Evaluation of a Novel Classification of Heat-Related Illnesses
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Teikyo Heisei University in June 2006 and Has Served 2
HP http://www.thu.ac.jp/ Tel 03-5843-3200 0120-918-392 School Philosophy We aim to give our students a broad range of knowledge and abilities applicable in specialized fields based on a foundation of practical learning. In this way, we nurture creative individuals with a powerful love for humanity. President This is where I want to learn. Fundamental Principles Hiroko Okinaga 冲永 寛子 1. Nurture a love for humanity through a well-balanced education in liberal arts, social science and natural science. Cultivate an ability to listen to Hiroko Okinaga graduated from the Department of Medicine in the Faculty of Medicine at the others, and cultivate in students a strong character capable of correctly University of Tokyo. She earned her doctorate applying specialized knowledge and abilities with the aim of improving in medicine and is a practicing physician. After working in the Division of Nephrology and A Comprehensive the happiness and health of others. Endocrinology at the University of Tokyo Hospital, she was appointed deputy director of Teikyo Heisei University in June 2006 and has served 2. Foster independence and tenacity in students, and cultivate richly as president since August 2007. She has been creative individuals with a broad range of advanced practical knowledge awarded with the Japan Endocrine Pathology Society Prize and the Acromegaly Forum Prize. University of and interdisciplinary problem-solving abilities. 3. Conduct deep research into specialized academic fields, communicate the results of our research to the world, and utilize university staff and facilities to improve how we interact with and contribute to local Practical Learning communities and to the improvement of the human condition. -

Evaluation of Versatile English Learning System Using Webpages As Learning Materials
International Journal of Information and Education Technology, Vol. 7, No. 6, June 2017 Evaluation of Versatile English Learning System using Webpages as Learning Materials Yuki Oikawa, Kozo Mizutani, and Masayuki Arai paper reports on the results of an evaluation of our system. Abstract—In Japan, there is a strong demand for English language instruction not only from students, but also from working adults. However, the nation has few systems that have II. SYSTEM OUTLINE functions for improving English language skills (listening, speaking, reading, and writing) that are both inexpensive and Fig. 1 describes how to execute our system. First, users simple to operate. In an effort to help resolve this problem, we access a webpage of their choice, and then they click the developed a versatile English learning system that uses “English Learning” button. This allows them to obtain the webpages as learning materials. The system has the following learning materials shown in the right side of the figure. characteristics: it creates Japanese versions of webpages Fig. 2(a)–2(c) show the three panels of the client view of translated from English, it can determine a user’s English skill level, it is capable of speaking and listening interactions, it does our system. Fig. 2(a) and 2(b) show an example of an English not require a subscription fee, and it is easy to operate. This language webpage selected by a user and the same webpage paper reports on the results of an evaluation of our system. translated into Japanese, respectively. Users can select unlearned or previously learned words, as shown in Fig. -

FAQ Regarding UNHCR-Refugee Higher Education Programme (RHEP) (For Candidates with Sufficient Language Skills for Pursing a Degree in English)
2022 admission (2021 selection) version FAQ regarding UNHCR-Refugee Higher Education Programme (RHEP) (For candidates with sufficient language skills for pursing a degree in English) Refugees have high potential to grow as competent personnel for the hosting community, and education is essential in preparing young refugees to rebuild their lives and to enable them to contribute their skills and knowledge to their new environment. The UNHCR Refugee Higher Education Programme (RHEP) purports to provide the basis of self-reliance for those who reside in Japan and are unable to enjoy sufficient rights and benefits because of their backgrounds as refugees and language barriers. Here are some frequently asked questions that may provide more information relevant to you, as a refugee, or your institution, if your university is interested in participating in the Programme: Q1. What is the Refugee Higher Education Programme? The UNHCR-Refugee Higher Education Programme (RHEP) is implemented by UNHCR and Japan for UNHCR in partnership with twelve universities in Japan, to grant scholarships to those who are protected as refugees in Japan, to receive a higher education offered by the partner universities. From academic year 2019, Waseda University started offering a graduate degree education at master or doctor’s degree course, and from the 2022 academic year (admission in April 2022), Soka University, Meiji University, and Teikyo University will also start accepting applications for their master's programmes. The scholarship scheme for the graduate degree programme is slightly different from that for the undergraduate course. Currently, many refugees in Japan have no option but to forgo the idea of pursuing higher education, primarily for socio- economic reasons. -

Selected Papers No.26" Contains English-Language Versions of Papers from the Japanese News- Letter Edition, Published from No.471 (2020.3.20) to No.490 (2021.1.5)
Selected Papers N o . 26 June 2021 P resident's Message As mankind moves through the 21st century, integrated policies of ocean governance are increasingly necessary for the sustainable development and use of our oceans and their resources and for the protection of the marine environment. Towards this end, Ocean Policy Research Institute (OPRI) of the Sasakawa Peace Foundation orients its research on ocean issues in line with the mission statement "Liv- ing in Harmony with the Oceans." OPRI aims to conduct cross-sectoral research in ocean related issues in order to initi- ate debate on marine topics and to formulate both domestic and international policy proposals. We publish a Japanese-language newsletter titled the "Ocean Newsletter" (previously known as "Ship & Ocean Newsletter") twice a month. "Ocean Newsletter Selected Papers No.26" contains English-language versions of papers from the Japanese News- letter edition, published from No.471 (2020.3.20) to No.490 (2021.1.5). The Ocean Newsletter seeks to provide people of diverse viewpoints and backgrounds with a forum for discussion and to contribute to the formulation of maritime policies condu- cive to coexistence between mankind and the ocean. Our Institute believes that the Newsletter can expand effective communication on these issues by introducing timely research abroad to an informed readership. It also welcomes responses from readers, some of which appear in the Newsletter. It is our sincere hope that these Selected Papers will provide useful insights on policy debate in Japan -

International Perspectives in Geography
International Perspectives in Geography AJG Library Volume 16 Editor-in-Chief Yuji Murayama, The University of Tsukuba, Tsukuba, Japan Series Editors Yoshio Arai, Teikyo University, Utsunomiya, Japan Hitoshi Araki, Ritsumeikan University, Kusatsu, Japan Shigeko Haruyama, Mie University, Tsu, Japan Yukio Himiyama, Hokkaido University of Education, Sapporo, Japan Mizuki Kawabata, Keio University, Tokyo, Japan Taisaku Komeie, Kyoto University, Kyoto, Japan Jun Matsumoto, Tokyo Metropolitan University, Tokyo, Japan Takashi Oguchi, The University of Tokyo, Kashiwa, Japan Toshihiko Sugai, The University of Tokyo, Kashiwa, Japan Atsushi Suzuki, Rissho University, Kumagaya, Japan Teiji Watanabe, Hokkaido University, Sapporo, Japan Noritaka Yagasaki, Nihon University, Tokyo, Japan Satoshi Yokoyama, Nagoya University, Nagoya, Japan Aim and Scope The AJG Library is published by Springer under the auspices of the Association of Japanese Geographers. This is a scholarly series of international standing. Given the multidisciplinary nature of geography, the objective of the series is to provide an invaluable source of information not only for geographers, but also for students, researchers, teachers, administrators, and professionals outside the discipline. Strong emphasis is placed on the theoretical and empirical understanding of the changing relationships between nature and human activities. The overall aim of the series is to provide readers throughout the world with stimulating and up-to-date scientific outcomes mainly by Japanese and other Asian geographers. Thus, an “Asian” flavor different from the Western way of thinking may be reflected in this series. The AJG Library will be available both in print and online via SpringerLink. About the AJG The Association of Japanese Geographers (AJG), founded in 1925, is one of the largest and leading organizations on geographical research in Asia and the Pacific Rim today, with around 3000 members. -

The Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension
Hypertension Research (2014) 37, 254–255 & 2014 The Japanese Society of Hypertension All rights reserved 0916-9636/14 www.nature.com/hr The Japanese Society of Hypertension Committee for Guidelines for the Management of Hypertension CHAIRPERSON Kazuaki SHIMAMOTO (Sapporo Medical University) WRITING COMMITTEE Katsuyuki ANDO (University of Tokyo) Ikuo SAITO (Keio University) Toshihiko ISHIMITSU (Dokkyo Medical University) Shigeyuki SAITOH (Sapporo Medical University) Sadayoshi ITO (Tohoku University) Kazuyuki SHIMADA (Jichi Medical University) Masaaki ITO (Mie University) Kazuaki SHIMAMOTO (Sapporo Medical University) Hiroshi ITOH (Keio University) Tatsuo SHIMOSAWA (University of Tokyo) Yutaka IMAI (Tohoku University) Hiromichi SUZUKI (Saitama Medical University) Tsutomu IMAIZUMI (Kurume University) Norio TANAHASHI (Saitama Medical University) Hiroshi IWAO (Osaka City University) Kouichi TAMURA (Yokohama City University) Shinichiro UEDA (University of the Ryukyus) Takuya TSUCHIHASHI (Steel Memorial Yahata Hospital) Makoto UCHIYAMA (Uonuma Kikan Hospital) Mitsuhide NARUSE (NHO Kyoto Medical Center) Satoshi UMEMURA (Yokohama City University) Koichi NODE (Saga University) Yusuke OHYA (University of the Ryukyus) Jitsuo HIGAKI (Ehime University) Katsuhiko KOHARA (Ehime University) Naoyuki HASEBE (Asahikawa Medical College) Hisashi KAI (Kurume University) Toshiro FUJITA (University of Tokyo) Naoki KASHIHARA (Kawasaki Medical School) Masatsugu HORIUCHI (Ehime University) Kazuomi KARIO (Jichi Medical University) Hideo MATSUURA (Saiseikai Kure Hospital) -

FAQ Regarding UNHCR-Refugee Higher Education Programme (RHEP) (For Candidates with Sufficient Language Skills for Pursing a Degree in English)
2021 admission (2020 selection) version FAQ regarding UNHCR-Refugee Higher Education Programme (RHEP) (For candidates with sufficient language skills for pursing a degree in English) Refugees have high potential to grow as competent personnel for the hosting community, and education is essential in preparing young refugees to rebuild their lives and to enable them to contribute their skills and knowledge to their new environment. The UNHCR Refugee Higher Education Programme (RHEP) purports to provide the basis of self-reliance for those who reside in Japan and are unable to enjoy sufficient rights and benefits because of their backgrounds as refugees and language barriers. Here are some frequently asked questions that may provide more information relevant to you, as a refugee, or your institution, if your university is interested in participating in the Programme: Q1. What is the Refugee Higher Education Programme? The UNHCR-Refugee Higher Education Programme (RHEP) is implemented by UNHCR and Japan for UNHCR in partnership with eleven universities in Japan, to grant scholarships to those who are protected as refugees in Japan, to receive a 4 year undergraduate education offered by the partner universities. From academic year 2019, Waseda University started offering a graduate degree education at master or doctor’s degree course. The scholarship scheme for the graduate degree programme is slightly different from that for the undergraduate course. Currently, many refugees in Japan have no option but to forgo the idea of pursuing higher education, primarily for socio-economic reasons. Accordingly, the employment opportunities for those refugees are severely limited compared to others who have completed some form of higher education. -

The Editor-Inchief, Together with All the Members of the Editorial Staff
97 Acknowledgments The Editor-inChief, together with all the members of the editorial staff of the Acta Paediatrica Japonica, wishes to extend the most cordial thanks to the reviewers who have contributed their time and efforts in reviewing the manuscripts submitted and improving the quality of this journal. The reviewers for the year 1987 were as follows: AKABANE, Taro IWATA, Tsutomu Shinshu University School of Medicine Faculty of Medicine, University of Tokyo ANDO, Masahiko KAJII, Tadashi Tokyo Women’s Medical College Yamaguchi University School of Medicine ARISAKA, Osamu KATO, Kiyohiko Juntendo University School of Medicine Yamanashi Medical College ASAI, Toshio KIDA, Mitsushiro Kanazawa Medical University Teikyo University School of Medicine BABA, Kunizo KITAGAWA, Teruo Kobe City General Hospital Nihon University School of Medicine CHIBA, Shunzo KOBAYASHI, Tatsuharu Sapporo Medical College Kansai Medical University EGI, Shinzo KOIKE, Michio Faculty of Medicine, University of Tokyo Wakayama Medical College FUKUI, Hiromu KOMIYA, Kazuhiko Nara Medical University Tokyo Metropolitan Neurological Hospital FUKWAMA, Yukio KONNO, Tasuke Tokyo Women’s Medical College Tohoku University School of Medicine HARADA, Kensuke KUROKI, Yoshikazu Nihon University School of Medicine Kanagawa Children’s Medical Center HASHIMOTO, Takeo KUSAKAWA, Sanji St. Maria Hospital Tokyo Women’s Medical College HAYASHI, Sadao MAEDA, Kaiuichi Kurume University School of Medicine Saitama Medical School HAYASHI, Tadashi MATSUO, Nobutake Yamagata University School of -

Teikyo University Learn “One’S Way” to Approach Endeavors by Thinking for Yourself, and Soar Into the Skies
http://www.teikyo-u.ac.jp/ UNIVERSITY GLOBAL GUIDE BOOK [ ENGLISH ] 2019.10 Number of THE World University 10 Faculties, international students Rankings 2019 among private 32 Departments, universities Approx.1,100 No. in Japan School Philosophy Educational Philosophy Educational Guidelines 1 (2019 academic year) 1 Junior College One’s way Practical learning Through applied programs we aim to that helps students master logical thinking develop skilled human resources who: “One’s way” refers to a life philosophy skills through real-world experience. whereby one nds their purpose or - Recognize that achievement comes interests and learns the knowledge and from eort skills to maximize their own unique International perspectives - Have open minds and extensive individuality to their advantage. One that help students learn how to understand Number of students countries Number of graduates knowledge assumes full responsibility for the and experience other cultures. 27 consequences of their actions. We oer - Think from an international perspective our support to encourage students to - Have creativity and good character learn to live their lives “their way.” Open mindedness overseas partner that helps students learn a balanced Approx. 24,000 schools and Approx.160,000 mix of knowledge and skills that hospitals are necessary for their future. (2019 academic year) 82 (2018 academic year) Table of Contents 02 President’s Message 04 About the Campus 06 Faculties and Departments 16 Introduction to Facilities 17 Global Network 18 Life on Hachioji Campus 24 Life on Utsunomiya Campus 28 Job-search Support 29 Guide to Applications and Scholarship Systems President’s Message History of Teikyo University Learn “One’s way” to approach endeavors by thinking for yourself, and soar into the skies. -

Medical Physics Education Program in Japan
Contents Education Courses in Medical Physics 1 Master’s Programs in Medical Physics 1 Doctoral Programs in Medical Physics 6 Residency Programs in Medical Physics 10 Education Courses in Medical Physics Education Courses in Medical Physics Master’s Programs in Medical Physics Institute JBMP Accreditation Gunma University accredited Hiroshima University accredited Hokkaido University accredited Ibaraki Prefectural University of Health Sciences accredited International University of Heath and Welfare accredited Juntendo University Kitasato University accredited Kobe University accredited Komazawa University accredited Kyoto University accredited Kyushu University accredited Niigata University accredited Osaka University accredited Rikkyo University Teikyo University accredited Tohoku University accredited Tokai University accredited Tokushima University Tokyo Metropolitan University accredited University of Tsukuba accredited • Gunma University, Medical Physics and Biology for Heavy Ion Therapy • URL: http://www.med.gunma-u.ac.jp/en/ • Contact Person: Masami Torikoshi, Ph.D (email: torikosi(AT)gunma-u.ac.jp) • Program: Medical Physics and Biology for Heavy Ion Therapy: Master’s Degree Program in Medicine • Director: Noriyuki Koibuchi, M.D., Ph.D • Address: 3-39-22 Showa-machi, Maebashi, Gunma, 371-8511 • Telphone: +81-27-220-7111 • Fax: +81-27-220-8379 1 Education Courses in Medical Physics • Hiroshima University, Medical Physics Course • URL: https://www.hiroshima-u.ac.jp/en/bhs • Contact Person: Akito Saito, PhD (email: akito(AT)hiroshima-u.ac.jp) -

1. Japanese National, Public Or Private Universities
1. Japanese National, Public or Private Universities National Universities Hokkaido University Hokkaido University of Education Muroran Institute of Technology Otaru University of Commerce Obihiro University of Agriculture and Veterinary Medicine Kitami Institute of Technology Hirosaki University Iwate University Tohoku University Miyagi University of Education Akita University Yamagata University Fukushima University Ibaraki University Utsunomiya University Gunma University Saitama University Chiba University The University of Tokyo Tokyo Medical and Dental University Tokyo University of Foreign Studies Tokyo Geijutsu Daigaku (Tokyo University of the Arts) Tokyo Institute of Technology Tokyo University of Marine Science and Technology Ochanomizu University Tokyo Gakugei University Tokyo University of Agriculture and Technology The University of Electro-Communications Hitotsubashi University Yokohama National University Niigata University University of Toyama Kanazawa University University of Fukui University of Yamanashi Shinshu University Gifu University Shizuoka University Nagoya University Nagoya Institute of Technology Aichi University of Education Mie University Shiga University Kyoto University Kyoto University of Education Kyoto Institute of Technology Osaka University Osaka Kyoiku University Kobe University Nara University of Education Nara Women's University Wakayama University Tottori University Shimane University Okayama University Hiroshima University Yamaguchi University The University of Tokushima Kagawa University Ehime -
Oberlin University
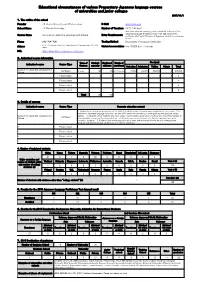
Educational circumstances of various Preparatory Japanese language courses of universities and junior colleges 2017/11/1 1.The outline of the school Founder J.F.Oberlin University and affiliated school E-Mail [email protected] School Name J.F.Oberlin University Number of Teachers 24 (2; Full-time) must have attained a passing grade on level N5 or higher of the Japanese Language Proficiency Test or be able to provide a Course Name Institute for Japanese Langauge and Culture Entry Requirements certificate of at least 150 hours of Japanese study from a language school Phone 042-704-7041 Testing Method Documents, if necessary interview 4-16-1 Fuchinobe, Chuou-ku, Sagamihara-shi, Kanagawa-ken 252-0206 Student Accommodations Adress Japan Yes, 55,000 yen / 1 month URL http://www.obirin.ac.jp/japanese_extension/ 2.Authorised course information Term of Student Registerd Month of Fee (yen) Authorized course Course Type Courses capacity students enrollment Selection Admission Tuition Others Total Institute for Japanese Langauge and Combined 1 year 120 129 April, September 15,000 100,000 500,000 0 615,000 Culture Please select 0 0 0 0 0 0 0 Please select 0 Please select 0 Please select 0 Total 120 129 3.Details of courses Authorized course Course Type Concrete education content 1. Applicants are accepted irrespective of the field of study they wish to pursue upon completion of our course. 2. In addition to Japanese language instruction, we also offer extensive counseling on undergraduate and graduate school Institute for Japanese Langauge and options. 3. Students of our institute who meet certain requirements can enroll for credit (and be issued transcripts) in Combined Culture undergraduate courses at the university level.