Breast Augmentation Info
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Taking Your Measurements \ I / \ I / ' ------/ / ' ,,,__
• 1mp s __ ...,... ___ _. _____ ___ ,,. -, Bulletin 498 / January 1956 / ' : TAKING YOUR MEASUREMENTS \ I / \ I / ' ------ / / ' ,,,__..... --- ------- ./ _,."' / / --- --- 1 -------------- \ \ ' A good looking dress is a well-fitted dress. Achieving a good fit depends upon three things: knowing your own figure measurements, selecting the size and type pattern which most nearly corres ponds to your measurements, and then making any necessary alterations in the pattern before cutting your dress. This leaflet tells you how to take your measurements and provides a place for you to record them. What Is A Well-fitted Dress? A dress that fits you well adapts itself to your body. Ir brings out your good points and skillfully hides your poor ones. You will know a good fit by- Direction of grain of fabric. - Crosswise yarns are parallel to the floor at the center-front and back busdine, and at the hipline, unless the dress has unusual style details. lengthwise yarns are at right angles to the floor at the center-front and back of both skirt and bodice of a dress. lengthwise yarns on the sleeve cap lie in the direction of the arm when it hangs straight at the side . This varies slightly on different figures but in general the crosswise yarns are also parallel are straight in front and back of your arm except to the floor. when special style features, such as extended shoul Direction of seam lines. - Seam lines that ders, requir.e otherwise. lie and hang straight keep your dress in proper li~e The waistline seam appears to be straight around on your figure. -

Ajsl ,QJI 8Ji)9
ajsL ,QJI 8jI)9 MINSTRY OF SOCIAL AFFAIRS L",uitom cz4 /ppaLf ('"oduaDon P'"zuocz1 Volume 2 TAILORING //, INTEGRATED SOCIAL SERVICES PROJECT aLSioJ 8jsto!*14I 3toj3JI J54o 4sjflko MINSTRY OF SOCIAL AFFAIRS cwitom c92/I/2a'LEf ?'oduation 57P/D 0 E15 ('uvzicul'um JoL CSPP nstzucto~ Volume 2 TAILORING g~jji~JI 6&= z#jJEi l tl / INTEGRATED SOCIAL SERVICES PROJECT wotsoi stoim 1oj3jw jsi.Lo 6suJf PREFACE The material which follows is .J l.a ,,h &*.aJIL& . part of a five volume series assem bled by the faculty and students of . 3aJ e~- t.l. -, r'- ,tY.. the University of North Carolina at L_:J q L--, X4 0-j VO Greensboro, Department of Clothing and Textiles, CAPP Summer Program. The CAPP, Custom Appar,1 Production LFJI L,4.," ,'"i u .U. J l Process, Program was initiated in Egypt as a part of the Integrated Social Services Project, Dr. Salah L-,S l k e. L C-j,,. El Din El Hommossani, Project Direc- - L0 C...J L'j tor, and under the sponsorship of 4 " r th Egyptian Ministry of Social !.Zl ij1.,1,,.B= r,L..,J1....J Affairs and the U.S. Agency for - .Jt , . -t. International Development. These materials were designed for use in . J L.Jt CSziJtAJI #&h* - L*J training CAPP related instructors t .L-- -- J and supervisors for the various programs of the Ministry of Social ._ . , .. .. Affairs and to provide such person- L , *i. l I-JL-j 6 h nel with a systematica,'ly organized und detailed curriculum plan which JL61tJ J..i..- J" could be verbally transferred to O| ->. -

Key Details We Look for at Inspection
Key Details We Look for at Inspection Please not that these lists are not all inclusive but highlight areas that most often cause difficulty. Additional details are included on spec sheets for individual costumes. Boys’ Costumes Achterhoek: 1. Overall appearance of costume 2. Do you have the correct hat? This is the high one. Volendam is shorter. 3. The collar extends to the edge of the shirt and can be comfortably buttoned at the neck. 4. Ring on scarf and is visible above vest. If necessary use a gold safety pin to hold the ring in place. 5. Is the scarf on the inside of the vest, front and back? 6. Shirt buttons are in the center of the front band 7. The vest closes left over right. 8. The chain is in the 2nd buttonhole from the bottom 9. Welt pockets are made correctly and in the correct position. 10. Pants clear shoes. 11. Pants have a 6” hem Marken: 1.Overall appearance of costume 2.Red shirt underneath jacket 3.Red stitching on jacket placket 4.Closes as a boy (L. over R.) 5.Pants at mid-calf when pulled straight 6.Pants down 1” from waist Nord Holland Sunday: 1. Overall appearance of costume 2. Correct hat and scarf 3. Neck - can fit 1 finger 4. 2 dickies (one solid and one striped) 5. Jacket - collar flaps lay smooth 6. Buttonholes are horizontal 7. Jacket closes as a boy (left over right) 8. Cord, hook and eye at back of pants 9. Pants clear shoes 10.6 inch hem Noord Holland Work: 1. -
Coats & Clark Surelock Serging Thread in a Contrasting Color Coats
HIP PATCHWORK TUNIC Lori Harder PO BOX 472147, CHARLOTTE, NC 28247 USA SEWING I SKILL LEVEL: INTERMEDIATE Featuring Coats & Clark Surelock Thread Fashion a patchwork tunic from recycled sweaters for a cute back-to- school look. Give it a deconstructed look by overlocking the seams on the right side of the tunic. MEASUREMENTS pattern piece this wide at the Girls 5/6 (adaptations given for top + 3/8” on each side for seam other sizes) allowance. For the width of the bottom of the pattern piece CUTTING add 1 inch or more to the above Prepare the sweater. measurement. To determine 1. Measure down from the length of pattern piece have shoulder seams to bustline child try on sweater and measure - approximately 6 ¾” for a from bustline down to desired girl’s size 5/6 and cut sweater length at hips and subtract 1 ½” around bustline. Use lower for the band. For the band use section of sweater to cut 2 the bustline measurement of the MATERIALS bands. sweater divided by 2 x 2 ¼”). Coats & Clark Surelock Serging Thread in a contrasting color 2. Cut 2 bands 2 ¼” x 12 ¾” cross Coats & Clark Button and Craft thread* grain for waistband SEWING 1 Fitted sweater 3. From the other sweater 4. Skirt: Pin one color sweater 3 or 4 colors of sweater fabric fabrics, cut 12 pieces of fabric to another at sides, Buttons * various colors using the wrong sides together and Serger/Overlock Sewing Machine pattern piece serge - stretching as you sew Pins to make the ru ed lettuce Scissors NOTE: If making a di erent size edge e ect. -

Trims, Labels, Treads, Elastics, Underlying Fabrics, Zippers, Butto
10/12/2009 1 TRIMS AND FINDINGS Chapter 8 2 Findings and Trims Findings: trims, labels, treads, elastics, underlying fabrics, zippers, buttons, other closures, other miscellaneous items Trims: subdivision of findings – decorative materials – ribbons, braids, laces, other narrow fabric trims, appliqués, flowers, beads, sequins, other decorative items Findings/trims usually aren’t the reason for purchase but they are often the reason for discarding a garment 3 Performance Finding/trim must reflect same quality level as the fabric Performance of finding or trim could negate the performance of the body fabric Ex. If fabric is dry-clean only, the trims must be dry-cleanable 4 Establishing specs Often established by the suppliers themselves or by the manufacturers in partnership w/ the suppliers Too many types of findings and trims to be an expert on all and be able to write accurate specs on all – best to rely on the supplier of the specific type of finding you need 5 Aesthetic performance Must complement the appearance of the garment Must be considered in concert with the design, construction, and finish of the garment Need to be attractive, fashionable, and functional to help sell the garment 6 Functional Performance Includes utility and durability of the finding Utility includes: dimensional stability, appearance retention, comfort, ease of care, and safety Durability includes: strength, abrasion resistance, and degradation by chemical & other elements 7 Performance, Cont. Design, materials, and constructions of a garment interact to determine -

Facts About Fitting Agricultural Extension Service
South Dakota State University Open PRAIRIE: Open Public Research Access Institutional Repository and Information Exchange SDSU Extension Circulars SDSU Extension 1960 Facts about Fitting Agricultural Extension Service Follow this and additional works at: http://openprairie.sdstate.edu/extension_circ Part of the Agriculture Commons Recommended Citation Service, Agricultural Extension, "Facts about Fitting" (1960). SDSU Extension Circulars. 618. http://openprairie.sdstate.edu/extension_circ/618 This Circular is brought to you for free and open access by the SDSU Extension at Open PRAIRIE: Open Public Research Access Institutional Repository and Information Exchange. It has been accepted for inclusion in SDSU Extension Circulars by an authorized administrator of Open PRAIRIE: Open Public Research Access Institutional Repository and Information Exchange. For more information, please contact [email protected]. • Extension Circular 593 FITTING \ ' ' ' ' ' ' ' ' .,,_-, ' , ...... ' ' I ' \ \ ' ' I • ' ' ' ' ..... -- -- ' - COOPERATIVE EXTENSION SERVICE SOUTH DAKOTA STATE UNIVERSITY, BROOKINGS U. S. DEPARTMENT OF AGRICULTURE FACTS ABOUT • • • F I T T I N G A garment that fits well looks as if it "belongs" to are square shoulders, wide shoulders, narrow sloping . he wearer. Such a garment adapts itself to the stand- shoulders, rounded shoulders in the back, prominent ing, sitting, and moving positions of the person wear- back hips or side hips, sway back ( exaggerated hollow ing it. It is neither too loose nor too tight and it feel s at the waistline), large upper arm, very thin arms, and looks comfortable. It brings out the good points in short or long arms, short or long waist. the individual's figure and skillfully hides poor ones. Insuring a good fit may depend on fitting after the Begin With the Pattern basic fitting dress is cut and basted or after the ready- it is important then, if you are going to make a gar- made dress is bought. -

Sewing Math: How to Add, Subtract, Multiply & Divide
PAGE 8 KITCHEN-KLATTER MAGAZINE, SEPTEMBER, 1974 it's gathered and full, the best proce dure is to sew the skirt to the bottom of the bodice and add an attractive purchased belt. If it's fairly straight or A-line, you can do that, or you can set SEWING MATH: it on flat and neat to the knit bodice, turn the seam upward (again toward the HOW TO ADD, knit) and topstitch. It's entirely possi SUBTRACT, ble, if your girl needs even more MULTIPLY & DIVIDE length, to cut the knit bodice long enough for a dropped waistline; then by Mary Feese the "new" dress can be worn with or without a belt, as its wearer prefers. As you re-use fabrics, you'll find buttons, zippers, and some trim that you don't need for the project in hand, yet that are too good to throw away. You look at that title and wonder, figures, the problems are somewhat Save them! Small buttons store well in "What on earth does that mean?" Well, different. Anything that fits this month pill bottles; larger ones can be put simply this: you can add, subtract, may not do so next month! Let's say into plastic sandwich bags to keep multiply, and divide with items of she has a good dress, whose fabric is them together, yet easily visible. To clothing your family already owns. Re well worth redoing - but there's just re-use zippers and various trims, take cycle, alter, remake, restyle, hand no room in the bustline. The "tank the time to spray-starch and press them down, freshen up - and come out with top" idea can solve this one. -
Em2246 1962.Pdf
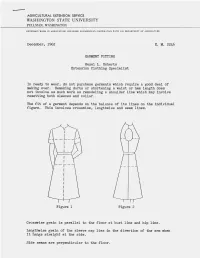
AGRICULTURAL EXTENSION SERVICE WASHINGTON STATE UNIVERSITY PULLMAN, WASHINGTON EXTENSION WORK IN AGRICULTURE AND HOME ECONOMICS IN COOPERATION W ITH U.S. DEPARTMENT OF AGRICULTURE December, 1962 E. M. 2246 GARMENT FITTING Hazel L. Roberts Extension Clothing Specialist In ready to wear, do not purchase garments which require a good deal of making over. Remaking darts or shortening a waist or hem length does not involve as much work as remodeling a shoulder line which may involve resetting both sleeves and collar. The fit of a garment depends on the balance of its lines on the individual figure. This involves crosswise, lengthwise and seam lines. Figure 1 Figure 2 Crosswise grain is parallel to the floor at bust line and hip line. Lengthwise grain of the sleeve cap lies in the direction of the arm when it hangs straight at the sidee Side seams are perpendicul ar to the floor. E.M. 2246 Page 2 SOME COMMON FITTING PROBLEMS TO FIT THE BODICE, KEEP THE CROSSWISE GRAIN OF THE FABRIC STRAIGHT ACROSS THE BUSTLINE - Shoulder line too long - in addition to being uncomfortable the too long shoulder line may pull the neckline from the side of the neck. Rip out the sleeve and recut armhole using a pattern as a guide. It is best to shorten the shoulder line in the pattern before the garment is cut. - Shoulder line too short. If the fabric is firm, make a smaller seam at the armhole shoulder line. Lengthen the shoulder line of the pattern be fore cutting the garment. - Shoulders too square for shoulder line of garment - indicated by diagonal wrinkles from shoulder tip to center front or back. -

It's All in the Details: Making an Early 19Th Century Ball Gown by Hope Greenberg
It's All in the Details: Making an early 19th Century Ball Gown By Hope Greenberg In 1775, the year of Jane Austen’s birth, women wore gowns with a fitted bodice, the waist at or below the natural waistline, and full skirts over a visible, often ornate, petticoat. They were made in a variety of heavy silks, cotton or wool. By the time she had reached her late teens the ornate gowns were being replaced by simple, lightweight, often sheer cotton or silk gowns that reflected the ideals of classicism. This guide provides images and details to consider when creating an early 19th century ballgown. The examples provide a general guide, not an exact historic timeline. Fashion is flexible: styles evolve and are adopted at a different pace depending on the wearer's age, location, and economic or social status. These examples focus on evening or ball gowns. Day dresses, walking dresses, and carriage dresses, while following the same basic silhouettes, have their own particular design details. Even evening gowns or opera gowns can usually be distinguished from ball gowns which, after all, must be designed for dancing! By focusing on the details we can see both the evolution of fashion for this period and how best to re-create it. What is the cut of the bodice, the sleeve length, or the height of the bustline? How full is the skirt, and where is that fullness? What colors are used? What type of fabric? Is there trim? If so, how much, what kind, and where is it placed? Based on the shape of the gown, what can we tell about the foundation garments? Paying attention to all these details will help you create a gown that is historically informed as well as beautiful. -

Home Healthcare Product Guide
Home Healthcare Product Guide 2014-15 Healthcare Home Contact a Cardinal Health Home Healthcare Specialist for more information. Front-end solutions Home Healthcare Product Guide cardinalhealth.com Cardinal Health © 2014 Cardinal Health. All rights reserved. CARDINAL HEALTH, Healthcare Supply Chain Services the Cardinal Health LOGO, and Essential to care are trademarks or registered trademarks of Cardinal Health. All other marks are the 7000 Cardinal Place property of their respective owners. Lit. No. 1CHP14-14120 (07/2014) Dublin, Ohio 43017 Table of Contents Aids to Daily Living Elbow ...........................................................................48-50 Exercise/Physical Therapy 108-113 (Compliance Aids) 6-18 Hand .............................................................................50-51 Electro Therapy ...................................................108-109 Bath and Hygiene Aids ...............................................6-7 Wrist .............................................................................51-55 Exercise Aids ........................................................109-111 Daily Activities ............................................................ 8-10 Thumb .........................................................................55-57 Body Fat Analyzers/ Ear, Eye and Nose Aids ..........................................10-11 Hernia ................................................................................ 57 Heart Rate Monitors/Oximeter ...............................111 Medication -

Buttons & Buttonholes
CT-MMB.189 BUTTONS & BUTTONHOLES BUTTONS Selection Button selection depends on the type and style Buttons can be fascinating, functional, and of the garment. Buttons should be selected fashionable. They are fascinating because of their BEFORE making buttonholes or button loops. many sizes, shapes, colors, and designs. They are Consider the following when making your functional because they are one of the major selection: methods of opening and closing garments. Buttons are fashionable because they also decorate and $ The pattern will have a suggested size which enhance apparel & other items. was determined as the pattern was being made. If the button size is changed, so must the size of the button and buttonhole placket. $ Weight of fabric B Heavy fabric needs heavier and larger buttons; lighter fabric needs lighter and smaller buttons. $ Fabric design B Buttons can blend with the History fabric OR they can call attention to the area. The term is from the French word, bouton, To call attention to the area use solid colored meaning a round object. Since the 13th century, buttons on prints and patterned buttons on buttons have been used as fasteners. Before that, solid color fabrics. they were used more for their decorative and symbolic value. Today, buttons continue to be used as decoration, but their placement once served a useful purpose. For instance buttons on the back of men’s coats served as a way to fasten coat tails up out of the $ Use a smooth, flat-textured button on smooth way when riding on horseback. During Frederick textured fabrics. Shiny buttons are best on the Great=s reign, it was customary for three decorative, shiny fabrics. -

It's All in the Details: Making an Early 19Th Century Ball Gown by Hope Greenberg
It's All in the Details: Making an early 19th Century Ball Gown By Hope Greenberg In 1775, the year of Jane Austen’s birth, women wore gowns with a fitted bodice, the waist at or below the natural waistline, and full skirts over a visible, often ornate, petticoat. They were made in a variety of heavy silks, cotton or wool. By the time she had reached her late teens the ornate gowns were being replaced by simple, lightweight, often sheer cotton or silk gowns that reflected the ideals of classicism. This guide provides images and details to consider when creating an early 19th century ballgown. The examples provide a general guide, not an exact historic timeline. Fashion is flexible: styles evolve and are adopted at a different pace depending on the wearer's age, location, and economic or social status. These examples focus on evening or ball gowns. Day dresses, walking dresses, and carriage dresses, while following the same basic silhouettes, have their own particular design details. Even evening gowns or opera gowns can usually be distinguished from ball gowns which, after all, must be designed for dancing! By focusing on the details we can see both the evolution of fashion for this period and how best to re-create it. What is the cut of the bodice, the sleeve length, or the height of the bustline? How full is the skirt, and where is that fullness? What colors are used? What type of fabric? Is there trim? If so, how much, what kind, and where is it placed? Based on the shape of the gown, what can we tell about the foundation garments? Paying attention to all these details will help you create a gown that is historically informed as well as beautiful.