Chan et al., 1980) venous urogram with tomograms, no obstruction, resulting in acute oliguric renal failure. A case of poor nephrogram. A renal biopsy showed tubulo- acute renal failure due to tubulo-interstitial nephritis interstitial nephritis with no eosinophil infiltrate. after 3 months of diflunisal is reported here. Recently, Diflunisal had been stopped 2 days before admission phenylakalonic acids with analgesic and anti- to this renal unit. -
Multifactorial Background for a Low Biological Response to Antiplatelet Agents Used in Stroke Prevention
medicina Review Multifactorial Background for a Low Biological Response to Antiplatelet Agents Used in Stroke Prevention Adam Wi´sniewski Department of Neurology, Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University in Toru´n, Skłodowskiej 9 Street, 85-094 Bydgoszcz, Poland; [email protected]; Tel.: +48-79-0813513 Abstract: Effective platelet inhibition is the main goal of the antiplatelet therapy recommended as a standard treatment in the secondary prevention of non-embolic ischemic stroke. Acetylsalicylic acid (aspirin) and clopidogrel are commonly used for this purpose worldwide. A low biological response to antiplatelet agents is a phenomenon that significantly reduces the therapeutic and protective properties of the therapy. The mechanisms leading to high on-treatment platelet reactivity are still unclear and remain multifactorial. The aim of the current review is to establish the background of resistance to antiplatelet agents commonly used in the secondary prevention of ischemic stroke and to explain the possible mechanisms. The most important factors influencing the incidence of a low biological response were demonstrated. The similarities and the differences in resistance to both drugs are emphasized, which may facilitate the selection of the appropriate antiplatelet agent in relation to specific clinical conditions and comorbidities. Despite the lack of indications for the routine assessment of platelet reactivity in stroke subjects, this should be performed in selected patients from the high-risk group. Increasing the detectability of low antiaggregant responders, in light of its negative impact on the prognosis and clinical outcomes, can contribute to a more individualized approach and modification of the antiplatelet therapy to maximize the therapeutic effect in the secondary prevention of stroke. -

Salicylate, Diflunisal and Their Metabolites Inhibit CBP/P300 and Exhibit Anticancer Activity
RESEARCH ARTICLE Salicylate, diflunisal and their metabolites inhibit CBP/p300 and exhibit anticancer activity Kotaro Shirakawa1,2,3,4, Lan Wang5,6, Na Man5,6, Jasna Maksimoska7,8, Alexander W Sorum9, Hyung W Lim1,2, Intelly S Lee1,2, Tadahiro Shimazu1,2, John C Newman1,2, Sebastian Schro¨ der1,2, Melanie Ott1,2, Ronen Marmorstein7,8, Jordan Meier9, Stephen Nimer5,6, Eric Verdin1,2* 1Gladstone Institutes, University of California, San Francisco, United States; 2Department of Medicine, University of California, San Francisco, United States; 3Department of Hematology and Oncology, Kyoto University, Kyoto, Japan; 4Graduate School of Medicine, Kyoto University, Kyoto, Japan; 5University of Miami, Gables, United States; 6Sylvester Comprehensive Cancer Center, Miami, United States; 7Perelman School of Medicine, University of Pennsylvania, Philadelphia, United States; 8Department of Biochemistry and Biophysics, Abramson Family Cancer Research Institute, Philadelphia, United States; 9Chemical Biology Laboratory, National Cancer Institute, Frederick, United States Abstract Salicylate and acetylsalicylic acid are potent and widely used anti-inflammatory drugs. They are thought to exert their therapeutic effects through multiple mechanisms, including the inhibition of cyclo-oxygenases, modulation of NF-kB activity, and direct activation of AMPK. However, the full spectrum of their activities is incompletely understood. Here we show that salicylate specifically inhibits CBP and p300 lysine acetyltransferase activity in vitro by direct *For correspondence: everdin@ competition with acetyl-Coenzyme A at the catalytic site. We used a chemical structure-similarity gladstone.ucsf.edu search to identify another anti-inflammatory drug, diflunisal, that inhibits p300 more potently than salicylate. At concentrations attainable in human plasma after oral administration, both salicylate Competing interests: The and diflunisal blocked the acetylation of lysine residues on histone and non-histone proteins in cells.