Mutagen Treatment As a Means for Selecting Immunogenic Variants from Otherwise Poorly Immunogenic Malignant Murine Tumors1
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Toxicological Profile for Radon
RADON 205 10. GLOSSARY Some terms in this glossary are generic and may not be used in this profile. Absorbed Dose, Chemical—The amount of a substance that is either absorbed into the body or placed in contact with the skin. For oral or inhalation routes, this is normally the product of the intake quantity and the uptake fraction divided by the body weight and, if appropriate, the time, expressed as mg/kg for a single intake or mg/kg/day for multiple intakes. For dermal exposure, this is the amount of material applied to the skin, and is normally divided by the body mass and expressed as mg/kg. Absorbed Dose, Radiation—The mean energy imparted to the irradiated medium, per unit mass, by ionizing radiation. Units: rad (rad), gray (Gy). Absorbed Fraction—A term used in internal dosimetry. It is that fraction of the photon energy (emitted within a specified volume of material) which is absorbed by the volume. The absorbed fraction depends on the source distribution, the photon energy, and the size, shape and composition of the volume. Absorption—The process by which a chemical penetrates the exchange boundaries of an organism after contact, or the process by which radiation imparts some or all of its energy to any material through which it passes. Self-Absorption—Absorption of radiation (emitted by radioactive atoms) by the material in which the atoms are located; in particular, the absorption of radiation within a sample being assayed. Absorption Coefficient—Fractional absorption of the energy of an unscattered beam of x- or gamma- radiation per unit thickness (linear absorption coefficient), per unit mass (mass absorption coefficient), or per atom (atomic absorption coefficient) of absorber, due to transfer of energy to the absorber. -

Toxicological Profile for Hydrazines. US Department Of
TOXICOLOGICAL PROFILE FOR HYDRAZINES U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Agency for Toxic Substances and Disease Registry September 1997 HYDRAZINES ii DISCLAIMER The use of company or product name(s) is for identification only and does not imply endorsement by the Agency for Toxic Substances and Disease Registry. HYDRAZINES iii UPDATE STATEMENT Toxicological profiles are revised and republished as necessary, but no less than once every three years. For information regarding the update status of previously released profiles, contact ATSDR at: Agency for Toxic Substances and Disease Registry Division of Toxicology/Toxicology Information Branch 1600 Clifton Road NE, E-29 Atlanta, Georgia 30333 HYDRAZINES vii CONTRIBUTORS CHEMICAL MANAGER(S)/AUTHOR(S): Gangadhar Choudhary, Ph.D. ATSDR, Division of Toxicology, Atlanta, GA Hugh IIansen, Ph.D. ATSDR, Division of Toxicology, Atlanta, GA Steve Donkin, Ph.D. Sciences International, Inc., Alexandria, VA Mr. Christopher Kirman Life Systems, Inc., Cleveland, OH THE PROFILE HAS UNDERGONE THE FOLLOWING ATSDR INTERNAL REVIEWS: 1 . Green Border Review. Green Border review assures the consistency with ATSDR policy. 2 . Health Effects Review. The Health Effects Review Committee examines the health effects chapter of each profile for consistency and accuracy in interpreting health effects and classifying end points. 3. Minimal Risk Level Review. The Minimal Risk Level Workgroup considers issues relevant to substance-specific minimal risk levels (MRLs), reviews the health effects database of each profile, and makes recommendations for derivation of MRLs. HYDRAZINES ix PEER REVIEW A peer review panel was assembled for hydrazines. The panel consisted of the following members: 1. Dr. -

Detection of Carcinogens As Mutagens in the Salmonella/Microsome Test
Proc. Nat. Acad. Sci. USA Vol. 73, No. 3, pp. 950-954, March 1976 Medical Sciences Detection of carcinogens as mutagens in the Salmonella/microsome test: Assay of 300 chemicals: Discussion* (prevention of cancer and genetic defects/somatic mutation/environmental insult to DNA) JOYCE MCCANN AND BRUCE N. AMES Department of Biochemistry, University of California, Berkeley, Calif. 94720 Contributed by Bruce N. Ames, January 7, 1976 ABSTRACT About 300 carcinogens and non-carcinogens Non-Carcinogens. Classification as to non-carcinogenicity of a wide variety of chemical types have been tested for mu- is usually difficult because of the varying completeness and tagenicity in the simple Salmonella/microsome test. The test uses bacteria as sensitive indicators of DNA damage, and modes of treatment in many studies and the statistical limi- mammalian liver extracts for metabolic conversion of carcin- tations inherent in animal tests (4, 8-10). Recent criteria for ogens to their active mutagenic forms. There is a high corre- adequate carcinogenicity tests are much more stringent (4, lation between carcinogenicity and mutagenicity: 90% 8-10). The test should be of adequate duration (lifetime pre- (157/175) of the carcinogens were mutagenic in the test, in- ferred in rodents) in at least two animal species, at several cluding almost all of the known human carcinogens that dose levels, and positive controls should be of the same gen- were tested. Despite the severe limitations inherent in defin- ing non-carcinogenicity, few "non-carcinogens" showed any eral chemical type as the chemical under test. The applica- degree of mutagenicity [McCann et a]. (1975) Proc. -

Lead, Mercury and Cadmium in Fish and Shellfish from the Indian Ocean and Red
Journal of Marine Science and Engineering Review Lead, Mercury and Cadmium in Fish and Shellfish from the Indian Ocean and Red Sea (African Countries): Public Health Challenges Isidro José Tamele 1,2,3,* and Patricia Vázquez Loureiro 4 1 Department of Chemistry, Faculty of Sciences, Eduardo Mondlane University, Av. Julius Nyerere, n 3453, Campus Principal, Maputo 257, Mozambique 2 Institute of Biomedical Science Abel Salazar, University of Porto, R. Jorge de Viterbo Ferreira 228, 4050-313 Porto, Portugal 3 CIIMAR/CIMAR—Interdisciplinary Center of Marine and Environmental Research, University of Porto, Terminal de Cruzeiros do Porto, Avenida General Norton de Matos, 4450-238 Matosinhos, Portugal 4 Department of Analytical Chemistry, Nutrition and Food Science, Faculty of Pharmacy, University of Santiago de Compostela, Santiago de Compostela, 15782 A Coruña, Spain; [email protected] * Correspondence: [email protected] Received: 20 March 2020; Accepted: 8 May 2020; Published: 12 May 2020 Abstract: The main aim of this review was to assess the incidence of Pb, Hg and Cd in seafood from African countries on the Indian and the Red Sea coasts and the level of their monitoring and control, where the direct consumption of seafood without quality control are frequently due to the poverty in many African countries. Some seafood from African Indian and the Red Sea coasts such as mollusks and fishes have presented Cd, Pb and Hg concentrations higher than permitted limit by FAOUN/EU regulations, indicating a possible threat to public health. Thus, the operationalization of the heavy metals (HM) monitoring and control is strongly recommended since these countries have laboratories with minimal conditions for HM analysis. -

Food-Derived Mutagens and Carcinogens1
[CANCER RESEARCH (SL'PPL.) 52. 2092s-2098s. April I, 1992] Food-derived Mutagens and Carcinogens1 Keiji Wakabayashi,2 Minako Nagao, Hiroyasu Esumi, and Takashi Sugimura National Cancer Center Research Institute, l-l, Tsukiji 5-chome, Chuo-ku, Tokyo 104, Japan Abstract pounds have planar structures that can be inserted between the base pairs of double-stranded DNA. Charred parts of broiled Cooked food contains a variety of mutagenic heterocyclic amines. All the mutagenic heterocyclic amines tested were carcinogenic in rodents fish and meat were also found to be mutagenic to TA98 after when given in the diet at 0.01-0.08%. Most of them induced cancer in metabolic activation (9, 10). These findings led to the isolations the liver and in other organs. It is noteworthy that the most abundant of the mutagenic compounds, IQ,' MelQ, MelQx from broiled heterocyclic amine in cooked food, 2-amino-l-methyl-6-phenylimi- fish and meat (5-7). Later PhIP was also isolated as member dazo(4,5-A|pyridine, produced colon and mammary carcinomas of this class of mutagens (11). These heterocyclic amines were in rats and lymphomas in mice but no hepatomas in either. 2-Amino-3- methylimidazo(4,5-/]quinoline induced liver cancer in monkeys. Forma formed by heating mixtures of creatinine, sugars, and amino acids, which are present in raw meat and fish (12-16). More tion of adducts with guanine by heterocyclic amines is presumably involved in their carcinogenesis. Quantification of heterocyclic amines in recently identified mutagens have been found to contain oxygen cooked foods and in human urine indicated that humans are continuously atoms (17-19). -

Appendix G Restricted Chemicals
APPENDIX G RESTRICTED CHEMICALS CHEMICAL NAME REASON FOR RESTRICTION Acetaldehyde Suspected carcinogen, highly flammable Acetamide Suspected animal carcinogen Acrylamide Suspected carcinogen, absorbs through skin AITCH-TU-ESS Cartridges Generates explosive and toxic gas (HIGH SCHOOL ONLY) Aldrin Suspected carcinogen, absorbs through skin Allyl Chloride Suspected carcinogen Aluminum Chloride, Anhydrous Water reactive; corrosive (Hydrate Salts Are Allowed) Ammonium Bichromate Oxidizer, corrosive, known human carcinogen Ammonium Nitrate AP/IB CHEMISTRY ONLY: Explosive if heated under confinement Ammonium Oxalate May be fatal if inhaled or ingested Ammonium Vanadate May be fatal if inhaled or ingested Anisidine (o-, p-isomers) Suspected carcinogen Barium Chloride Severely toxic; 0.8 gram fatal dose Barium Hydroxide Highly toxic, neurotoxin Barium Nitrate Poison, strong oxidant, highly toxic to eyes Benzone (Phenylbutazone) Irritant Benzo(a)pyrene Suspected carcinogen Bromine Poison, powerful oxidizer Bromoform Toxic by inhalation, unsuspected carcinogen iso-Butanol Suspected carcinogen, highly flammable sec-Butanol May form explosive hydroperoxides tert-Butanol Suspected carcinogen and mutagen, highly flammable 1,3-Butadiene Suspected carcinogen Caffeine Very toxic, 1 grain may be life threatening Calcium Carbide Flammable, reacts with water Calcium Chromate Suspected carcinogen Calcium Fluoride Mutagenic effects in animals, poison, toxic to humans Calcium Oxide Corrosive, irritating Carbol Fuchsin Suspect animal carcinogen and mutagen Carmine -

Carcinogens and Reproductive Toxicants
Facilities Management Environmental Health and Safety Principal Investigator: Date Approved: This document covers basic chemical safety information for carcinogens and reproductive toxicants. The use of any carcinogen or reproductive toxicant is subject to pre-approval by the Toxic Substances Committee. DO NOT USE CARCINOGENS OR REPRODUCTIVE TOXICANTS UNTIL YOU HAVE OBTAINED THE NECESSARY APPROVAL. Carcinogens and Reproductive Toxicants Refer to the University of Arkansas Chemical Hygiene Plan for a description of chemicals that will be considered as a Particularly Hazardous Substance (PHS) carcinogen or reproductive toxicant. Chemicals that meet the definition of a PHS carcinogen or reproductive toxicant must be used only in a designated area where limited access, special procedures, knowledge, and work skills are required. A designated area can be the entire laboratory, a specific laboratory workbench, or a laboratory hood. Designated areas must be clearly marked with signs that identify the chemical hazard and include an appropriate warning; for example: WARNING! CARCINOGEN/ REPRODUCTIVE TOXICANT WORK AREA Carcinogens are materials that have the potential to cause cancer. Reproductive toxicants are materials that have the potential to interfere with fertility, fetal development, and/or lactation. Mutagens are materials that can cause genetic mutations. Such mutations can often lead to cancer or reproductive toxicity. Please note that the use of Listed Carcinogens, halogenated liquids, ethidium bromide, and formaldehyde is not covered by this general SOP. Exposure, Signs and Symptoms and Chemical Properties Review the appropriate sections of the chemical specific Safety Data Sheet (SDS) for information on ways to detect exposure, appropriate exposure limits, signs and symptoms of exposures and chemical properties. -

OECD Environmental Health and Safety Publications
Unclassified ENV/JM/MONO(99)2 Organisation de Coopération et de Développement Economiques OLIS : 16-Feb-1999 Organisation for Economic Co-operation and Development Dist. : 17-Feb-1999 __________________________________________________________________________________________ English text only ENVIRONMENT DIRECTORATE Unclassified ENV/JM/MONO(99)2 JOINT MEETING OF THE CHEMICALS COMMITTEE AND THE WORKING PARTY ON CHEMICALS OECD SERIES ON TESTING AND ASSESSMENT Number 12 Detailed Review Document on Classification Systems for Germ Cell Mutagenicity in OECD Member Countries English textEnglish only 74491 Document complet disponible sur OLIS dans son format d'origine Complete document available on OLIS in its original format ENV/JM/MONO(99)2 2 ENV/JM/MONO(99)2 OECD Environmental Health and Safety Publications Series on Testing and Assessment No. 12 Detailed Review Document on Classification Systems for Germ Cell Mutagenicity in OECD Member Countries Environment Directorate ORGANISATION FOR ECONOMIC CO-OPERATION AND DEVELOPMENT Paris 1999 3 ENV/JM/MONO(99)2 Also published in the Series on Testing and Assessment: No. 1, Guidance Document for the Development of OECD Guidelines for Testing of Chemicals (1993; reformatted 1995) No. 2, Detailed Review Paper on Biodegradability Testing (1995) No. 3, Guidance Document for Aquatic Effects Assessment (1995) No. 4, Report of the OECD Workshop on Environmental Hazard/Risk Assessment (1995) No. 5, Report of the SETAC/OECD Workshop on Avian Toxicity Testing (1996) No. 6, Report of the Final Ring-test of the Daphnia magna Reproduction Test (1997) No. 7, Guidance Document on Direct Phototransformation of Chemicals in Water (1997) No. 8, Report of the OECD Workshop on Sharing Information about New Industrial Chemicals Assessment (1997) No. -

Carcinogens and Mutagens Fact Sheet
Carcinogens and Mutagens Fact Sheet This fact sheet is for general safety awareness. Individual Standard Operating Procedures for all experiments and processes involving carcinogens or mutagens must be developed by the laboratory. PROPERTIES & HAZARDS Carcinogens are chemicals that are known or suspected to cause cancer in humans. Cancer is a chronic effect and is typically the result of repeated or long-term exposure. Symptoms may develop many years after exposure. A known human carcinogen means there is sufficient evidence of a cause and effect relationship between exposure to the material and cancer in humans. A substance that has induced cancer in experimental animal studies is referred to as a suspected human carcinogen. Mutations are defined as causing a permanent change in the amount or structure of the genetic material in a cell. The term mutation applies both to heritable genetic changes that may be manifested at the phenotypic level and to the underlying DNA modifications when known. This hazard class is primarily concerned with chemicals that may cause mutations in the germ cells of humans that can be transmitted to the progeny. However, mutagenicity/genotoxicity tests in vitro and in mammalian somatic cells in vivo are also considered in classifying substances and mixtures within this hazard class. There are three categories for carcinogens and mutagens, Category 1A, 1B and 2, that you may see on the safety data sheet (SDS) or chemical bottle. In Section 2 – Hazard Identification of the SDS, a combination of the following hazard classifications, pictograms and hazard statements will be listed indicating a carcinogen or mutagen hazard. -

PROVISIONAL PEER-REVIEWED TOXICITY VALUES for O-PHENYLENEDIAMINE (CASRN 95-54-5)
EPA/690/R-16/007F l Final 09-27-2016 Provisional Peer-Reviewed Toxicity Values for o-Phenylenediamine (CASRN 95-54-5) Superfund Health Risk Technical Support Center National Center for Environmental Assessment Office of Research and Development U.S. Environmental Protection Agency Cincinnati, OH 45268 AUTHORS, CONTRIBUTORS, AND REVIEWERS CHEMICAL MANAGERS Elizabeth Owens, PhD National Center for Environmental Assessment, Cincinnati, OH Letitia Wong, PhD Oak Ridge Institute for Science and Education Research Participation Program National Center for Environmental Assessment, Cincinnati, OH DRAFT DOCUMENT PREPARED BY SRC, Inc. 7502 Round Pond Road North Syracuse, NY 13212 PRIMARY INTERNAL REVIEWER Suryanarayana Vulimiri, PhD National Center for Environmental Assessment, Research Triangle Park, NC This document was externally peer reviewed under contract to: Eastern Research Group, Inc. 110 Hartwell Avenue Lexington, MA 02421-3136 Questions regarding the contents of this PPRTV assessment should be directed to the EPA Office of Research and Development’s National Center for Environmental Assessment, Superfund Health Risk Technical Support Center (513-569-7300). ii o-Phenylenediamiamine TABLE OF CONTENTS COMMONLY USED ABBREVIATIONS AND ACRONYMS .................................................. iv BACKGROUND .............................................................................................................................1 DISCLAIMERS ...............................................................................................................................1 -

The Calculation of Median Lethal Dose (LD50) and Maximum Permissible Dose (MPD) Values of Sodium Arsenite in Female Swiss Albino Mice
IOSR Journal of Environmental Science, Toxicology and Food Technology (IOSR-JESTFT) e-ISSN: 2319-2402,p- ISSN: 2319-2399.Volume 12, Issue 9 Ver. I (September. 2018), PP 89-91 www.iosrjournals.org The Calculation of Median Lethal Dose (LD50) And Maximum Permissible Dose (MPD) Values of Sodium Arsenite In Female Swiss Albino Mice *Shailendra Kumar And Preety Sinha Departement of Zoology, A. N. College, Patna, Bihar, India. Corresponding Author: Shailendra Kumar Abstract: Sodium arsenite is an environmental pollutant and is responsible for both knowing poisonings and accidental exposures that can cause harmful health issues and possibly death. Median lethal dose (LD50) is a statistically obtained dose of a compound that can be predicted to cause death in 50% of the mice when administered by a specific route as a single dose and mice noticed for a specific time period. In the present research, different doses i.e., 6, 9, 12, 15, 18, 21 and 24 mg/kg body weight of Sodium arsenite was given orally by gavage method to the seven different groups of Swiss albino mice. Signs and symptoms of toxicity and probable death of mice were observed for 3 hours and then at 6, 12, 24, 48 and 72 hours to calculate the Median lethal dose (LD50) and maximum permissible dose (MPD) of Sodium arsenite. The LD50 was found to 18 mg/kg body weight after oral administration in Swiss albino mice. Finally, MPD of Sodium arsenite by oral route in mice was found to be 1.8 mg/kg body weight. Keywords: Sodium arsenite, Swiss albino mice, LD50, MPD ----------------------------------------------------------------------------------------------------------------------------- ---------- Date of Submission: 27-08-2018 Date of acceptance: 11-09-2018 ----------------------------------------------------------------------------------------------------------------------------- ---------- I. -
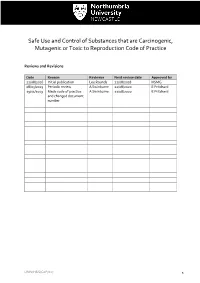
Safe Use and Control of Substances That Are Carcinogenic, Mutagenic Or Toxic to Reproduction Code of Practice
Safe Use and Control of Substances that are Carcinogenic, Mutagenic or Toxic to Reproduction Code of Practice Reviews and Revisions Date Reason Reviewer Next review date Approved by 22/08/2016 Initial publication Lee Rounds 22/08/2018 HSMG 08/05/2019 Periodic review A Swinburne 22/08/2020 E Pritchard 29/11/2019 Made code of practice A Swinburne 22/08/2020 E Pritchard and changed document number UNN/H&S/CoP/017 1 Contents Introduction ....................................................................................................................................... 3 General Principles .............................................................................................................................. 3 Definitions ......................................................................................................................................... 4 Responsibilities ................................................................................................................................. 6 Exposure Risk and Hazardous Properties Of Cmrs .............................................................................. 7 Accident/Incident Reporting ............................................................................................................. 10 University Procedures .................................................................................................................... 100 Training ...........................................................................................................................................