Hemi-Implant Arthroplasty with Decompression And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Volume 15, Issue 1, January-April
Volume 15, Issue 1, January-April Osteochondral lesions of the talus in adults J. Batista, G. Joannas, L. Casola, L. Logioco, G. Arrondo 1A Traumatic lesion with isolated cartilage injury (flap) Tx: arthroscopy, curettage, and microfractures. 1B Traumatic lesion (cartilage and subchondral bone injury) 1B.1 Lesion <10mm in diameter and <5mm of depth (superficial lesion) Tx: arthroscopy, curettage, and microfractures. 1B.2 Lesion >10mm in diameter and >5mm in depth Tx: fragment fixation with osteosynthesis, open surgery, osteochondral graft, or mosaicoplasty. 2A Non-traumatic isolated bone injury, subchondral cyst. Tx: retrograde drilling. 2B Non-traumatic open subchondral bone cyst with articular connection (progression of type 2A). 2B.1 Lesion measuring <10mm in diameter and <5mm in depth (superficial lesion). Tx: arthroscopy, curettage, and microfractures. 2B.2 Lesion measuring >10mm in diameter and >5mm in depth. Tx: open surgery, osteochondral graft, or mosaicoplasty. 3 Type 1 or 2 lesions associated with lateral instability of the ankle Tx: ligament repair. 4 With limb deformities 4A Types 1 or 2 lesions with hindfoot deformity = varus or valgus calcaneus Tx: varus or valgus calcaneal osteotomy. 4B Type 1 or 2 lesion with supramalleolar deformity of distal tibia (varus or valgus) Tx: varus or valgus supramalleolar osteotomy. Tx: treatment. Volume 15, Issue 1, January-April The Journal of the Foot & Ankle (eISSN 2675-2980) is published quarterly in April, August, and December, with the purpose of disseminating papers on themes of Foot and Ankle Medicine and Surgery and related areas. The Journal offers free and open access to your content on our website. All papers are already published with active DOIs. -

Anterior Reconstruction Techniques for Cervical Spine Deformity
Neurospine 2020;17(3):534-542. Neurospine https://doi.org/10.14245/ns.2040380.190 pISSN 2586-6583 eISSN 2586-6591 Review Article Anterior Reconstruction Techniques Corresponding Author for Cervical Spine Deformity Samuel K. Cho 1,2 1 1 1 https://orcid.org/0000-0001-7511-2486 Murray Echt , Christopher Mikhail , Steven J. Girdler , Samuel K. Cho 1Department of Orthopedics, Icahn School of Medicine at Mount Sinai, New York, NY, USA Department of Orthopaedics, Icahn 2 Department of Neurological Surgery, Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, School of Medicine at Mount Sinai, 425 NY, USA West 59th Street, 5th Floor, New York, NY, USA E-mail: [email protected] Cervical spine deformity is an uncommon yet severely debilitating condition marked by its heterogeneity. Anterior reconstruction techniques represent a familiar approach with a range Received: June 24, 2020 of invasiveness and correction potential—including global or focal realignment in the sagit- Revised: August 5, 2020 tal and coronal planes. Meticulous preoperative planning is required to improve or prevent Accepted: August 17, 2020 neurologic deterioration and obtain satisfactory global spinal harmony. The ability to per- form anterior only reconstruction requires mobility of the opposite column to achieve cor- rection, unless a combined approach is planned. Anterior cervical discectomy and fusion has limited focal correction, but when applied over multiple levels there is a cumulative ef- fect with a correction of approximately 6° per level. Partial or complete corpectomy has the ability to correct sagittal deformity as well as decompress the spinal canal when there is an- terior compression behind the vertebral body. -
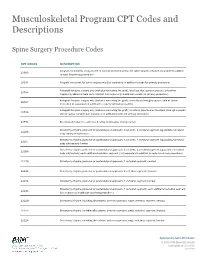
Musculoskeletal Program CPT Codes and Descriptions
Musculoskeletal Program CPT Codes and Descriptions Spine Surgery Procedure Codes CPT CODES DESCRIPTION Allograft, morselized, or placement of osteopromotive material, for spine surgery only (List separately in addition 20930 to code for primary procedure) 20931 Allograft, structural, for spine surgery only (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); local (eg, ribs, spinous process, or laminar 20936 fragments) obtained from same incision (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); morselized (through separate skin or fascial 20937 incision) (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); structural, bicortical or tricortical (through separate 20938 skin or fascial incision) (List separately in addition to code for primary procedure) 20974 Electrical stimulation to aid bone healing; noninvasive (nonoperative) Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22206 body subtraction); thoracic Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22207 body subtraction); lumbar Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22208 body subtraction); each additional vertebral segment (List separately in addition to code for -

Osteotomy Around the Knee: Evolution, Principles and Results
Knee Surg Sports Traumatol Arthrosc DOI 10.1007/s00167-012-2206-0 KNEE Osteotomy around the knee: evolution, principles and results J. O. Smith • A. J. Wilson • N. P. Thomas Received: 8 June 2012 / Accepted: 3 September 2012 Ó Springer-Verlag 2012 Abstract to other complex joint surface and meniscal cartilage Purpose This article summarises the history and evolu- surgery. tion of osteotomy around the knee, examining the changes Level of evidence V. in principles, operative technique and results over three distinct periods: Historical (pre 1940), Modern Early Years Keywords Tibia Osteotomy Knee Evolution Á Á Á Á (1940–2000) and Modern Later Years (2000–Present). We History Results Principles Á Á aim to place the technique in historical context and to demonstrate its evolution into a validated procedure with beneficial outcomes whose use can be justified for specific Introduction indications. Materials and methods A thorough literature review was The concept of osteotomy for the treatment of limb defor- performed to identify the important steps in the develop- mity has been in existence for more than 2,000 years, and ment of osteotomy around the knee. more recently pain has become an additional indication. Results The indications and surgical technique for knee The basic principle of osteotomy (osteo = bone, tomy = osteotomy have never been standardised, and historically, cut) is to induce a surgical transection of a bone to allow the results were unpredictable and at times poor. These realignment and a consequent transfer of weight bearing factors, combined with the success of knee arthroplasty from a damaged area to an undamaged area of joint surface. -

Periacetabular Osteotomy (PAO) of the Hip
UW HEALTH SPORTS REHABILITATION Rehabilitation Guidelines For Periacetabular Osteotomy (PAO) Of The Hip The hip joint is composed of the femur (the thigh bone) and the Lunate surface of acetabulum acetabulum (the socket formed Articular cartilage by the three pelvic bones). The Anterior superior iliac spine hip joint is a ball and socket joint Head of femur Anterior inferior iliac spine that not only allows flexion and extension, but also rotation of the Iliopubic eminence Acetabular labrum thigh and leg (Fig 1). The head of Greater trochanter (fibrocartilainous) the femur is encased by the bony Fat in acetabular fossa socket in addition to a strong, (covered by synovial) Neck of femur non-compliant joint capsule, Obturator artery making the hip an extremely Anterior branch of stable joint. Because the hip is Intertrochanteric line obturator artery responsible for transmitting the Posterior branch of weight of the upper body to the obturator artery lower extremities and the forces of Obturator membrane Ischial tuberosity weight bearing from the foot back Round ligament Acetabular artery up through the pelvis, the joint (ligamentum capitis) Lesser trochanter Transverse is subjected to substantial forces acetabular ligament (Fig 2). Walking transmits 1.3 to Figure 1 Hip joint (opened) lateral view 5.8 times body weight through the joint and running and jumping can generate forces across the joint fully form, the result can be hip that is shared by the whole hip, equal to 6 to 8 times body weight. dysplasia. This causes the hip joint including joint surfaces and the to experience load that is poorly previously-mentioned acetabular The labrum is a circular, tolerated over time, resulting in labrum. -

What Is the Impact of a Previous Femoral Osteotomy on THA?
Clin Orthop Relat Res (2019) 477:1176-1187 DOI 10.1097/CORR.0000000000000659 2018 Bernese Hip Symposium What Is the Impact of a Previous Femoral Osteotomy on THA? A Systematic Review Enrico Gallazzi MD, Ilaria Morelli MD, Giuseppe Peretti MD, Luigi Zagra MD 02/11/2020 on BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD30p/TQ0kcqx8yGZO9yTf1dd5lN9ZPVa7AUCC2fdK0Vq4= by https://journals.lww.com/clinorthop from Downloaded Downloaded from Received: 10 August 2018 / Accepted: 8 January 2019 / Published online: 17 April 2019 https://journals.lww.com/clinorthop Copyright © 2019 by the Association of Bone and Joint Surgeons Abstract by Background Femoral osteotomies have been widely used Questions/purposes In this systematic review, we asked: BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD30p/TQ0kcqx8yGZO9yTf1dd5lN9ZPVa7AUCC2fdK0Vq4= to treat a wide range of developmental and degenerative hip (1) What are the most common complications after THA in diseases. For this purpose, different types of proximal fe- patients who have undergone femoral osteotomy, and how mur osteotomies were developed: at the neck as well as at frequently do those complications occur? (2) What is the the trochanteric, intertrochanteric, or subtrochanteric lev- survival of THA after previous femoral osteotomy? (3) Is els. Few studies have evaluated the impact of a previous the timing of hardware removal associated with THA femoral osteotomy on a THA; thus, whether and how a complications and survivorship? previous femoral osteotomy affects the -

Ankle Injuries
Pediatric Fractures of the Ankle Nicholas Frane DO Zucker/Hofstra School of Medicine Northwell Health Core Curriculum V5 Disclosure • Radiographic Images Courtesy of: Dr. Jon-Paul Dimauro M.D or Christopher D Souder, MD, unless otherwise specified Core Curriculum V5 Outline • Epidemiology • Anatomy • Classification • Assessment • Treatment • Outcomes Core Curriculum V5 Epidemiology • Distal tibial & fibular physeal injuries 25%-38% of all physeal fractures • Ankle is the 2nd most common site of physeal Injury in children • Most common mechanism of injury Sports • 58% of physeal ankle fractures occur during sports activities • M>F • Commonly seen in 8-15y/o Hynes D, O'Brien T. Growth disturbance lines after injury of the distal tibial physis. Their significance in prognosis. J Bone Joint Surg Br. 1988;70:231–233 Zaricznyj B, Shattuck LJ, Mast TA, et al. Sports-related injuries in school-aged children. Am J Sports Med. 1980;8:318–324. Core Curriculum V5 Epidemiology Parikh SN, Mehlman CT. The Community Orthopaedic Surgeon Taking Trauma Call: Pediatric Ankle Fracture Pearls and Pitfalls. J Orthop Trauma. 2017;31 Suppl 6:S27-S31. doi:10.1097/BOT.0000000000001014 Spiegel P, et al. Epiphyseal fractures of the distal ends of the tibia and fibula. J Bone Joint Surg Am. 1978;60(8):1046-50. Core Curriculum V5 Anatomy • Ligamentous structures attach distal to the physis • Growth plate injury more likely than ligament failure secondary to tensile weakness in physis • Syndesmosis • Anterior Tibio-fibular ligament (AITFL) • Posterior Inferior Tibio-fibular -

Total Knee Arthroplasty After Osteotomies Around the Knee
Review Article Page 1 of 5 Total knee arthroplasty after osteotomies around the knee Salvatore Risitano, Alessandro Bistolfi, Luigi Sabatini, Fabrizio Galetto, Alessandro Massè Department of Orthopedics and Traumatology, Città della Salute e della Scienza, CTO Hospital, Turin 10126, Italy Contributions: (I) Conception and design: A Bistolfi, L Sabatini; (II) Administrative support: None; (III) Provision of study materials or patients: None; (IV) Collection and assembly of data: S Risitano, F Galetto; (V) Data analysis and interpretation: A Bistolfi, S Risitano; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Salvatore Risitano, MD. via Zuretti 29, Turin 10126, Italy. Email: [email protected]. Abstract: Osteotomies around the knee are procedures that have shown excellent results to treat unicompartmental arthritis delaying the need for knee replacement. Despite the good results, benefits generally deteriorate with time leading to a total knee arthroplasty (TKA) for progression of osteoarthritis and involvement of the other compartments. Conversion of osteotomy to TKA is more surgically demanding compared with a primary prosthesis; in this paper, we analyze surgical difficulties that surgeons can found to perform TKA after an osteotomy around the knee; according to the literature we analyze surgical steps that can differ from standard primary surgery, including skin incision, hardware removal, residual tibial and femoral deformities and balancing of soft tissue. Keywords: Total knee arthroplasty (TKA); high tibial osteotomy (HTO); femoral osteotomy Received: 29 March 2017; Accepted: 07 April 2017; Published: 31 May 2017. doi: 10.21037/aoj.2017.05.11 View this article at: http://dx.doi.org/10.21037/aoj.2017.05.11 Introduction Surgical incision Osteotomies around the knee are procedures that have The knee joint is vulnerable to multiple parallel incision and shown excellent results to treat unicompartmental arthritis skin necrosis is an important issue in this surgery. -

Kyphoplasty/Vertebroplasty, Thoracic Spine
Musculoskeletal Surgical Services: Spine Fusion/Stabilization Surgery; Kyphoplasty/Vertebroplasty, Thoracic Spine POLICY INITIATED: 06/30/2019 MOST RECENT REVIEW: 06/30/2019 POLICY # HH-5641 Overview Statement The purpose of these clinical guidelines is to assist healthcare professionals in selecting the medical service that may be appropriate and supported by evidence to improve patient outcomes. These clinical guidelines neither preempt clinical judgment of trained professionals nor advise anyone on how to practice medicine. The healthcare professionals are responsible for all clinical decisions based on their assessment. These clinical guidelines do not provide authorization, certification, explanation of benefits, or guarantee of payment, nor do they substitute for, or constitute, medical advice. Federal and State law, as well as member benefit contract language, including definitions and specific contract provisions/exclusions, take precedence over clinical guidelines and must be considered first when determining eligibility for coverage. All final determinations on coverage and payment are the responsibility of the health plan. Nothing contained within this document can be interpreted to mean otherwise. Medical information is constantly evolving, and HealthHelp reserves the right to review and update these clinical guidelines periodically. No part of this publication may be reproduced, stored in a retrieval system or transmitted, in any form or by any means, electronic, mechanical, photocopying, or otherwise, without permission -

Patient Information for Knee Osteotomy Surgery
Patient information for knee osteotomy surgery Introduction Osteoarthritis (‘wear and tear’) of the knee joint is common and can cause considerable pain and sometimes deformity of the joint. Normally when we are walking or standing, the weight goes through the centre of our knee. Unfortunately, when wear and tear affects one side of the joint, it can cause a bow leg or a knock knee. When this happens the weight is taken by the worn part of the joint, which can become more and more painful over time. This can be seen when looking at the x-rays below. On the left the weight is going through the centre of the knees and on the right it is going through the inner part of the knees, which are worn with bow legs. Normal alignment Knock knees Page 1 of 4 Treatment Early treatment can involve the use of painkillers, physical therapy, injections and weight loss, but when these options no longer control the pain adequately, a major surgical procedure may be required. Often, it is a joint replacement that is required, but this can sometimes be regarded as a risk in a young and relatively active patient due to concerns that the joint replacement may ‘wear out’ in the future, needing further surgery. Osteotomy surgery is an option that can be used instead of performing a joint replacement, particularly when the wear and tear is confined to only one side of the knee joint. The principle is that the leg is re-aligned so that more weight goes through the good side of the knee rather than the bad side that has the wear and tear. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Dega Osteotomy (Pelvic Osteotomy)
Dega Osteotomy (Pelvic Osteotomy) Why does my child need this surgery? The hip joint is a ball-and-socket joint that joins the thighbone (femur) to the pelvis. The femoral head, a bony ball at the top of the femur, rotates (turns) inside the pelvic socket (acetabulum). In a child with very tight muscle tone (spasticity), the muscles around the femur can begin pulling the ball out of the socket. For children who walk, the weight of the pelvis may help hold the joint together. A child whose pelvic socket is deep and in good condition may need a femoral derotational osteotomy. This surgery repositions the ball of the femur in the pelvic socket. Sometimes a child’s pelvic socket becomes too shallow to hold the femoral ball. They may need a Dega osteotomy and a femoral derotational osteotomy. Together, the two What happens after surgery? procedures repair the socket, reposition the ball of the femur Your child will probably not be in a cast. A bandage will and make the hip joint stable again. Both procedures will cover the incision. The doctor may use a soft wedge pillow to most likely happen during the same surgery session. They keep the legs spread so the hips can heal in the right position. will probably be combined with a procedure to relax tight Most children are out of the hospital in four to five days. muscles around the hips. The Dega osteotomy is named This includes children who have more than one procedure at for the physician who first wrote about it.