The Minutes That Matter Most Tulane Advances the Science & Treatment of Strokes
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Hank-Aaron.Pdf
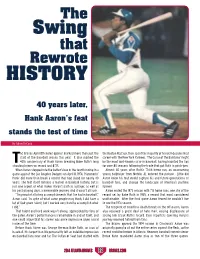
The Swing that Rewrote HISTORY 40 years later, Hank Aaron’s feat stands the test of time By Adam DeCock he Braves April 8th home opener marked more than just the the Boston Red Sox, then spent the majority of his well-documented start of the baseball season this year. It also marked the career with the New York Yankees. ‘The Curse of the Bambino’ might 40th anniversary of Hank Aaron breaking Babe Ruth’s long be the most well-known curse in baseball, having haunted the Sox standing home run record and #715. for over 80 seasons following the trade that put Ruth in pinstripes. When Aaron stepped into the batter’s box in the fourth inning in a Almost 40 years after Ruth’s 714th home run, an unassuming game against the Los Angeles Dodgers on April 8, 1974, ‘Hammerin’ young ballplayer from Mobile, AL entered the picture. Little did Hank’ did more than break a record that had stood for nearly 40 Aaron know his feat would capture his and future generations of years. The feat itself remains a marvel in baseball history, but is baseball fans, and change the landscape of America’s pastime just one aspect of what makes Aaron’s path as a player, as well as forever. his post-playing days, a memorable journey. And it wasn’t all luck. Aaron ended the 1973 season with 713 home runs, one shy of the “I’m proud of all of my accomplishments that I’ve had in baseball,” record set by Babe Ruth in 1935, a record that most considered Aaron said. -

Conversations at Home with Georgia Duker and James Johnston Are Likely to Turn to the Subject of How to Capture Someone's Imag
2088txt_22to40c5 7/16/01 2:22 PM Page 28 Conversations at home with Georgia Duker and James Johnston are likely to turn to the subject of how to capture someone’s imagination. Each professor has been honored with teaching award after teaching award. (Shown here with protégés Christina, 13, Alex, 16, and Nishi, 7- year-old tabby.) 28 PITTMED 2088txt_22to40c5 7/16/01 2:22 PM Page 29 FEATURE JUST A COUPLE OF GREAT TEACHERS BY DOTTIE HORN NO LARGER THAN LIFE he resident was in a hurry when he wrote the prescription. Without thinking, he checked “refills” on the order. Two months later, his patient came back. She had problems with bone marrow suppression. Once the resident looked at the prescription he had Twritten, he knew the cause of her problem. He said to her, I messed up. You should have only had this for two weeks. You had it for eight weeks. This was the wrong thing for you to have had for that long. The patient looked at him. I know you’ll do your best to make it better, she said. It is a story James Johnston, professor of medicine at the University of Pittsburgh School of Medicine and winner of the 2000 Chancellor’s Distinguished Teaching Award, shares with his students. It is the story of a mistake he made while treating a patient when he was a newly minted MD. “The students get the idea that a role model never has made any mistakes or that it’s never, ever talked about,” he says. -

2020-21 Season Brochure
2020 SEA- This year. This season. This orchestra. This music director. Our This performance. This artist. World This moment. This breath. This breath. 2021 SON This breath. Don’t blink. ThePhiladelphiaOrchestra MUSIC DIRECTOR YANNICK NÉZET-SÉGUIN our world Ours is a world divided. And yet, night after night, live music brings audiences together, gifting them with a shared experience. This season, Music Director Yannick Nézet-Séguin and The Philadelphia Orchestra invite you to experience the transformative power of fellowship through a bold exploration of sound. 2 2020–21 Season 3 “For me, music is more than an art form. It’s an artistic force connecting us to each other and to the world around us. I love that our concerts create a space for people to gather as a community—to explore and experience an incredible spectrum of music. Sometimes, we spend an evening in the concert hall together, and it’s simply some hours of joy and beauty. Other times there may be an additional purpose, music in dialogue with an issue or an idea, maybe historic or current, or even a thought that is still not fully formed in our minds and hearts. What’s wonderful is that music gives voice to ideas and feelings that words alone do not; it touches all aspects of our being. Music inspires us to reflect deeply, and music brings us great joy, and so much more. In the end, music connects us more deeply to Our World NOW.” —Yannick Nézet-Séguin 4 2020–21 Season 5 philorch.org / 215.893.1955 6A Thursday Yannick Leads Return to Brahms and Ravel Favorites the Academy Garrick Ohlsson Thursday, October 1 / 7:30 PM Thursday, January 21 / 7:30 PM Thursday, March 25 / 7:30 PM Academy of Music, Philadelphia Yannick Nézet-Séguin Conductor Michael Tilson Thomas Conductor Lisa Batiashvili Violin Yannick Nézet-Séguin Conductor Garrick Ohlsson Piano Hai-Ye Ni Cello Westminster Symphonic Choir Ravel Le Tombeau de Couperin Joe Miller Director Szymanowski Violin Concerto No. -
![T-Wave [Yearbook] 1984](https://docslib.b-cdn.net/cover/6579/t-wave-yearbook-1984-316579.webp)
T-Wave [Yearbook] 1984
i1 > I'cJSS V , /. \^ \ s /. x > rjjiwgwyr/J^' < :y li TULANE MEDICAL SCHOOL 1984 ®ulattp ImitptBttg C » "W Wtt f*^ I*? , Digitized by the Internet Archive in 2010 with funding from Lyrasis IVIembers and Sloan Foundation http://www.archive.org/details/twaveyearbook1984edit T-WAVE 1984 TULANE UNIVERSITY SCHOOL OF MEDICINE NEW ORLEANS, LOUISIANA VOLUME 3 YEARBOOK STAFF Donna Chester Editor in Chief Personal Album Childhood Photos Donna Park History of Tulane Senior photos Mickey Puente History of Tulane Bill Shoies The Way It Was George Luck The Way It Was Manny Ramos Admissions Faculty Sam Young PHOTOGRAPHY Senior photos Annelle Ahmed Senior photos Jim Dorcbak larcus Penn Ben Mills Senior Photos Liz Mannino Betty Mortenson Catbv Chicola Assisted all sections Bill Shoies Donna Chester Dave Treen SPECIAL THANKS To Bill Hopkins ofJosten s Publishing Co. for his expertise To Mike Puyau and Colleen Storrs for helping us get and patient counsel. organized when we didn't know which direction we To our generous sponsors and to the parents, companies and were heading. organizations who advertised in this publication. To Cindy for helping us obtain information and historic To Victoria Burten for spending long hours helping us type photos for the History of Tulane Section. the copy for this book. To Parents who contributed pictures for the Childhood Photo section. ^"' 4^4- ¥:^ [If tv^ University Of Louisiana, Medical And Law Departments Tulane University School Of Medicine 1984 THE HISTORY OF TULANE MEDICAL SCHOOL Tulane Medical School had its auspicious beginning as the Medical College of Louisiana in September 1834. Three brash young medical men. -

Brunch/Lunch
315 N. LASALLE STREET × CHICAGO, IL × 312 527 1417 • RIVERROASTCHICAGO.COM SITUATED IN THE HEART OF THE CITY, WITH STRIKING VIEWS OF THE CHICAGO RIVER AND CITY SKYLINE River Roast Private Events offers an Experienced event planning and CONTACT OUR EVENT SALES TEAM impressive setting for your next party service teams aim to accommodate and 312 527 1417 or or meeting. Helmed by Executive Chef anticipate your needs for a flawless event. [email protected] Cedric Harden, River Roast is a lively social Whether you’re planning a grand gala for riverroastchicago.com house and gathering place. 300 people or an exclusive affair for eight, 315 N. LaSalle Street | Chicago, IL the delectable customized menus and exceptional views will impress. Event Spaces • With 6 event spaces to choose from – each featuring sophisticated decor that pays tribute to the historical landmark building the restaurant is housed in – the options for corporate and social events are endless. Event Spaces SEAted Reception THE MURDOCH 280 400 THE MONARCH 160 200 MONARCH ROOM A 60 85 MONARCH ROOM B 70 90 THE REID BAR N/A 25 THE MAIN DINING ROOM 120 150 THE COMMERCE ROOM 15 N/A THE SEMI-PRIVATE ROOM 24 N/A THE VERANDA CENTER N/A 30 For larger than life events N/A 1000 THE COMPLETE PROPERTY chef CEDRIC HARDEN CHEF CEDRIC HARDEN IS THE LEADING FORCE BEHIND THE CULINARY PROGRAM AT RIVER ROAST • Growing up with the natural inclination and desire to cook for his family, Harden’s passion for food was sparked at a very early age. -

Larger Than Life: Immersion and Imagination in the Not-So-Small Worlds Sustained by Scale
318 THE VALUE OF DESIGN Larger Than Life: Immersion and Imagination in the Not-So-Small Worlds Sustained by Scale DONALD KUNZE Pennsylvania State University Despite the common use of scale models made of being in two places at once makes the LTL model at a “smaller scale” than the 1:1 of everyday life, a scale model par excellence and, because it mate- the case of the “larger-than-life” (LTL) model is rializes the essential operations of the imagination, not only signifi cant but instructive.1 Like the set a model of the imagination’s role in architecture of Alfred Hitchcock’s North by Northwest, where and other forms of art as well. Cary Grant and Eva Marie Saint are chased over the presidential faces of Mt. Rushmore, or the pen- LTL immersability can be conferred on models that etrable Statue of Liberty in the New York harbor, are not technically larger-than-life, or not even the immersability of the user of the LTL model models in the strict sense: Kurt Schwitters’ Merz- demonstrates the key quality of all scale models: bau, Jacques Tati’s set for the fi lm Playtime (1967), the ability of scale consistency to sustain the il- the National Mall in Washington, D. C., or even the lusion of the model’s imaginary world.2 The LTL “lands” created by Walt Disney to support bad faith model allows the viewer to enter, often literally, versions of the wild west, the future, or fairy tales. into the perceptual fi eld created by the model, but Whenever the viewer can fi nd a place inside the during this immersion scale difference prevents a fi eld of what can be regarded as a model, even full merger of viewer with the viewed. -
HISTORICAL FICTION Suggested Reading List
Juv Fiction CAO W Juv Paperback FORBES E HISTORICAL FICTION BRONZE AND SUNFLOWER JOHNNY TREMAIN Taken in by a poor family in a rural vil- After injuring his hand, a silversmith's ap- Suggested Reading List lage, Sunflower bonds with the family's prentice in Boston becomes a messenger *First in a Series only child, Bronze, who has not spoken for the Sons of Liberty in the days before since being traumatized by a terrible fire. the American Revolution. YA Fiction ANDERSON L Juv Fiction COATS J Juv Fiction FRANK S CHAINS* THE MANY REFLECTIONS OF ARMSTRONG & CHARLIE After being sold to a cruel couple in New MISS JANE DEMING During the pilot year of a Los Angeles York City, a slave named Isabel spies for Jane is excited to be part of an expedi- school system integration program, two the rebels during the Revolutionary War. tion to bring orphans and Civil War wid- sixth grade boys, one black and one white, become best friends. ows to Washington Territory. Juv Paperback AVI Juv Paperback CURTIS C Juv Fiction GRATZ A CRISPIN: THE CROSS OF LEAD* BUD, NOT BUDDY REFUGEE An orphaned peasant boy in fourteenth- Bud, a motherless boy living in Michigan Josef, a Jewish boy living in 1930s Germa- century England flees his village and during the Great Depression, escapes a ny; Isabel, a Cuban girl in 1994; and meets a larger-than-life juggler who bad foster home and sets out in search of Mahmoud, a Syrian boy in 2015, embark holds a dangerous secret. the man he believes to be his father. -

Curriculum Vitae: James R. Andrews, M.D. 1
Curriculum Vitae: James R. Andrews, M.D. James R. Andrews, M.D. Curriculum Vitae EDUCATION Fellowships Knee Surgery & Athletic Injuries July 1972 - December 1972 University of De Lyon, France Service De Professor: Albert Trillat, M.D Hand Surgery & Athletic Medicine January 1972 - June 1972 University of Virginia Medical Center Sponsor: Frank C. McCue, III, M.D. Chief of Service: Warren Stamp, M.D. Residency Tulane University School of Medicine July 1, 1968-December 30, 1972 Department of Orthopedic Surgery Chief of Service: Jack Wickstrom, M.D Third Year Residency Rotation, Columbus, GA July 1970-July 1971 With: Jack C. Hughston, MD Post-Graduate Tulane Basic Science Course Jan. 1970 - June 1970 Internship USPHS Hospital July 1967-June 1968 San Francisco, CA Mixed Medicine Medical School Louisiana State University School of Medicine 1963-1967 New Orleans, Louisiana Externship University of Washington Summer 1964 Three Months – Orthopaedics and Physical Medicine Louisiana State University 1960-1963 Baton Rouge, Louisiana Bachelor of Science Degree Homer School System ( Grades: 1-12) 1948-1960 Homer, Louisiana 1 Curriculum Vitae: James R. Andrews, M.D. PRIVATE PRACTICE The Andrews Institute Part-time: May 2005 – April 2011 Gulf Breeze, FL Full-time: April 2011 – Present Andrews Sports Medicine & Orthopaedic Center November 2007 – April 2011 Birmingham, AL Alabama Sports Medicine & Orthopaedic Center October 1986 – November 2007 Birmingham, AL (name changed) Hughston Orthopaedic Clinic January 1973-October 1986 Columbus, GA RESEARCH AND EDUCATIONAL ACTIVITIES Medical Director of the Andrews Institute May 2005-Present President & Chairman of the Board: Andrews Research & Education May 2005 – Present Foundation (formally Andrews Research & Education Institute) Chairman of the Board & Medical Director: American Sports Medicine October 1986 - Present Institute (ASMI) AREAS OF SPECIAL INTEREST & CONCERN: 1. -

BULLETIN Volume 99, Number 7 • July 1, 2012 Our Hollywood History
WILSHIRE BOULEVARD TEMPLE BULLETIN Volume 99, Number 7 • July 1, 2012 Our Hollywood History hey called him “Rabbi to the Stars.” During his 69 years Thalberg’s spirit lives on among the scaffolds and platforms Tas senior rabbi at Wilshire Boulevard Temple, Rabbi rising up to the ceiling of the dome where today restoration Edgar F. Magnin cultivated close, personal relationships with work on its coffered plaster, the Sh’ma and oculus are at full legendary entertainment industry executives and celebrities. speed. Once crumbling to the floor, plaster is being repaired He presided over the life-cycle events of larger than life movie or replaced, the gold trim regilded and the center repainted to moguls Louis B. Mayer, the Warner brothers and appear as it was in 1929, in its original, dazzling glory. Irving Thalberg, among many others. These show business Rabbi Magnin died in 1984 at the age of 94. Shortly pioneers both inspired and helped build, in 1929, the historic before his death, he summed up his life: “God has been good to Temple we now call home. me. I’ve been very fortunate in the choice of my ancestors and For the third Temple of what was then Congregation the choice of my friends.” B’nai B’rith, Rabbi Magnin envisioned a main sanctuary This history has come full circle—recently illustrated in with an interior like a theater. Mayer donated the funds for an article in the Hollywood Reporter’s June 8 issue. The article, the Main Sanctuary’s east and west triple lancet art glass “Hollywood’s Hottest $150 Million Project is an 83-Year-Old windows. -

Curriculum Vitae 1 Robert A
Curriculum Vitae 1 Robert A. Gordon, M.D., F.A.A.P. ROBERT A. GORDON, MD, FAAP, FAAO Curriculum Vitae ADDRESS: Tulane University Health Sciences Department of Ophthalmology 1430 Tulane Avenue, Box SL-69 New Orleans, Louisiana 70112-2699, USA Email: [email protected] EDUCATION: Fellowship, Pediatric Ophthalmology & Strabismus, University of Indiana - 1976 Chief Resident of Ophthalmology, Tulane University - 1972-1973 Resident, Tulane University, Department of Ophthalmology - 1970-1973 Rotating Internship, Ben Taub Hospital-Baylor Affiliated, Houston, TX-1969-1970 Tulane University School of Medicine, M.D. - 1969 Tulane University, B.S. Chemistry and Mathematics- 1965 LICENSURE/CERTIFICATIONS: 1969-Present Louisiana Board of Medical Examiners 1970 National Board of Medical Examiners 1977-Present Drug Enforcement Administration Certificate of Insurance Controlled Dangerous Substance 1976 American Board of Ophthalmology (Lifetime) CURRENT POSITION: Chief, Pediatric Ophthalmology and Adult Strabismus Tulane University Health Sciences HOSPITAL APPOINTMENTS: Active, Tulane University Hospital, New Orleans, LA, since 1975 Curriculum Vitae 2 Robert A. Gordon, M.D., F.A.A.P. Active, Senior Visiting Surgeon, Medical Center of New Orleans, New Orleans, LA, since 1976 Consulting Staff, Terrebonne General Hospital, Houma, La since 2005 Consulting Staff, Lake Charles Memorial Hospital, Lake Charles, LA, since 2004 Consulting Staff, Lakeview Regional Medical Center, Covington, LA, since 2008 Consulting Staff, St. Tammany Parish Hospital, Covington, LA, since 2006 Consulting Staff, Veterans Administration Medical Center, New Orleans, LA, since 1976 Consulting Staff, Lakearea Hospital, Lake Charles, since 2004 Consulting Staff, Slidell Memorial Hospital, Slidell, LA, since 2003 Courtesy, Children’s Hospital, New Orleans, LA, since 1977 Courtesy, St. Francis Medical Center, Monroe, LA, since 1997 Courtesy, Terrebonne General Medical Center, Houma, LA, since 2007 Courtesy, West Jefferson Hospital, Marrero, LA, since 1994 Past Affiliations: Courtesy, Huey P. -

How a Gulf South Business School Became a Global Leader A
GOLDRING/WOLDENBERG NEW MASTER’S IN BUSINESS FORMER EXECUTIVE VP EXPANSION NEARS COMPLETION ANALYTICS TO LAUNCH BEGINS NEW CHAPTER t HOW A GULF SOUTH BUSINESS SCHOOL BECAME A GLOBAL LEADER A. B. FREEMAN SCHOOL OF BUSINESS TULANE UNIVERSITY SUMMER OF FREEMAN SCHOOL 2017 B. A. WAVE ‘17 HOMECOMING REUNION FAMILY WEEKEND In 2017, Freeman graduate reunions are BIGGER and BETTER THAN EVER! RECONNECT WITH YOUR CLASSMATES CATCH UP WITH THE LATEST AT FREEMAN ENJOY A FALL WEEKEND IN NEW ORLEANS Tentative Events: FRIDAY, NOVEMBER 3, 2017 • Dean’s State of the School Address • “Back to the Classroom” Faculty Lectures • Tours of the new Goldring/Woldenberg Business Complex • Graduate Reunion Welcome Party for all reunion classes • Informal Class Parties (as planned by class committees) SATURDAY, NOVEMBER 4, 2017 • Freeman Tailgate, LBC Quad • Tulane Homecoming Game, Yulman Stadium • All-Alumni After Party, Tipitina’s To see your class list, go to freemanalumni.tulane.edu/reunions Content is updated regularly. To learn more about leadership opportunities, email [email protected] CLASSES OF 1967 1972 1977 1982 1987 1992 1997 2002 2007 2012 1 Summer 2017 2017 Summer 1 . XXXIV XXXIV No . Vol t THE MAGAZINE OF THE A. B. FREEMAN SCHOOL OF BUSINESS TULANE UNIVERSITY 22 GLOBAL REACH Over the past two decades, the A. B. Freeman School of Business has emerged as one of the most international business schools in America. 2 FROM THE DEAN 3 IN THE NEWS 19 RESEARCH 32 KEEPING UP WITH YVETTE JONES 36 WITH ALUMNI Above: Tulane University’s former executive vice president is doing what she enjoys most in her latest endeavor. -

Patient Praises Cardiac Partnership
ruralroads Patient praises cardiac partnership Rural recruitment and retention Collaboration addresses children’s mental health NRHA volunteers rebuild homes SUMMER 2008 A QUARTERLY MAGAZINE VOLUME 6, NO. 2 @hp8\Zg8p^8[^lm8\Zk^8_hk8 ^o^krhg^8bg8hnk8\hffngbmr 8 Siemens broad portfolio of solutions can help you continue to deliver responsive and compassionate care. Gg^8;hffngbmr8EZgr8Dbo^l8Gg^8?hZe8Kb^f^gl8bl8]^]b\Zm^]8mh8a^eibg`8rhn8_bg]8ma^8kb`am8\hf[bgZmbhg8h_8AL8bfZ`bg`88 Zg]8eZ[8ikh]n\ml8maZm8Zk^8ngbjn^8mh8rhnk8hk`ZgbsZmbhgÁl8`hZel8=gaZg\^8jnZebmr8\Zk^8;k^Zm^8Z8_bl\Zeer8obZ[e^8_nmnk^88 Kb^f^gl8bl8ikhn]8mh8[^8ma^8_bklm8f^]b\Ze8bfZ`bg`8Zg]8AL8\hfiZgr8mh8[^8Z8FJ@98?he]8D^o^e8;hkihkZm^8HZkmg^k88 pppnlZlb^f^gl\hf¥\hffahli8¦¦¦ Answers for life. 9¦ ¦9¦9 Û88Kb^f^gl8E^]b\Ze8Khenmbhgl8MK98Ag\89ee8kb`aml8k^l^ko^] A9111_8994_v3.indd 1 6/6/08 9:17:05 AM Rural Roads is a publication of the National Rural Health Association, a not-for-profit association composed of individual and organizational members who share a common interest in rural health. Rural Roads seeks to disseminate news and information of interest to rural health ruralroads professionals to help establish a national network of rural health care advocates. For more information on joining the NRHA, go to www.RuralHealthWeb.org or call Estelle Montgomery at 816-756-3140. A QUARTERLY MAGAZINE 2008 Board of Trustees VOLUME 6, NO. 2 Officers Paul Moore, President ISSN 1550-6576 Beth Landon, President-elect Sandra Durick, Treasurer Mike French, Secretary George Miller, Past-president 4 Farming lessons still relevant Constituency Group Chairs Raymond Christensen – Clinical Services 5 Project helps farmer with Art Clawson – Community Grassroots disability Greg Dent – Community-operated Practices Marita Novicky – Diverse Underserved Populations 6 Education, advocacy and Kristin Juliar – Frontier networking H.D.