The Pediatric Dentist's Role in Sleep Disordered Breathing and Myofunctional Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Feline Dentistry: Cats Are Not Small Dogs Matt Lemmons, DVM, DAVDC Medvet Indianapolis Carmel, IN
Basics for Practitioners: Oral Anatomy and Pathology Matt Lemmons, DVM, DAVDC MedVet Indianapolis Carmel, IN Dentistry is truly a branch of medicine and surgery. A strong knowledge of normal anatomy and pathology is cornerstone to adequate diagnosis and treatment of diseases of the oral cavity. The majority of oral related disease is inflammatory (periodontal disease) or traumatic (fractured teeth, orthopedic injuries) in nature. However other causes are not rare and need to be recognized. The basic dental unit is the tooth and surrounding periodontium. The tooth consists of the crown and root. The crown is covered in enamel and the root by cementum. Deep to the crown and cementum is the dentin. Dentin is a porous hard tissue which continuously grows toward the center of the tooth as long as the tooth is vital. Deep to the dentin is the pulp which consists of nerves, blood vessels, connective tissue, fibroblasts and odontoblasts. The periodontium is composed of the cementum, periodontal ligament, alveolar bone, and gingiva. The periodontal ligament serves to anchor the cementum to the alveolar bone, act as a shock absorber and aid in sensation. The gingiva is attached to the bone (attached gingiva), tooth by connective tissue and the most apical extent is not attached and is known as the free gingiva. The potential space between the free gingiva and tooth and ending apically at the sulcular epithelium is the gingival sulcus. In health this should be less than 3mm in depth in dogs and 1mm in cats. When addressing the teeth and periodontium, directional nomenclature is not similar to directional nomenclature of the rest of the body. -

II. DIGESTIV SYSTEM TESTS General Data 1. CS the Organ Represent: A
II. DIGESTIV SYSTEM TESTS General data 1. CS The organ represent: a) a structure made up by three layers b) a hollow element c) a part of the body built by complex of tissues integrated to realize the common functions d) a parenchymatous formation located in abdominal cavity e) a formation constituted by epithelium, vessels and nerves 2. CS The visceral apparatus is considered: a) The organs of different systems with diverse structure involved in performing some functions. b) the organs of neck region c) the organs located in the lesser pelvis d) the organs realized protective function e) the organs located at the border between thoracic and abdominal cavities 3. CS The primary gut is developed from: a) ectoderm b) mesoderm c) endoderm d) dermatome e) myotome 4. CS From which embryonic layer is developed the primary intestine : a) entoderm b) ectoderm c) sclerotome d) mesoderm e) splanhnopleura 5. CM The Viscera represents: a) the organs localized in abdominal cavity b) the systems of organs realized the connection of the body and external environment c) the organs and system of organs located in body’s cavities which realized the metabolic functions to sustain the life d) the complex of organs from abdominal and pelvic cavities e) the complex of organs from thoracic cavity 6. CM According by structure the organs are divided in: a) serous b) parenchymatous c) glandular d) epithelial e) hollow 7. CM Name two functions of the organic stroma: a) secretory b) trophic c) hematopoietic d) metabolic e) sustaining 8. CM The hollow organs distinguish the following layers: a) mucous b) submucous c) muscular d) membranous e) serous 9. -
Anatomic Landmarks in a Maxillary and Mandibular Ridge
International Journal of Applied Dental Sciences 2017; 3(2): 26-29 ISSN Print: 2394-7489 ISSN Online: 2394-7497 IJADS 2017; 3(2): 26-29 Anatomic landmarks in a maxillary and mandibular © 2017 IJADS www.oraljournal.com ridge - A clinical perspective Received: 18-02-2017 Accepted: 19-03-2017 Mohd. Azeem, Ashraf Mujtaba, Shrestha Subodh, Ahmad Naeem, Gaur Mohd. Azeem PG Student, Department of Abhishek and Pandey Kaushik Kumar Prosthodontics, Career Post Graduate Institute of Dental Abstract Sciences, Lucknow, A thorough knowledge of oral anatomy helps the clinician in identifying enough landmarks that in turn Uttar Pradesh, India act as positive guides in treatment planning. In the present article, a review of all the intraoral anatomical landmarks is been presented and analyzed Ashraf Mujtaba PG Student, Department of Prosthodontics, Career Post Keywords: Maxillary ridge, Mandibular ridge, Edentulism, Anatomical landmarks Graduate Institute of Dental Sciences, Lucknow, Introduction Uttar Pradesh, India Literature Review: A total of 43 articles were downloaded & analyzed using the following mesh words maxillary ridge, mandibular ridge, edentulism & anatomical landmarks searching Shrestha Subodh PG Student, Department of pubmed & science direct data bases. 08 articles were finally selected and examined as per the Prosthodontics, Career Post requirement of the present review article on anatomic landmarks in a maxillary and Graduate Institute of Dental mandibular ridge - A clinical perspective. Sciences, Lucknow, In a Maxillary Arch, following anatomic Landmarks are present; Uttar Pradesh, India Incisive Papilla: It is a pad of fibrous connective tissue overlying the orifice of the Ahmad Naeem Reader, Department of nasopalatine canal. Prosthodontics, Career Post Graduate Institute of Dental Significance: Stable landmark and gives its relation to incisive foramen through which the Sciences, Lucknow, neurovascular bundle emerge and lie on the surface of bone. -

DHE121 Lesson Objectives
Instructional Objectives for DHE121 Identify the following anatomical structures and terms: Parotid Papilla Canine Eminence Parotid Duct or Stenson’s Duct Primary Teeth Maxilla Permanent Teeth Mandible Anterior Teeth Maxillary Sinuses or Paranasal Sinuses Posterior Teeth Alveolar Process or Bone Incisors Maxillary or Mandibular Vestibule Canines Buccal, Labial, and Alveolar Mucosa Premolars Vestibular Fornix Molars Mucobuccal Fold Exostoses Labial Frenum Pulp Cavity Alveolus Torus or Tori Periodontal Ligament (PDL) Gingiva Crown of a Tooth Attached Gingiva Root of a Tooth Alveolar Mucosa Enamel Mucogingival Junction Dentin Marginal Gingiva Cementum Gingival Sulcu Maxillary or Mandibular Tuberosity Interdental Gingiva or Papilla Fordyce Spots Fauces Linea Alba Anterior and Posterior Tonsillar Pillar Retromolar Pad Palatine Tonsils Palate Hard and Soft Median Palatine Raphe Incisive Papilla Palatine Rugae Uvula of the Palate Pterygomandibular Fold or Raphe Base of the Tongue Body of the Tongue Apex of the Tongue Lingual Papillae Dorsal Surface of the Tongue Median Lingual Sulcus of the Tongue Filiform Lingual Papillae Fungiform Lingual Papillae Sulcus Terminalis of the Tongue Foramen Cecum Circumvallate Lingual Papillae Lingual Tonsil Lateral Surface of the Tongue Foliate Lingual Papillae Ventral Surface of the Tongue Plicae Fimbriata Lingual Frenum Sublingual Fold Sublingual Salivary Gland Sublingual Caruncle Submandibular Duct (Wharton’s Duct) Sublingual Duct (Bartholin’s Duct) Laryngopharynx Nasopharynx Oropharynx Facial or Labial Anterior Buccal Posterior Palatal Frenum Lingual Dorsal Vestibules Oral Mucosa or Mucous Membrane Mastication DHE121 ORAL CAVITY 1. Describe the boundaries of the oral cavity. 2. Cite the two parts of the oral cavity. 3. Define: vestibule oral cavity proper mucobuccal fold frenum alveolar mucosa gingiva exotoses palatine tori (torus palatinis) mandibular tori (torus mandibularis) 4. -

Influence of Non-Orthodontic Intervention on Digit Sucking and Consequent Anterior Open Bite: a Preliminary Study
International Dental Journal SCIENTIFIC RESEARCH REPORT doi: 10.1111/idj.12178 Influence of non-orthodontic intervention on digit sucking and consequent anterior open bite: a preliminary study Boyen Huang1, Carla Lejarraga2, Christopher S. Franco3, Yunlong Kang4, Andrew Lee3, John Abbott3, Katsu Takahashi5, Kazuhisa Bessho5 and Pongthorn Pumtang-on6 1School of Dentistry and Health Sciences, Charles Sturt University, Orange, NSW, Australia; 2Thumbsucking Clinic, Townsville, QLD, Australia; 3School of Medicine and Dentistry, James Cook University, Cairns, QLD, Australia; 4Department of Orthodontics, Melbourne Dental School, the University of Melbourne, Melbourne, VIC, Australia; 5Department of Oral and Maxillofacial Surgery, Graduate School of Medicine, Kyoto University, Kyoto, Japan; 6School of Biomedical Sciences, Charles Sturt University, Wagga Wagga, NSW, Australia. Objectives: This study aimed to assess behavioural and occlusal outcomes of non-orthodontic intervention (NOI) in a sample of children, 4–12 years of age, in Australia, in order to establish clinical relevance. Materials and methods: Data from 91 patient records of 4- to 12-year-old children reporting a habit of digit sucking, from two clinics in north-eastern Australia, were de-identified and used. Each patient had been examined at two visits, separated by an interval of 4 months, using standard clinical procedures. Results: Of the 77 children who received a 4-month NOI, 69 (89.6%) had ceased their digit sucking habit by the end of the NOI period [v2 = 67.0, degrees of freedom (d.f.) = 1, P < 0.001]. Of the 72 subjects who had front teeth, the number with anterior open bite decreased from 37 (51.4%) to 12 (16.7%) upon completion of NOI (v2 = 21.3, d.f. -

Oral Cancer Screening: Let Your Fingers Do the Talking Lesion Descriptor Guide*
Oral Cancer Screening: Let your fingers do the talking Lesion Descriptor Guide* Anatomic Locations HEAD: scalp, eye, ear, nose, cheek, chin, neck; R or L NECK: midline, right, left, near certain anatomic structure LIP: Max, mand, Commisure, vermillion border, labial mucosa; R or L BUCCAL MUCOSA: parotid papilla, mucobuccal fold; near tooth # GINGIVA: free, attached; near tooth # TONGUE: anterior 1/3, middle 1/3, posterior 1/3; dorsal, ventral, right lateral, left lateral FLOOR OF MOUTH: lingual frenum, sublingual folds, sublingual caruncle; near tooth # PALATE: hard, soft, midline, incisive papilla; R or L OROPHARYNX: pillars, midline, uvula Border (may not be necessary when documenting elevated lesions) WELL-DEMARCATED (regular shape): easy to see where lesion begins and ends POORLY-DEMARCATED irregular shape:: difficult to see where lesion begins and ends Color change/Configuration COLOR: red, white, red and white, blue, yellow, brown, black LESION PATTERN: single lesion or multiple lesions (discrete, grouped, confluent, linear) Diameter/Dimension IF OBLONG OR IRREGULAR SHAPE: length and width IF CIRCULAR OR ROUND SHAPE: diameter (measurement of a line running from one side of a circle through the center to the other side) Type Non palpable Flat Lesions Macule: flat discolored spot, < 1 cm Patch: flat discolored spot, > 1 cm Palpable Elevated Solid Masses Papule: solid raised lesion, < 1 cm diameter Plaque: superficial raised lesion, > 1 cm diameter Nodule: marble-like lesion >1 cm diameter Wheal: localized area of skin edema Fluid-Filled Lesions Vesicle: small blister with clear fluid, < 1 cm diameter Bulla: larger blister with fluid, > 1 cm diameter Pustule: small raised pus filled lesion Loss of Skin or Mucosal Surface Ulcer: craterlike lesion with loss of top layer of skin/mucosa Fissure: linear crack History Known or unknown: if patient is aware of lesion 1. -

Ta2, Part Iii
TERMINOLOGIA ANATOMICA Second Edition (2.06) International Anatomical Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TA2, PART III Contents: Systemata visceralia Visceral systems Caput V: Systema digestorium Chapter 5: Digestive system Caput VI: Systema respiratorium Chapter 6: Respiratory system Caput VII: Cavitas thoracis Chapter 7: Thoracic cavity Caput VIII: Systema urinarium Chapter 8: Urinary system Caput IX: Systemata genitalia Chapter 9: Genital systems Caput X: Cavitas abdominopelvica Chapter 10: Abdominopelvic cavity Bibliographic Reference Citation: FIPAT. Terminologia Anatomica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, 2019 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Anatomica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: SYSTEMA DIGESTORIUM Chapter 5: DIGESTIVE SYSTEM Latin term Latin synonym UK English US English English synonym Other 2772 Systemata visceralia Visceral systems Visceral systems Splanchnologia 2773 Systema digestorium Systema alimentarium Digestive system Digestive system Alimentary system Apparatus digestorius; Gastrointestinal system 2774 Stoma Ostium orale; Os Mouth Mouth 2775 Labia oris Lips Lips See Anatomia generalis (Ch. -

Oral Clinical Examination
Lips and labial mucosa External portion of the lips: the vermilion border and the skin Vermilion border : the exposed red portion of the lip, covered by mucous membrane, no mucous glands Boundary: the moist labial mucosa in the mouth and the mucocutaneous junction on the skin Skin around the mouth: Lateral labial sulcus: begins at the ala of the nose and progresses downward and outward Mesial labial sulcus: begins at the corners of the mouth(commisures) and runs parallel to the lateral labial sulcus Mental labial sulcus: runs parallel to the mucoucutaneous junction of the lower lip Philtrum: a depression that divides the upper lip into right and left halves Upper and lower labial frenum: at the midline of the upper and lower lip Fibroepithelial polyp: small tag of tissue of the upper labial frenum Buccal mucosa Lining of the cheek Parotid papilla: near the second maxillary molar tooth on the buccal mucosa (opening of the stensen’ duct) Linea alba: hyperkeratotic line corresponding to the line of occlusion of the teeth Caliculus angularis: a small palpable nodule at the anterior termination of the linea alba Pterygomandibular raphe: a fold of tissue at the posterior boundary of the buccal mucosa Buccal frenum: attaches the buccal mucosa to both the maxilla and mandible at approximately the level of the premolar teeth Fordyce‘s granules: clusters of small, yellow nodules of ectopic sebaceous glands Leukoedema: wrinkled, whitish, opalescent appearance Mucogingival junction: junction of the attached gingiva and labial and buccal mucosa Hard -

Equine Digestive Head Neck 1.Pdf
10/12/2016 Learning Objectives for My Lectures Recognize the importance of the head. List the functions of the digestive system. Correlate the anatomy with the clinical study. EQUINE UPPER Understand the parts and boundaries of oral cavity and its DIGESTIVE SYSTEM anatomical features. List and give description to the salivary glands. Dr. Fawzy Elnady Describe the anatomy of the tongue. Prof. of Anatomy and Embryology Cairo University Describe the anatomy of the pharynx. 10516 Introduction Key terms Why the head is important? Herbivores What are the functions? Carnivores Prehension Omnivores Mastication Vegetarian Chemical digestion Vegan Absorption Elimination of wastes Key terms Key terms Digestive or gastrointestinal Lingual/glossal = tongue Stomatitis mouth tube/tract (GIT) Gingiva = gum (mucosa = gastroenteric over the jaws, it is less Gingivitis gingiva sensible, no glands) Alimentary canal = gut Entery ---- intestine Glossitis tongue Oris ---- oral ---- mouth Peristalsis Labial --- lip Cheilitis lips Buccal --- cheek Pharyngitis pharynx Dento = donto ----- teeth Esophagus esophagitis 1 10/12/2016 Boundaries of the maxillary sinus: Approach to RMS Approach to CMS Maxillary Sinus Width of mandible and Oral mucosa maxilla 1st line of defense Smooth, shiny, pink . Maxilla is wider than mandible . Outside of upper cheek teeth and inside of Stratified squamous epithelium lower teeth ecome sharp 2 10/12/2016 Capillary refill time (CRT) Oral cavity Boundaries Rostrally --- lips Laterally --- cheeks Dorsally --- Hard palate Ventrally --- tongue and mucous membrane Caudally --- isthmus faucium DOG Isthmus faucium Divisions of the oral cavity The oral cavity communicates with the oro-pharynx Oral cavity through the isthmus faucium (aditus pharyngis) It is bounded by soft palate --- dorsally Oral cavity Oral vestibule root of tongue --- ventrally proper palato-glossal fold --- laterally Labial v. -
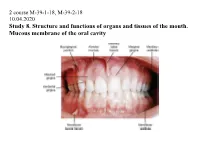
Study 8. Structure and Functions of Organs and Tissues of the Mouth
2 course М-39-1-18, М-39-2-18 10.04.2020 Study 8. Structure and functions of organs and tissues of the mouth. Mucous membrane of the oral cavity Oral cavity Oral cavity consists of two parts: anterior – vestibule, posterior – oral cavity proper, including tongue, teeth, their supporting tissues (alveolar bone, periodontal ligaments), salivary glands and tonsils. Lips Red border of the lips is a transition zone (line of Klain). Cheeks Mucous membrane of the cheeks is mobile. Gums Gingiva consists of three areas: the marginal gingival, alveolar gingiva, gingival papillae. Hard palate The mucosa of the hard palate in the region of palatal suture and close to the alveolar bone has no submucosa. Near the central incisors there is incisive papilla. Soft palate The mucous membrane of the soft palate is characterized by the presence of a significant amount of elastic fibers on the border of the lamina propria of the mucosa and submucosa. Tongue Tongue is a muscular organ of the mouth. Salivary glands There are major and minor salivary glands. Minor salivary glands are located in the submucosal layer of the oral cavity. Parotid glands are the largest pair of glands. Excretory duct a valve that regulates the release of the secret. Parotid glands produces serous secretion. Its amount depends on the organism condition, sight and smell of food. Cells of the parotid gland take part in removing toxins and remedies from the organism. Parotid glands are endocrine glands, as their secret parotin includes in mineral and protein metabolism. Sensitive, sympathetic and parasympathetic nerves takes part in the innervations of the parotid salivary glands. -

Anatomic Landmarks © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT for SALE OR DISTRIBUTION NOT for SALE OR DISTRIBUTION
© Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION SECTION 1 © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION Anatomic Landmarks © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION Objectives: © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC • Recognize, define,NOT and describe FOR SALE the soft OR tissue DISTRIBUTION structures and landmarks of the anteriorNOT and FOR posterior SALE oral OR DISTRIBUTION cavity. • Recognize, define, and describe the soft tissue structures and landmarks of the floor of the mouth, tongue, and palate. • Recognize,© Jones define, & Bartlett and describe Learning, the soft LLC tissue structures and landmarks© Jones of the & periodontium. Bartlett Learning, LLC • Recognize,NOT FOR define, SALE and OR describe DISTRIBUTION the bony structures and landmarksNOT of the FOR maxilla SALE and mandible OR DISTRIBUTION and adjacent regions. • Recognize, define, and describe common variants of normal. • In the clinical setting, identify intraoral soft tissue structures and anatomic landmarks in a patient’s mouth. © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION © Jones & Bartlett Learning, LLC © Jones & Bartlett Learning, LLC NOT FOR SALE OR DISTRIBUTION NOT FOR SALE OR DISTRIBUTION 1 © Jones & Bartlett Learning LLC, an Ascend Learning Company. -

Oral Cavity, Tongue, Salivary Glands, Teeth
ORAL CAVITY, TONGUE, SALIVARY GLANDS, TEETH Andrea Heinzlmann Veterinary University Department of Anatomy and Histology 18th MARCH 2019 FUNCTION OF THE DIGESTIVE SYSTEM 1. prehension of food 2. mastication 3. digestion 4. absorption 5. initial storage of the nutreints 6. expulsion of the unabsorbed portion of the food https://hu.pinterest.com/pin/253609022739030729/ STRUCTURES OF THE DIGESTIVE SYSTEM 1. MOUTH 2. PHARYNX 3. ALIMENTARY CANAL 4. ACCESSORY GLANDS https://equinenutritionnerd.com/2014/06/29/the-equine-digestive-system/ https://veteriankey.com/digestive-system/ https://slideplayer.com/slide/10444416/ STRUCTURES OF THE DIGESTIVE SYSTEM ALIMENTARY CANAL: • muscular tube • begins with the esophagus • ends at the anus https://www.horsehageforage.co.uk/WP/?page_id=149 RUMINANT https://slideplayer.com/slide/4157123/ DOG https://veteriankey.com/digestive-system/ http://davidmarlin.co.uk/portfolio/2313/ STRUCTURES OF THE DIGESTIVE SYSTEM ACCESSORY GLANDS: • salivary glands located on the head • liver • pancreas https://veteriankey.com/digestive-system/ http://bvetmed1.blogspot.com/201 3/02/oral-cavity-lecture-131.html https://veteriankey.com/digestive-system/ https://hu.pinterest.com/pin/294704369347319951/ CONSECUTIVE SEGMENTS OF THE DIGESTIVE SYSTEM 1. MOUTH 2. PHARYNX 3. ESOPHAGUS 4. STOMACH 5. SMALL INTESTINE 6. LARGE INTESTINE 7. ANAL CANAL https://veteriankey.com/digestive-system/ ORAL CAVITY • extends from the lips to the entrance into the pharynx STRUCTURES OF THE ORAL CAVITY: 1. tongue 2. teeth 3. salivary glands ORAL CAVITY