Advance Copy Air Pollution and Child Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1 1 DNA Barcodes Reveal Deeply Neglected Diversity and Numerous
Page 1 of 57 1 DNA barcodes reveal deeply neglected diversity and numerous invasions of micromoths in 2 Madagascar 3 4 5 Carlos Lopez-Vaamonde1,2, Lucas Sire2, Bruno Rasmussen2, Rodolphe Rougerie3, 6 Christian Wieser4, Allaoui Ahamadi Allaoui 5, Joël Minet3, Jeremy R. deWaard6, Thibaud 7 Decaëns7, David C. Lees8 8 9 1 INRA, UR633, Zoologie Forestière, F- 45075 Orléans, France. 10 2 Institut de Recherche sur la Biologie de l’Insecte, UMR 7261 CNRS Université de Tours, UFR 11 Sciences et Techniques, Tours, France. 12 3Institut de Systématique Evolution Biodiversité (ISYEB), Muséum national d'Histoire naturelle, 13 CNRS, Sorbonne Université, EPHE, 57 rue Cuvier, CP 50, 75005 Paris, France. 14 4 Landesmuseum für Kärnten, Abteilung Zoologie, Museumgasse 2, 9020 Klagenfurt, Austria 15 5 Department of Entomology, University of Antananarivo, Antananarivo 101, Madagascar 16 6 Centre for Biodiversity Genomics, University of Guelph, 50 Stone Road E., Guelph, ON 17 N1G2W1, Canada 18 7Centre d'Ecologie Fonctionnelle et Evolutive (CEFE UMR 5175, CNRS–Université de Genome Downloaded from www.nrcresearchpress.com by UNIV GUELPH on 10/03/18 19 Montpellier–Université Paul-Valéry Montpellier–EPHE), 1919 Route de Mende, F-34293 20 Montpellier, France. 21 8Department of Life Sciences, Natural History Museum, Cromwell Road, SW7 5BD, UK. 22 23 24 Email for correspondence: [email protected] For personal use only. This Just-IN manuscript is the accepted prior to copy editing and page composition. It may differ from final official version of record. 1 Page 2 of 57 25 26 Abstract 27 Madagascar is a prime evolutionary hotspot globally, but its unique biodiversity is under threat, 28 essentially from anthropogenic disturbance. -

Safety of Immunization During Pregnancy a Review of the Evidence
Safety of Immunization during Pregnancy A review of the evidence Global Advisory Committee on Vaccine Safety © World Health Organization 2014 All rights reserved. Publications of the World Health Organization are available on the WHO website (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications –whether for sale or for non-commercial distribution– should be addressed to WHO Press through the WHO website (www.who.int/about/licensing/copyright_form/en/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters. All reasonable precautions have been taken by the World Health Organization to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. -
Hiv Prevention in Maternal Health Services Programming Guide
PREVENTING HIV,PROMOTING REPRODUCTIVE HEALTH HIV PREVENTION IN MATERNAL HEALTH SERVICES PROGRAMMING GUIDE HIV Prevention in Maternal Health Services: Programming Guide © 2004 UNFPA and EngenderHealth. All rights reserved. United Nations Population Fund 220 East 42nd Street New York, NY 10017 U.S.A. www.unfpa.org EngenderHealth 440 Ninth Avenue New York, NY 10001 U.S.A. Telephone: 212-561-8000 Fax: 212-561-8067 e-mail: [email protected] www.engenderhealth.org This publication was made possible through financial support provided by UNFPA. Design: Deb Lake Typesetting: ConsolidatedGraphics Cover design: Cassandra Cook Cover photo credits: Liz Gilbert, on behalf of the David and Lucile Packard Foundation Printing: Automated Graphics Systems, Inc. ISBN 0-89714-694-8 Printed in the United States of America. Printed on recycled paper. Library of Congress Cataloging-in-Publication data are available from the publisher. CONTENTS Acknowledgements v • Making Services Friendlier for Stigmatised Populations 55 Introduction 1 • Universal Precautions 57 • Why Was This Guide Developed? 3 • Safer Delivery Practises 58 • What Is Covered in This Guide? 5 • Staff Training 59 • How Was This Guide Developed? 6 • Facilitative Supervision 61 • Who Is This Guide For? 7 • Programme Resources 62 • How Can This Guide Be Used? 8 • How Is This Guide Organised? 8 Chapter 3: Training Topics 67 Chapter 1: Programme Planning 11 • Basic HIV and STI Orientation 69 • Planning Process 13 • Group Education Strategies 70 • Step 1: Needs Assessment 14 • Core Counselling -

Download Download
Agr. Nat. Resour. 54 (2020) 499–506 AGRICULTURE AND NATURAL RESOURCES Journal homepage: http://anres.kasetsart.org Research article Checklist of the Tribe Spilomelini (Lepidoptera: Crambidae: Pyraustinae) in Thailand Sunadda Chaovalita,†, Nantasak Pinkaewb,†,* a Department of Entomology, Faculty of Agriculture, Kasetsart University, Bangkok 10900, Thailand b Department of Entomology, Faculty of Agriculture at Kamphaengsaen, Kasetsart University, Kamphaengsaen Campus, Nakhon Pathom 73140, Thailand Article Info Abstract Article history: In total, 100 species in 40 genera of the tribe Spilomelini were confirmed to occur in Thailand Received 5 July 2019 based on the specimens preserved in Thailand and Japan. Of these, 47 species were new records Revised 25 July 2019 Accepted 15 August 2019 for Thailand. Conogethes tenuialata Chaovalit and Yoshiyasu, 2019 was the latest new recorded Available online 30 October 2020 species from Thailand. This information will contribute to an ongoing program to develop a pest database and subsequently to a facilitate pest management scheme in Thailand. Keywords: Crambidae, Pyraustinae, Spilomelini, Thailand, pest Introduction The tribe Spilomelini is one of the major pests in tropical and subtropical regions. Moths in this tribe have been considered as The tribe Spilomelini Guenée (1854) is one of the largest tribes and the major pests of economic crops such as rice, sugarcane, bean belongs to the subfamily Pyraustinae, family Crambidae; it consists of pods and corn (Khan et al., 1988; Hill, 2007), durian (Kuroko 55 genera and 5,929 species worldwide with approximately 86 genera and Lewvanich, 1993), citrus, peach and macadamia, (Common, and 220 species of Spilomelini being reported in North America 1990), mulberry (Sharifi et. -

1 Abbey Books; #4 Richard Abel Bookseller; 1973:1, S
M-106 BOOKSELLER’S CATALOGS A & R BOOKSELLERS; #1 ABACUS BOOKSHOP; #1 ABBEY BOOKS; #4 RICHARD ABEL BOOKSELLER; 1973:1, Sale edition; 1974: 1 ABI BOOKS; #10-11, 15, 22-23, 30; Edward Gordon Craig; 1982: Early autumn, Spring, Edward Gorey; 1983: Spring ABINGTON BOOKS; 1973: Autumn ABOUT BOOKS; #3, 9-10, 61-64, 67-69 BEN ABRAHMSON’S ARGUS BOOK SHOP; #1-5, 7-12, 14-17, 20-34, Along the north wall, Along the south wall, 383, 623, 626, 969, 975, 985, 1944: Oct. HERMAN ABROMSON; #5-6, 7-10, 12 ACADEMIC BOOK COLLECTION; #9 ACADEMY BOOK SHOP; #61 PAUL ADAMS; Botany ADCO SPORTS BOOK EXCHANGE; 1808 TO DATE RICHARD ADAMIAK; #29 RICHARD H. ADELSON; 1981: Spring ; 1983: Spring ; 1992-93: Winter; 1994-95: Winter ADS AUTOGRAPHS; #1-3, 6-10, 13 ADVENTURE BOOK STORE; #1 ; 1988: Nov. AEONIAN PRESS; 1 catalog (unnumbered/undated) AESOP BOOKS; #8 CHARLES AGVENT; #2-5 AHAB RARE BOOKS; #26-27 ALASTOR RARE BOOKS; #16 EDWIN ALBERT; #1 l ALBION BOOKS; #3-4; 1979: Dec. ALCAZAR BOOK SERVICE; #51, 156 ALDREDGE BOOK STORE; #53, 87, 89-90, 114-116 ALEX ALEC-SMITH; #10, 14/16, 18 ALEPH-BET BOOKS; #3, 8-12, 14, 32, 35, 38-41, 43-45, 49, 53, 65; 2004: April 19 ALEXANDERSON & KLOSINSKI BOOKSELLERS; #1-2 ALFA ANTIQUARIAN BOOKSELLER; #79 LIBRAIRIE ALIX; #1 D.C. ALLEN; #32-33, 36, 58, 60, 62 R.R. ALLEN BOOKS; #21, 66-67, 70, 74, 79, 81-82, 84, 86, 92-96; 1996 WILLIAM H. ALLEN BOOKSELLER; #189, 206, 219, 224-225, 227-228, 231-232, 235-236, 239, 244-245, 249-251, 254-256, 259-261, 264-266, 268, 271-273, 275-276, 279-281, 283-284, 287-288, 290-291, 293- 294, 296-297, 300-301, 303-305, 307, 310-311, 313-314, 316-318, 320-321, 323-324; Special mailing 20 DUNCAN M. -

Maternal Health Outcomes in Dc
MATERNAL HEALTH OUTCOMES IN DC: Why are Black Women Dying from Pregnancy- Professor Jocelyn Johnston American University PUAD 610.003 | April 26th, 2020 Related Complications in Wards 7 & 8? Nancy Erickson, Matthew Hufford, & Isabel Taylor OUR MOTIVATION CAUSES • The US ranks 60th in maternal mortality rate out of 187 ranked Policy nations, placing well behind other developed nations1. Unlike • In DC, Medicaid only pays for health services up to ing, affordable childcare, and job opportunities. other countries, the American mortality rate has increased over 60 days postpartum and 1-2 visits. the past 10 years2 even though 3 in 5 pregnancy-related deaths in • In DC, inequitable resource distribution, limited Race and History the USA are preventable3. number of health systems funded, and delayed • Many black women do not trust medical institu- • The DC maternal mortality rate is still almost 2 times the national passing of key legislation.10 tions due to a long history of mistreatment toward rate4 despite dramatic improvements since 2014.5 Within DC, African-Americans. Wards 7 and 8 experience the highest rates of women delaying Socioeconomics • Black women frequently experience disrespect, proce- prenatal care, smoking during pregnancy, preterm births, low • Nearly 97% of DC residents “It’s hard to repair birth weights, and infant mortality.6 have health insurance11; free dures without consent, rough preventative healthcare services 100 years of harmful handling, and dismissiveness Percentage of D.C. Women Who Initiated Prenatal Care by decisions with 5 years toward pain from doctors. 25 are underutilized. Ward and Trimester, 2015-2016 • There is insufficient research of positive ones.” Various studies have indicated into social determinants of ac- implicit racial bias among 100% - Kristina Wint, AMCHP 17 cessing preventative care in DC. -
50% Off List Copy
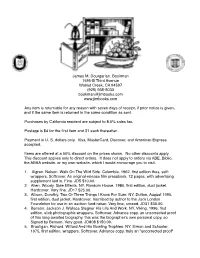
! ! ! ! ! ! James M. Dourgarian, Bookman! 1595-B Third Avenue! Walnut Creek, CA 94597! (925) 935-5033! [email protected]" www.jimbooks.com! ! Any item is returnable for any reason with seven days of receipt, if prior notice is given, and! if the same item is returned in the same condition as sent.! !Purchases by California resident are subject to 8.5% sales tax.! !Postage is $4 for the first item and $1 each thereafter.! Payment in U. S. dollars only. Visa, MasterCard, Discover, and American Express accepted.! ! Items are offered at a 50% discount on the prices shown. No other discounts apply. This discount applies only to direct orders. It does not apply to orders via ABE, Biblio, the! ABAA website, or my own website, which I would encourage you to visit.! 1. Algren, Nelson. Walk On The Wild Side. Columbia, 1962, first edition thus, self- wrappers. Softcover. An original-release film pressbook, 12 pages, with advertising supplement laid in. Fine. JD5 $10.00.! 2. Allen, Woody. Side Effects. NY, Random House, 1980, first edition, dust jacket. Hardcover. Very fine. JD17 $25.00.! 3. Allison, Dorothy. Two Or Three Things I Know For Sure. NY, Dutton, August 1995, first edition, dust jacket. Hardcover. Inscribed by author to the Jack London Foundation for use in an auction fund-raiser. Very fine, unread. JD31 $30.00.! 4. Benson, Jackson J. Wallace Stegner His Life And Work. NY, Viking, 1996, first edition, slick photographic wrappers. Softcover. Advance copy, an uncorrected proof of this long-awaited biography, this was the biographer's own personal copy, so Signed by Benson. -

120 Banned Books, Censorship Histories of World Literature
120 banned Books, second edition CENSORSHIP HISTORIES OF WORLD LITERATURE NICHOLAS J. KAROLIDES, MARGARET BALD AND DAWN B. SOVA To the University of Wisconsin–River Falls Chalmer Davee Library staff —N. J. K. For Jonathan, André and Daniel —M. B. To my son, Robert Gregor —D. B. S. 120 Banned Books, Second Edition Copyright © 2011 by Nicholas J. Karolides, Margaret Bald and Dawn B. Sova All rights reserved. No part of this book may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage or retrieval systems, without permission in writing from the publisher. For information contact: Checkmark Books An imprint of Infobase Learning 132 West 31st Street New York NY 10001 Library of Congress Cataloging-in-Publication Data Karolides, Nicholas J. 120 banned books : censorship histories of world literature / Nicholas J. Karolides, Margaret Bald, and Dawn B. Sova. — 2nd ed. p. cm. Includes bibliographical references and index. ISBN 978-0-8160-8232-2 (acid-free paper) 1. Censorship—United States—History—20th century. 2. Prohibited books—United States—History—20th century. 3. Challenged books—United States—History—20th century. 4. Censorship—History. 5. Prohibited books—United States—Bibliography. 6. Challenged books—United States—Bibliography. I. Bald, Margaret. II. Sova, Dawn B. III. Title. IV. Title: One hundred and twenty banned books. V. Title: One hundred twenty banned books. Z658.U5K35 2011 363.6'1—dc22 2011013099 Checkmark Books are available at special discounts when purchased in bulk quantities for businesses, associations, institutions, or sales promotions. Please call our Special Sales Department in New York at (212) 967-8800 or (800) 322-8755. -

Tackling Maternal Health Disparities: a Look at Four Local Organizations with Innovative Approaches
Tackling Maternal Health Disparities: A Look at Four Local Organizations with Innovative Approaches Maternal health disparities have many causes, but disparate social conditions and a lack of prenatal care or substandard maternal care are often key factors. Community-based maternal care models can help to narrow the disparities in maternal health outcomes by providing expanded prenatal, childbirth and postpartum support that is respectful and culturally relevant to at-risk women. These models may also focus on breastfeeding and parental development. This issue brief highlights four programs from across the country, examines the importance of community-based maternal care models and offers recommendations for supporting and expanding them. Maternal Health Disparities The United States has some of the worst rates of maternal and infant health outcomes among high-income nations, despite spending an estimated $111 billion per year on maternal, prenatal and newborn care.1 For example, Black, American Indian and Alaska Native2 women are more likely to experience complications during pregnancy and are nearly four times more likely to die from pregnancy or childbirth than white women.3 Latina, Asian and Pacific Islander women generally have birth outcomes that are similar to those of white women, but some reports show that certain subgroups fare worse than white women.4 National Partnership for Women & Families Tackling Maternal Health Disparities 1 Many of the poor maternal health outcomes that women of color experience are due to systemic barriers that create METHODOLOGY unequal social conditions. Compared to white women, women The National Partnership for Women of color are: & Families research team visited }}More likely to experience discrimination, which can increase Mamatoto Village in Washington, cortisol levels with adverse effects on maternal and infant DC and conducted the interview in person; the other three interviews took health.5 Racism can have negative consequences on the birth place as conference calls. -

Recommendations for Maternal Health and Infant Health Quality Improvement in Medicaid and the Children's Health Insurance Prog
Anchor Recommendations for Maternal Health and Infant Health Quality Improvement in Medicaid and the Children’s Health Insurance Program December 18, 2020 JudyAnn Bigby, Jodi Anthony, Ruth Hsu, Chrissy Fiorentini, and Margo Rosenbach Submitted to: Division of Quality & Health Outcomes Center for Medicaid and CHIP Services Centers for Medicare & Medicaid Services 7500 Security Blvd. Baltimore, MD 21244 Contracting Officer Representative: Deirdra Stockmann, Ph.D. Contract Number: HHSM-500-2014-00034I/75FCMC18F0002 Submitted by: Mathematica 955 Massachusetts Avenue Suite 801 Cambridge, MA 02139 Telephone: (617) 491-7900 Facsimile: (617) 491-8044 Project Director: Margo L. Rosenbach, Ph.D. Contents Introduction ................................................................................................................................................. 1 Poor outcomes and disparities call for urgent actions to improve maternal and infant health ............. 1 The role for Medicaid and CHIP to improve maternal and infant health .............................................. 2 Opportunities to Improve Maternal and Infant Health .................................................................................. 4 Maternal health ................................................................................................................................... 4 Infant health ........................................................................................................................................ 5 Recommendations ..................................................................................................................................... -

The Impact of Covid-19 on Maternal Health and Family Planning in Maldives the Impact of Covid-19 on Maternal Health and Family Planning in Maldives
THE IMPACT OF COVID-19 ON MATERNAL HEALTH AND FAMILY PLANNING IN MALDIVES THE IMPACT OF COVID-19 ON MATERNAL HEALTH AND FAMILY PLANNING IN MALDIVES The recent onset of the COVID-19 pandemic has threatened to become one of the most challenging tests faced by humanity in modern history, with governments facing multifaceted health and socio-economic challenges. Impacts can range from affecting livelihoods, increasing morbidity and mortality, overwhelming health systems, and triggering lasting geopolitical change. Maldives is currently implementing measures like lockdowns and travel bans. The consequential disruption of services on an already overstretched health system and the deviation of resources from essential sexual and reproductive humanitarian crises such as the 2004 Tsunami. The high health (SRH) services are expected to increase the risk of population density in Male’ compounds the likely social and maternal and child morbidity and mortality, as shown in past health impacts of COVID-19. 2 Compounded with the above factors, there could be an impact on the ability of women and couples to access family planning methods during this time. Some of the drivers of a potentially reduced access to contraceptive services include: ● Strict lockdown measures, disruption of continuity of essential SRH services including family planning, and limited access to such services; ● Geographical distribution of the country and scattered population on small islands may contribute to inaccessibility of proper maternal health services and facilities, and this is amplified during the current crisis; ● Contraceptive stocks are likely to run out and replenishing stocks is difficult because of restrictions of movement and limited service availability. -

2014 Integrated Africa Cancer Factsheet-Cervical+SRHR, HIV
! ! ! ! ! ! ! ! Advancing Multi-sectoral Policy & Investment for Girls, Women, & Children’s Health Information & Analysis on Health, Population, Human & Social Development !!!!!!!!!!!!! !!!!!!!! ! ! ! !! 2014%Integrated%Africa%Cancer%Factsheet%Focusing)on)Cervical)Cancer)+)) )Girls)&)Women)Health)/)Sexual)&)Reproductive)Health,)HIV)&)Maternal)Health% Figure 1: Cervical Cancer: Estimated Age-Standardised Rate (World / Regions) per 100,000 % Cervical Cancer At A Glance % Incidence / Prevalence / Mortality: Cervical! cancer! is! the! fourth! most! common! cancer! in! women,! and! seventh! overall,!with!an!estimated!528,000!new!cases!in!2012.!Majority!of!the!global! burden!(around!85%)!occurs!in!the!less!developed!regions,!where!it!accounts! for! almost!12%! of!all!female!cancers.! HighErisk! regions,! with!estimated!Age! Standardised!Rate!(ASR)!of!over!30!per!100,000,!include:!Eastern!Africa!42.7;! Southern! Africa! 31.5;! Middle/Central! Africa! 30.6;! –! with! Western! Africa! on! the!border!line!of!high!risk!at!29.3.!(See!Fig.!1)! There!were!an!estimated!266,000!global!deaths!from!cervical!cancer!in!2012,! accounting!for!7.5%!of!all!female!cancer!deaths.!Almost!nine!out!of!ten!(87%)! cervical! cancer! deaths! occur! in! less! developed! regions.! Mortality! varies! 18E fold!between!different!regions!of!the!world,!with!rates!ranging!from!less!than! 2!per!100,000!in!Western!Asia,!Western!Europe!and!Australia/New!Zealand! to! more! than! 20! per! 100,000! in! Middle/Central! Africa! 22.2;! and! Eastern! Africa!27.6.!Western!Africa!is!not!far!behind!at!18.5.!!